Abstract
Pneumothorax is the most urgent cause of a hyperlucent thorax. Pneumothorax has a variety of causes ranging from trauma to rupture of pulmonary cavities, cysts, or bullae into the lungs. Hyperlucent lungs result from air trapping or decreased pulmonary vasculature. Emphysema causes both over inflation and decreased pulmonary vasculature. Emphysema is a bilateral disease, but it often appears asymmetric, especially when the patient has large bullae. Swyer-James syndrome was originally described as a unilateral hyperlucent lung that resulted from constrictive bronchiolitis. High resolution computed tomography of patients with constrictive bronchiolitis reveals multiple areas of air trapping that are described as mosaic attenuation and are usually bilateral but asymmetric enough to account for the unilateral appearance on the chest x-ray. Obstruction of large bronchi most often causes loss of lung volume with atelectasis, but there are rare causes where collateral air drift permits overinflation of the lung distal to the obstruction. Pulmonary embolism decreases pulmonary blood flow, but the decreased perfusion is infrequently detected on the chest x-ray.
Keywords
bronchial atresia, bullae, constrictive bronchiolitis, emphysema, pneumothorax, pulmonary embolism, Swyer-James syndrome
Questions
- 1.
Match the abnormal thoracic lucencies seen in Fig. 22.1, A to C , with the following diagnoses.
____ Bilateral pneumothorax.
____ Bullous emphysema.
____ Ruptured subpleural bullae with pneumothorax.

Fig. 22.1
- 2.
Asymmetric air trapping may be confirmed by which of the following radiographic techniques?
- a.
Lateral decubitus view.
- b.
Forced inspiratory view.
- c.
Forced expiratory view.
- d.
Overpenetrated view.
- e.
Oblique view.
- a.
- 3.
Mosaic attenuation on high-resolution computed tomography (HRCT) is a common finding in patients with which one of the following diagnoses?
- a.
Constrictive bronchiolitis.
- b.
Pulmonary embolism.
- c.
Panacinar emphysema.
- d.
Centrilobular emphysema.
- e.
Asthma.
- a.
Discussion
The first step in the evaluation of the apparently hyperlucent lung ( Chart 22.1 ) is to check on radiologic technique. A high-contrast, low-kilovoltage (low-kVp) technique may result in a high-contrast chest film and thus obscure the normal vascular markings of the lung, leading to the false impression of hyperlucent lungs. Such highly contrasted radiographs are readily identified by the marked contrast between the soft tissue opacities and the lucency of the lung. This is a particularly common problem with the portable examination, for which high-kVp techniques are more difficult to obtain. The radiologic technique may also result in the appearance of a unilateral hyperlucent lung when the patient is rotated. Rotation produces the unilateral hyperlucent appearance by projecting soft tissues over one side of the chest while rotating the soft tissues off the opposite side of the chest. This latter problem is particularly noticeable in female patients with large pendulous breasts, which add considerably to the opacity over the lower lung fields. Improper centering of the radiographic beam may also cause asymmetric exposure.
- I.
Bilateral
- A.
Faulty radiologic technique (overpenetrated examination)
- B.
Thin body habitus
- C.
Bilateral mastectomy
- D.
Right-to-left cardiac shunts (e.g., tetralogy of Fallot, pseudotruncus arteriosus, truncus type IV)
- E.
Pulmonary embolism 396
- F.
Emphysema 169 , 174 , 593 , 594
- G.
Acute asthmatic attack 175
- H.
Acute bronchiolitis (usually in pediatric patients)
- I.
Interstitial emphysema 649
- A.
- II.
Unilateral
- A.
Mastectomy
- B.
Absent pectoralis muscles
- C.
Faulty radiologic technique, including rotation of patient
- D.
Extrapulmonary air collections (e.g., pneumothorax, mediastinal emphysema, subcutaneous emphysema)
- E.
Pulmonary embolism (acute or chronic) 660
- F.
Emphysema (particularly bullous emphysema) 235
- G.
