Thymoma is the most common primary malignancy of the anterior mediastinum and the most common thymic epithelial neoplasm, but it is a rare tumor that constitutes less than 1% of adult malignancies. Computed tomography (CT) is currently the imaging modality of choice for distinguishing thymoma from other anterior mediastinal masses, characterizing the primary tumor, and staging the disease. However, magnetic resonance imaging is also effective in evaluating and characterizing anterior mediastinal masses and staging thymoma in patients with contraindications to contrast-material-enhanced CT such as contrast allergy and/or renal failure.
Key points
- •
Although thymoma is a rare tumor, it is the most common primary malignancy of the anterior mediastinum.
- •
MR imaging is an excellent tool for characterizing anterior mediastinal masses and elegantly distinguishes normal thymus and thymic hyperplasia from malignant neoplasms involving the thymus.
- •
Thoracic MR imaging may be used to stage patients in whom allergy to intravenous contrast and/or renal failure precludes evaluation with contrast-enhanced chest computed tomography (CT).
Introduction
Thymoma is the most common primary malignancy of the anterior mediastinum, but it is a rare tumor that constitutes less than 1% of adult malignancies. Thmyoma is the most common thymic epithelial neoplasm, a group that also includes thymic carcinoma and thymic carcinoid. Because of the rarity of thymoma, it has not been evaluated thoroughly and many of the studies regarding imaging characteristics of the tumor were single-institution studies spanning multiple decades. Increased interest in thymic malignancies and greater international collaboration over the past 5 years has ultimately resulted in the formation of the International Thymic Malignancy Interest Group (ITMIG), an organization that provides infrastructure for the study of these lesions. With the formation of an international thymic malignancy database, it is hoped that large-scale multiinstitutional studies will overcome the smaller ones of the past and advance the knowledge in the detection, staging, and treatment of this disease. CT is currently the imaging modality of choice for distinguishing thymoma from other anterior mediastinal masses, characterizing the primary tumor, and staging the disease. However, MR imaging is also effective in evaluating and characterizing anterior mediastinal masses and staging thymoma in patients with contrast allergy and/or renal failure, which preclude evaluation with contrast-material-enhanced CT. This review focuses on the characterization, classification, and staging of thymoma based on various morphologic features that may be identified on MR imaging and the impact of imaging findings on therapy and management.
Introduction
Thymoma is the most common primary malignancy of the anterior mediastinum, but it is a rare tumor that constitutes less than 1% of adult malignancies. Thmyoma is the most common thymic epithelial neoplasm, a group that also includes thymic carcinoma and thymic carcinoid. Because of the rarity of thymoma, it has not been evaluated thoroughly and many of the studies regarding imaging characteristics of the tumor were single-institution studies spanning multiple decades. Increased interest in thymic malignancies and greater international collaboration over the past 5 years has ultimately resulted in the formation of the International Thymic Malignancy Interest Group (ITMIG), an organization that provides infrastructure for the study of these lesions. With the formation of an international thymic malignancy database, it is hoped that large-scale multiinstitutional studies will overcome the smaller ones of the past and advance the knowledge in the detection, staging, and treatment of this disease. CT is currently the imaging modality of choice for distinguishing thymoma from other anterior mediastinal masses, characterizing the primary tumor, and staging the disease. However, MR imaging is also effective in evaluating and characterizing anterior mediastinal masses and staging thymoma in patients with contrast allergy and/or renal failure, which preclude evaluation with contrast-material-enhanced CT. This review focuses on the characterization, classification, and staging of thymoma based on various morphologic features that may be identified on MR imaging and the impact of imaging findings on therapy and management.
Epidemiologic and clinical features
The incidence of thymoma is 1 to 5 cases per million individuals per year in the United States, and it is higher in African Americans and Asians. Men and women are affected equally. The incidence of thymoma increases with age, and the condition is most common in patients older than 40 years, but decreases in incidence after 60 years of age. Children are only rarely affected.
The most common clinical symptoms reported at the time of diagnosis include chest pain, dyspnea, and cough. These symptoms are present in up to one-third of patients and typically secondary to compression and/or invasion of mediastinal structures. Dysphagia, diaphragmatic paralysis, and superior vena cava syndrome may also be present. One-third of patients present with systemic symptoms and paraneoplastic syndromes because of the presence of hormones, antibodies, and cytokines released by the tumor. The most common paraneoplastic syndrome associated with thymoma is myasthenia gravis, which is present in 30% to 50% of patients and is more common in women than in men. Other paraneoplastic syndromes include hypogammaglobulinemia and pure red cell aplasia, which are present in 10% and 5% of cases, respectively. Autoimmune disorders such as systemic lupus erythematosus, polymyositis, and myocarditis may be associated with thymoma. Patients may be asymptomatic, and the increased utilization of CT for the diagnosis and follow-up of benign and malignant diseases has increased the detection of incidental thymomas.
