Functional imaging offers information more sensitive to changes in lung structure and function. Hyperpolarized helium ( 3 He) and xenon ( 129 Xe) MR imaging of the lungs provides sensitive contrast mechanisms to probe changes in pulmonary ventilation, microstructure, and gas exchange. Gas imaging has shifted to the use of 129 Xe. Xenon is well-tolerated. 129 Xe is soluble in pulmonary tissue, which allows exploring specific lung function characteristics involved in gas exchange and alveolar oxygenation. Hyperpolarized gases and 129 Xe in particular stand to be an excellent probe of pulmonary structure and function, and provide sensitive and noninvasive biomarkers for pulmonary diseases.
Key points
- •
Hyperpolarized (HP) helium ( 3 He) and xenon ( 129 Xe) MR imaging of the lungs provides sensitive contrast mechanisms to probe changes in pulmonary ventilation, microstructure, and gas exchange.
- •
Recent scarcity in the supply of 3 He shifted the field of HP gas imaging to the use of less expensive and naturally available 129 Xe.
- •
129 Xe has been shown to be well-tolerated in healthy volunteers and patients with various pulmonary diseases.
- •
Current technology allows 129 Xe to be imaged 3-dimensionally in all 3 compartments of the lung (airspace, barrier, red blood cells) and provides a new view of pulmonary gas exchange.
Introduction
Lung diseases affect the conducting airways, the gas exchange parenchyma, or both. As a result, they have a high impact on patients’ morbidity, and quality of life. Chronic obstructive pulmonary disease (COPD), for example, is an umbrella term for progressive and irreversible obstructive diseases that affect the airways as well as the parenchyma. After cardiovascular diseases and cancer, COPD is predicted to be the third leading cause of death in the United States. Similarly, airway diseases such as asthma have a high prevalence and a large economic impact with $56 billion in associated health care costs. Furthermore, interstitial lung diseases, although less prevalent than COPD or asthma, also have a high morbidity. This morbidity is partially attributable to a lack of viable therapeutic options to treat the underlying diseases. However, equally problematic is the lack of sensitive biomarkers that can be used to diagnose these diseases earlier, better monitor progression, and show early therapeutic response.
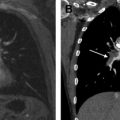
The current gold standard for diagnosis and monitoring treatment of pulmonary diseases is spirometric pulmonary function testing (PFTs). However, by assessing the lung only on a global basis, PFT metrics generally lack the ability to detect functional changes associated with the small airways and gas exchange regions. This insensitivity of PFTs to the functioning of the distal lung parenchyma ( Fig. 1 ) has led these regions to be referred to as the ‘silent zone.’ Additionally, these metrics largely rely on subject effort, causing significant measurement uncertainty and variability. Hence, current therapy is guided largely by patients’ symptoms and survival. Given the large burden on our health care system and the growing prevalence of pulmonary disease, there exists a need for improved diagnostic tools and quantitative metrics to better diagnose and quantify pulmonary disease progression and help to accurately measure response to therapy.
To overcome the lungs’ many compensatory mechanisms and improve sensitivity to early disease, it is necessary to exploit regional information obtained by imaging. To this end, hyperpolarized (HP) gas MR imaging provides a noninvasive, ionizing radiation–free method to image pulmonary structure and function. Although the early days of HP gas MR imaging saw extensive development and progress using the noble gas 3 He, its recent scarcity and concomitant increase in price (∼$2000/L) has caused a transition to the less expensive and naturally available 129 Xe (∼$30/L, natural abundance). An added advantage of 129 Xe is obtained by virtue of its solubility in pulmonary tissues, which leads to 2 signal sources, distinct from the xenon in the airspaces. 129 Xe can be detected separately in the pulmonary barrier tissues and the red blood cells (RBCs) in the capillary network, compartments in which it exhibits distinct resonant signal frequencies. These 3 129 Xe resonances can provide quantitative regional information on the fundamental function of the lung, gas exchange.
This article briefly touches on the history of HP gas MR imaging, describes the key technical properties, and discusses current and future applications and opportunities for pulmonary imaging.
Introduction
Lung diseases affect the conducting airways, the gas exchange parenchyma, or both. As a result, they have a high impact on patients’ morbidity, and quality of life. Chronic obstructive pulmonary disease (COPD), for example, is an umbrella term for progressive and irreversible obstructive diseases that affect the airways as well as the parenchyma. After cardiovascular diseases and cancer, COPD is predicted to be the third leading cause of death in the United States. Similarly, airway diseases such as asthma have a high prevalence and a large economic impact with $56 billion in associated health care costs. Furthermore, interstitial lung diseases, although less prevalent than COPD or asthma, also have a high morbidity. This morbidity is partially attributable to a lack of viable therapeutic options to treat the underlying diseases. However, equally problematic is the lack of sensitive biomarkers that can be used to diagnose these diseases earlier, better monitor progression, and show early therapeutic response.