Atrophy of trapezius muscle (after radical neck dissection) 568
- H.
Bronchial obstruction
- 1.
Neoplastic
- a.
Bronchogenic carcinoma (rare)
- b.
Metastatic (rare, but most common primary tumors are breast, thyroid, pancreas, colon, melanoma) 36
- a.
- 2.
Granulomatous masses, including broncholith
- 3.
Bronchial stenosis with mucocele 574
- 4.
Foreign body (common in children)
- 1.
- J.
Hilar mass (e.g., adenopathy, bronchogenic cyst)
- K.
Constrictive bronchiolitis (Swyer-James, or MacLeod, syndrome)
- L.
Compensatory overaeration
- M.
Congenital lobar overdistension
- N.
Cardiomegaly (left lower lobe)
- A.
Anatomic variations also result in the appearance of hyperlucent lungs. The best-known example is the patient with a very thin body habitus, which results in an overpenetrated chest radiograph. Asymmetric absence of soft tissues can likewise result in unilateral hyperlucent lungs. Radical mastectomy is the most common source of this problem. Rarely, congenital asymmetry of the chest wall results in a similar appearance. This is noted in patients who have hypoplastic or absent pectoralis muscles.
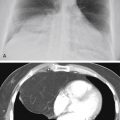
Extrapulmonary air collections, including subcutaneous emphysema, mediastinal emphysema, and pneumothoraces (see Fig. 22.1, B and C ), produce lucent abnormalities that are usually recognized on the basis of their location and are not usually confused with hyperlucent lungs. Most of these conditions result in differences in the opacity of the lung because of overlying soft tissues or their absence. It is important to remember that the radiologic opacity of the normal lung is produced by the pulmonary vascularity. The pulmonary vessels are radiologically identifiable because they contain blood, which is of soft tissue opacity, and are surrounded by air. Therefore, any loss of opacity of the lung reflects a change in the pulmonary vascularity. This should be detected by noting diminution in the size and number of radiologically identifiable vessels ( Fig. 22.2 ). The size and number of radiologically visible vessels are directly related to pulmonary blood flow, supporting the observation that a truly hyperlucent lung is a reflection of decreased blood flow through the lung. This may be the result of cardiac or primary pulmonary disease.

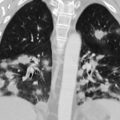
Emphysema
Emphysema is a very important cause of loss of pulmonary vascularity (see Fig. 22.1, A ). 169 , 174 Severe cases of emphysema will produce marked attenuation and stretching of pulmonary vessels. This process may be diffuse to such an extent that there may even be nearly complete absence of vessels. The diagnosis of emphysema by evaluation of the pulmonary vascularity requires a subjective evaluation of the vascular patterns. Thurlbeck and Simon 594 evaluated 700 patients in an effort to correlate paper-mounted, whole-lung sections with posteroanterior and lateral view roentgenograms to determine the accuracy of the radiologic diagnosis of emphysema. They measured lung length and width, size of the retrosternal clear space, heart size, and position of the diaphragm. They observed that lung length and the size of the retrosternal clear space increased, the level of the diaphragm was lowered, the heart size decreased, and the lung width was unchanged as the emphysema became more severe. They believed that lung length and diaphragm level were the most discriminating measurements for diagnostic accuracy, followed by size of the retrosternal clear space. However, they identified no combination of these radiologic variables that identified emphysema better than the subjective diagnosis of the disease based on arterial deficiency. They also emphasized that radiologic lung dimensions are related to stature and must therefore be interpreted cautiously. For example, kyphosis of the thoracic spine causes an increase in the anteroposterior diameter of the chest. They further divided vascular patterns into three main categories of abnormality: (1) the vessels are present but narrowed in most of the lung; (2) there is a normal axial pathway but fewer side branches; and (3) there may be complete absence of vessels. While these vascular alterations may be subtle on chest radiograph, HRCT is very sensitive for the detection of variations in regional perfusion and detection of emphysema ( Fig. 22.3, A and B ).