Abstract
The proximal right and left pulmonary arteries and proximal bronchi account for the appearance of the hila on the chest x-ray, but the arteries are crossed by the pulmonary veins. Multiple small lymph nodes are in the hila but are not visible on the chest x-ray. Enlargement of the hila may result from vascular or nodal enlargement. The first step in evaluation of hilar enlargement is to distinguish enlarged vessels from lymph nodes. Enlarged vessels maintain the vascular contour and are often associated with main pulmonary artery and right heart enlargement, confirming the diagnosis of pulmonary artery hypertension. Lymph nodes have a more lobulated appearance and are often associated with enlarged mediastinal nodes. There are a number of benign and malignant causes of hilar adenopathy, which are reviewed in this chapter. Proximal primary lung cancers are most often squamous or small cell tumors.
Keywords
bronchogenic cyst, lung cancer, lymphoma, metastases, postcapillary and precapillary pulmonary hypertension, tuberculosis
Questions
- 1.
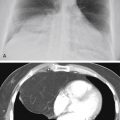
The most likely cause of unilateral hilar enlargement in the adult in Fig. 11.1, A-C , is:
- a.
Bronchogenic cyst.
- b.
Lung cancer.
- c.
Large right pulmonary artery.
- d.
Pulmonary varix.
- e.
Aneurysm of the descending aorta.

Fig. 11.1
- a.
- 2.
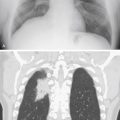
The most likely cause of the bilateral hilar enlargement in the asymptomatic young adult in Fig. 11.2 is:
- a.
Metastasis.
- b.
Primary tuberculosis.
- c.
Sarcoidosis.
- d.
Lymphoma.
- e.
Histoplasmosis.

Fig. 11.2
- a.
Discussion
The first problem in the evaluation of hilar enlargement is the distinction of vascular enlargement from hilar masses. 73 The normal hilar contours are formed by the pulmonary arteries. Distinction of enlarged pulmonary arteries from hilar masses often requires careful analysis, followed by computed tomography (CT) scanning for confirmation. In cases with bilateral hilar enlargement, it may be especially difficult to distinguish vascular enlargement from masses. Unilateral hilar enlargement also requires careful evaluation but is more suggestive of a mass. In addition to changes in the contour of the hilum, the finding of added opacity strongly suggests a mass. For precise localization to the hilum, it is important to note whether the increased opacity blends imperceptibly with the normal pulmonary artery shadows and thus obscures their borders, or whether the pulmonary arteries are easily identified in addition to the suspected opacity. When the borders of the pulmonary arteries are clearly identifiable, it must be assumed that the mass is discrete and either anterior or posterior to the hilum. The contour of the pulmonary artery is visible because of the adjacent aerated lung. When the aerated lung is filled or displaced, the border of the pulmonary artery will no longer be detected. An area of increased opacity anterior or posterior to the hilum has no effect on the air adjacent to the pulmonary artery and therefore has no effect on its visibility. Felson 150 has described this phenomenon as the hilum overlay sign ( Fig 11.3, A-C ). This is very useful for separating true hilar abnormalities from superimposed anterior or posterior opacities. In such cases, the lateral view is usually adequate for verifying that the abnormality is not in the hilum. This separation is easily accomplished with CT scanning.

Once it has been ascertained that a hilum is abnormal, the next step in evaluating hilar enlargement is to determine whether the abnormal hilum is the result of an enlarged vascular structure or a mass ( Chart 11.1 ). This requires detailed understanding of the anatomy of the hilum in at least the posteroanterior (PA) and lateral projections ( Fig 11.4, A and B ). As noted earlier, the hilar shadows in both projections are produced mainly by the right and left pulmonary arteries. The left pulmonary artery is very characteristic in its appearance on the PA chest radiograph, creating an opacity above the left mainstem bronchus and continuing as an opacity that appears to be lateral to the large bronchi.
- I.
Large pulmonary arteries
- A.
Postcapillary pulmonary arterial hypertension
- 1.
Left-sided heart failure
- 2.
Mitral stenosis 75
- 3.
Left atrial myxoma
- 4.
Pulmonary veno-occlusive 529
- 5.
Mediastinal fibrosis
- 1.
- B.
Precapillary pulmonary arterial hypertension
- 1.
Emphysema 368 (see Chapter 22 )
- 2.
Chronic interstitial lung disease (see Chapter 19 )
- 3.
Cystic fibrosis
- 4.
Pulmonary embolism (acute and chronic) 65 , 637
- 5.
Portal hypertension 71
- 6.
Metastatic tumor emboli
- 7.
Cardiac shunts
- a.
Ventricular septal defect (VSD)
- b.
Atrial septal defect (ASD)
- c.
Patent ductus arteriosus
- d.
Truncus arteriosus
- e.
Transposition of great vessels
- a.
- 8.
Primary pulmonary hypertension 607
- 1.
- C.
Pulmonary artery aneurysms 66 (septic emboli in intravenous drug users, Takayasu disease, Behçet disease)
- A.
- II.
Unilateral hilar mass
- A.
Neoplasm
- B.
- C.
Bronchial carcinoid 275
- D.
Metastasis 379
- E.
Lymphoma
- F.
Inflammation
- 1.
- 2.
Nontuberculous mycobacteria 389
- 3.
Fungal infection (histoplasmosis, 97 coccidioidomycosis, 373 blastomycosis, 450 infrequently in cryptococcosis) 200 , 346
- 4.
Viral infections (atypical measles)
- 5.
Infectious mononucleosis (rare) 248
- 6.
Acquired immune deficiency syndrome 314
- 7.
Drug reactions 236 , 503 (phenytoin [Dilantin])
- 8.
Sarcoidosis (infrequent)
- 9.
Bacterial lung abscess 482
- 1.
- A.
- III.
Bilateral hilar masses
- A.
Neoplasm
- 1.
Lymphoma
- 2.
Leukemia (chronic lymphocytic leukemia)
- 3.
Metastases 107
- 4.
Lung cancer (usually asymmetric)
- 1.
- B.
Inflammation
- 1.
- 2.
Occupational diseases (silicosis and coal worker’s pneumoconiosis)
- 3.
Inhalational anthrax 125
- 1.
- C.
Collagen vascular diseases
- 1.
Lupus (rare)
- 2.
Polyarteritis nodosa
- 3.
Mixed
- 1.
- A.
- IV.
Duplication cysts (bronchogenic cysts) 463