The current gold standard for diagnosis and monitoring treatment of pulmonary diseases is spirometric pulmonary function testing (PFTs). However, by assessing the lung only on a global basis, PFT metrics generally lack the ability to detect functional changes associated with the small airways and gas exchange regions. This insensitivity of PFTs to the functioning of the distal lung parenchyma ( Fig. 1 ) has led these regions to be referred to as the ‘silent zone.’ Additionally, these metrics largely rely on subject effort, causing significant measurement uncertainty and variability. Hence, current therapy is guided largely by patients’ symptoms and survival. Given the large burden on our health care system and the growing prevalence of pulmonary disease, there exists a need for improved diagnostic tools and quantitative metrics to better diagnose and quantify pulmonary disease progression and help to accurately measure response to therapy.
To overcome the lungs’ many compensatory mechanisms and improve sensitivity to early disease, it is necessary to exploit regional information obtained by imaging. To this end, hyperpolarized (HP) gas MR imaging provides a noninvasive, ionizing radiation–free method to image pulmonary structure and function. Although the early days of HP gas MR imaging saw extensive development and progress using the noble gas 3 He, its recent scarcity and concomitant increase in price (∼$2000/L) has caused a transition to the less expensive and naturally available 129 Xe (∼$30/L, natural abundance). An added advantage of 129 Xe is obtained by virtue of its solubility in pulmonary tissues, which leads to 2 signal sources, distinct from the xenon in the airspaces. 129 Xe can be detected separately in the pulmonary barrier tissues and the red blood cells (RBCs) in the capillary network, compartments in which it exhibits distinct resonant signal frequencies. These 3 129 Xe resonances can provide quantitative regional information on the fundamental function of the lung, gas exchange.
This article briefly touches on the history of HP gas MR imaging, describes the key technical properties, and discusses current and future applications and opportunities for pulmonary imaging.
History and safety
In 1994, the first HP gas MR imaging studies were carried out ex vivo using the noble gas isotope 129 xenon ( 129 Xe). In 1997, Mugler and colleagues used 129 Xe to conduct the first ground breaking studies in humans. Although this represented a rapid advancement from mouse to clinical translation, these studies were limited by relatively low 129 Xe polarization (1%–2%), which resulted in low signal intensities. This limitation caused research interest to transition quickly to the other stable inert gas isotope. 3 He, which has a larger gyromagnetic ratio than 129 Xe (32.4 MHz/T vs 11.77 MHz/T), offered a simpler and more mature polarization technology (∼30%), and corresponding larger signal intensities. Additionally, unlike 129 Xe that, in large enough alveolar concentrations (>70%), is known to exhibit anesthetic properties, 3 He does not have any physiologic side effects, and was considered to be a better starting point for clinical imaging. Indeed, the known anesthetic properties of xenon led to it being regulated as a drug, and further increased the barriers to its use in research. Interestingly, it would later be recognized that the tissue solubility of 129 Xe that contribute to its anesthetic properties actually provided new and exciting opportunities for imaging of the lung beyond what is possible with 3 He.
3 He MR imaging entered clinical research in 1996 and soon expanded to multicenter clinical studies. The results of the ventilation studies showed significant correlation to conventional PFTs in patients with COPD, asthma, and cystic fibrosis. Diffusion-weighted imaging yielded the apparent diffusion coefficient (ADC), which is a sensitive marker of alveolar enlargement, and this marker was significantly increased in subjects with emphysema.
The problem with 3 He HP MR imaging is 2-fold. First, the only source of 3 He comes from the decay of tritium, which is exclusively derived from the past production of nuclear warheads in the United States. The supply from the current stockpile is becoming progressively depleted and access increasingly limited. Second, a large portion of the current stockpile has been allocated for homeland security applications to detect emitted neutrons from smuggled plutonium. These reasons have driven up costs significantly to approximately $800 to $2000 per liter depending on academic versus commercial use. With these greater costs and lesser availability, 3 He HP MR imaging, although having contributed greatly to the creation of this field, is not sustainable economically.
Recent progress in 129 Xe polarization technology led Patz and colleagues to reintroduce 129 Xe MR imaging in humans. Xenon has a long history of safe use as a contrast agent in CT lung imaging studies, which was confirmed by Driehuys and colleagues, who rigorously tested the safety and tolerability of inhaling multiple, undiluted 1-L volumes of HP 129 Xe. No major adverse effects were reported in total of 44 study subjects including healthy volunteers and COPD patients. Among the reported symptoms were mild dizziness, paresthesia/hypoesthesia, and euphoria, which were transient for approximately 1 to 2 minutes. No subject showed changes in laboratory tests or electrocardiogram. With the advent of more efficient polarizers, resulting in improved 129 Xe polarization, one can expect better image quality with a lesser volume of xenon, and the described symptoms are likely to be diminished further. In fact, a second safety study by Shukla and co-workers showed that inhalation of only 0.5 L volumes caused subjects to experience few or no symptoms.
