Abstract
Anterior mediastinal masses are detectable on chest x-rays when they distort the normal mediastinal contours or fill the retrosternal clear space on the lateral view. CT is often required for detection and may provide specific diagnostic features or important staging information. A variety of anterior mediastinal masses are often related to normal structures including thymus, thyroid, lymph nodes, and vascular structures.
Keywords
ascending aortic aneurysm, cystic hygroma, epicardial fat, germ cell tumors, lymphoma, metastases, Morgagni hernia, pericardial cyst, thymoma, thyroid masses
Questions
- 1.
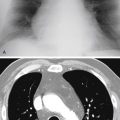
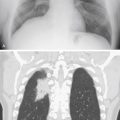
Which one of the following diagnoses is most likely in a middle-aged adult with the chest radiographs and computed tomography (CT) scan shown in Fig. 9.1, A-C ?
- a.
Goiter.
- b.
Thymoma.
- c.
Germ cell tumor.
- d.
Cystic hygroma.
- e.
Pericardial cyst.

Fig. 9.1
- a.
- 2.
Which one of the following tumors is most likely to spread contiguously and is unlikely to metastasize to distant sites?
- a.
Thymoma.
- b.
Thyroid carcinoma.
- c.
Germ cell tumor.
- d.
Lymphoma.
- e.
Thymic carcinoma.
- a.
- 3.
Which one of the following is least likely to calcify?
- a.
Substernal thyroid.
- b.
Thymic cyst.
- c.
Thymoma.
- d.
Germ cell tumor.
- e.
Treated lymphoma.
- a.
Discussion
The anterior mediastinum contains the thymus, lymph nodes, vessels, and fat ( Chart 9.1 ). There is considerable variation in the normal width of the mediastinum on the posterior-anterior (PA) chest radiograph and in the size and opacity of the retrosternal clear space on the lateral view. 323 These variations result from differences in the shape and size of vessels and fat content. When there is minimal anterior fat, both lungs extend in front of the ascending aorta, pressing all four layers of pleura together to form the anterior junction line. Masses are visible on the PA and lateral views when they displace the mediastinal pleura and alter the normal mediastinal contour. Visibility is mainly determined by the interface of the mass with the aerated lung, but soft-tissue masses that are surrounded by fat may appear as minimally visible opacities that require CT for confirmation.
- I.
Thymic lesions 178
- A.
Thymoma (benign and invasive) 509 , 567 , 600
- B.
Thymic cyst 276
- C.
- D.
Lymphoma
- E.
Thymic hyperplasia 413
- F.
Thymic carcinoid tumor 413 , 567
- G.
Thymic carcinoma 567
- A.
- II.
Germ cell tumors 486
- A.
Dermoid cyst (mature cystic teratoma) 276
- B.
Teratoma (benign and malignant) 486 , 582
- C.
Embryonal cell carcinoma
- D.
Choriocarcinoma
- E.
Seminoma
- F.
Mixed germ cell tumor 486
- A.
- III.
Thyroid
- A.
Goiter
- B.
Adenoma
- C.
Carcinoma
- A.
- IV.
Lymph nodes 67
- A.
Lymphoma (both Hodgkin and non-Hodgkin) 21
- B.
Metastases
- C.
Benign lymph node hyperplasia
- D.
Angioblastic lymphoid adenopathy
- E.
Sarcoidosis and granulomatous infections (rare)
- A.
- V.
Cardiovascular
- A.
Epicardial fat pad
- B.
Aneurysm of ascending aorta 548
- C.
Aneurysm of sinus of Valsalva 418 , 470
- D.
Dilated superior vena cava
- E.
Pericardial cyst 148
- F.
Cardiac tumors
- G.
Traumatic pseudoaneurysm of ascending aorta
- A.
- VI.
Cysts
- A.
Cystic hygroma (lymphangioma)
- B.
Bronchogenic cyst
- C.
Extralobar sequestration
- D.
Thymic and germ cell lesions (see above)
- A.
- VII.
Other
- A.
Neural tumors of vagus or phrenic nerves 459
- B.
Paraganglioma (chemodectoma and pheochromocytoma) 459
- C.
Hernia of the foramen of Morgagni 183
- D.
Parathyroid adenoma, 525 adenocarcinoma
- E.
Primary bone tumors and metastases to the sternum
- F.
Lipoma, 183 , 195 lipomatosis 339
- G.
Hemangioma 145
- H.
Pancreatic pseudocyst 302
- A.
Once the presence of a mediastinal mass has been confirmed, precise localization of the mass is the most important aspect of radiologic evaluation. Strict anatomic divisions of the mediastinum are not easily translated to the lateral chest radiograph. Anatomy texts have divided the mediastinum into four compartments: superior, anterior, middle, and posterior. When this division is applied to the lateral chest radiograph, the radiologist should consider a fifth compartment corresponding anatomically to the posterior gutter, which includes the paravertebral soft tissues. These anatomic divisions of the mediastinal compartments were established before the development of chest radiology. Felson 150 was one of the first to recognize the cumbersome nature of applying anatomic definitions to the lateral chest radiograph and devised a simplified method based on easily identifiable radiologic landmarks. He divided the anterior and middle compartments by drawing a line from the intersection of the anterior border of the trachea with the sternum to intersect the diaphragm. This line follows the posterior border of the heart and the inferior vena cava. A second line, 1 cm posterior to the anterior border of the vertebral bodies, was used to separate the middle from the posterior mediastinum ( Fig. 9.2 ). This method of dividing the mediastinum is not anatomically precise, but it is much less cumbersome to apply to the lateral chest radiograph, and provides the radiologist with a starting point in the evaluation of mediastinal masses. CT permits more precise anatomic localization and reveals the relationship of the mass to normal anatomic structures. 631