Technique
Traditional MR imaging of the lungs is fraught with a number of difficulties. Conventional MR scanners are primarily tuned to excite hydrogen protons ( 1 H) that are present in abundance in water molecules. However, the lungs have only very low 1 H density (∼20%) compared with other anatomic structures. Combined with a long relaxation time, the signal available for imaging is minimal. Further complicating the image acquisition is the inhomogeneous magnetic environment of the lung, which introduces significant susceptibility artifacts that further challenge conventional MR acquisitions. However, these problems of MR-based lung imaging are not faced by the external gaseous contrast media ( 3 He or 129 Xe), which instead image the airways and airspaces within the lungs rather than the surrounding tissues ( Fig. 2 ). This greatly reduces the problems of unfavorable longitudinal and transverse relaxation times faced by 1 H MR imaging in the lung. On the other hand, MR imaging of a gas is challenging because its density is typically about 4 orders of magnitude less than that of protons ( 1 H density of water ∼100 mol/L vs 129 Xe gas density ∼0.01 mol/L). This lower density reduces commensurately the available signal intensity and would seem to make gas MR imaging impossible. To circumvent this limitation, a physical process called hyperpolarization is used to increase the magnetization of these particular gases by about 5 orders of magnitude. Hyperpolarization more than overcomes their low density and makes MR-based imaging of these inhaled gases feasible within a single breath-hold.
Gas Polarization
Physics
The physics around polarizing gases dates back to the atomic physics publications in the 1960s. This technology remained of purely intellectual interest until the introduction of high-power lasers afforded the ability to polarize large volumes of gases on reasonable time scales. This paved the way for the use of HP gases in medical imaging. The schematic shown in Fig. 3 describes the sequence of events involved in increasing the nuclear spin polarization of either 3 He or 129 Xe. This involves 2 processes: (1) optical pumping and (2) spin exchange.
As shown in Fig. 3 A depicting 6 nuclear spins, under normal conditions, roughly one-half of the nuclear spins within the gas volume are aligned parallel to the direction of the main magnetic field and one-half against it. This situation leads to zero signal because the MR signal is determined by the difference in the number of spins aligned in either direction, that is, polarization. Hence, the most ideal scenario that would give us the most signal would have all the nuclear spins pointed along 1 direction, or 100% polarized. If we were to put this ensemble of spins into a large magnetic field like that of a 1.5-T or 3.0-T scanner, it would cause slightly more spins to align with rather than against the field. This difference, although sufficient for imaging with ubiquitous sources like water, is not nearly sufficient for imaging dilute gases like 3 He or 129 Xe. An alternative way of viewing our hypothetical system is to note that we need only to add 3 quanta of angular momentum to turn every downward pointed nuclear spin to one that is up and thereby align every nuclear spin in the same direction. Thus, hyperpolarization involves simply adding angular momentum to the system.
To achieve this, circularly polarized laser light is used as a carrier of angular momentum. However, nuclei cannot directly absorb laser light, so we use an intermediary to absorb the light and its angular momentum. Specifically, laser light is tuned to the principal resonance of an alkali metal atom such as rubidium (Rb), which causes its single outer shell valence electron to become aligned. This process is known as optical pumping (see Fig. 3 B). Only alkali metal atoms with electron spins that are down can absorb the light, so simply illuminating the alkali vapor with circularly polarized resonant light converts the entire sample to the spin up direction. Once a valence electron spin has been flipped up, it remains in this state until collisions cause it to depolarize. Then, it simply absorbs another photon and returns to the aligned state.
Subsequently, through collisions between polarized electron spins of the alkali metal Rb and the 129 Xe or 3 He nuclei, the alignment from Rb valence electron is transferred to the noble gas nucleus. This process is referred as spin exchange (see Fig. 3 C). After the spin exchange collision, the Rb electrons become aligned again by absorbing additional laser light and continue to build polarization within the available noble gas nuclei. Currently available optical pumping and spin exchange techniques deliver polarizations of approximately 40% to 80% for 3 He and approximately 10% to 40% for 129 Xe. Recently, very high peak 129 Xe polarization levels have been demonstrated in diluted mixtures.
Gas polarization technique
A simplified schematic for xenon polarization is shown in Fig. 4 . Optical pumpin g is carried out using Rb, which is contained within a glass optical cell. This optical cell is housed in an oven, surrounded by 2 Helmholtz coils that generate a small, but homogeneous 20 G magnetic field. The Rb in the optical cell is heated to approximately 150°C to produce a Rb vapor pressure equal to about 1 ppm of the total gas density in the cell. During this time, 10 to 100 W of circularly polarized laser light tuned to the D1 transition of Rb illuminates the optical cell. The Rb vapor absorbs a significant fraction (>50%) this incident laser light, which polarizes the valence electron spins on the Rb atoms in the vapor.