Histology and classification
Thymomas are typically solid, encapsulated tumors that are restricted to the thymus. One-third of thymomas demonstrate necrosis, hemorrhage, or cystic components, and one-third of tumors invade the capsule and adjacent structures. Although thymomas are typically slow-growing malignancies, aggressive features such as invasion of surrounding structures and involvement of the pleura and pericardium may be present. However, compared with thymic carcinoma and other malignancies of the anterior mediastinum, distant metastases are rare.
The histologic classification of thymoma is complex and has been the source of controversy. Histologically, thymomas are composed of neoplastic epithelial cells and nonneoplastic lymphocytes, and most tumors are heterogeneous in composition. The first histologic classification scheme developed by the World Health Organization (WHO) Consensus Committee was released in 1999 and classified thymomas into 6 separate subtypes (A, AB, B1, B2, B3, and C) based on morphologic features of the neoplastic epithelial cells and the lymphocyte:epithelial cell ratio. A revised WHO classification scheme was published in 2004 and moved type C (thymic carcinoma) to a separate category. However, there are inherent limitations in this classification system. Because thymomas are typically heterogeneous tumors, many different subtypes may coexist within the same lesion. In addition, when diagnosis is made from tissue obtained via needle biopsy, the sample obtained may not be representative of the predominant subtype of the tumor. For histologic classification to be useful, it should correlate with prognosis so that therapy could be selected according to the classification. The WHO classification schemes of 1999 and 2004 lacked intraobserver and interobserver reproducibility and clinical predictive value. At present, the most important feature of the histologic classification of thymic epithelial malignancies is differentiation of thymic carcinoma from thymoma, because thymic carcinoma is the most distinct group histologically and clinically with worse outcomes. However, worse clinical outcomes have also been shown for subtype B3 when compared with the other histologic subtypes combined.
Staging
Many staging systems for thymoma have been proposed. However, the Masaoka system ( Table 1 ) and a variant of it, the Masaoka-Koga staging system, are the most commonly used systems. The Masaoka-Koga staging system is the one recommended by the ITMIG because of its correlation with patient survival as documented in several studies ( Table 2 ). The Masaoka-Koga staging system is based on the gross and microscopic features of thymoma. Tumors are designated as stage I when completely encaspulated; stage II in the setting of microscopic invasion through the capsule (IIa) or macroscopic invasion of the surrounding fat (IIb); stage III when invasion of an adjacent structure such as the great vessels, pericardium, or lung is present; and stage IV in the setting of pleural or pericardial dissemination (IVa) or lymphatic/hematogenous metastasis (IVb). Advanced-stage disease is defined as stages III and IV. Although the Masaoka system or its variants has been the most commonly used staging mechanism, a new TNM-based staging system has been proposed and will probably replace these schemes in the future.
| Stage | Descriptors |
|---|---|
| I | Complete encapsulation of tumor and no microscopic invasion of capsule |
| II | Macroscopic invasion into surrounding fat or mediastinal pleura Microscopic invasion into capsule |
| III | Invasion of pericardium, great vessels, or lung |
| IVa | Pleural or pericardial dissemination |
| IVb | Lymphatic/hematogenous metastasis |
| Stage | Descriptors |
|---|---|
| I | Complete encapsulation of tumor |
| IIa | Microscopic tumor invasion through capsule |
| IIb | Macroscopic tumor invasion into surrounding fat |
| III | Invasion of pericardium, great vessels, or lung |
| IVa | Pleural or pericardial dissemination |
| IVb | Lymphatic/hematogenous metastasis |
As the Masaoka-Koga system is a postsurgical staging system, the role of the radiologist in staging thymoma is critical because neoadjuvant chemotherapy may be used for specific stages (III and IV) of disease. Therefore, good communication between the radiologist and the surgeon is necessary to determine the extent of disease and formulate appropriate treatment strategies.
Treatment
Accurate staging and completeness of surgical resection are the 2 most important factors in formulating treatment strategies in patients with thymoma, because these factors demonstrate the strongest correlation with duration of progression-free and overall survival. Stage I and II tumors are treated with surgical resection alone. Adjuvant chemotherapy and radiation therapy have no role in the treatment of stage I tumors and most stage II tumors because they provide no additional survival benefit. However, postoperative radiation therapy is typically administered in cases of incompletely resected stage II tumors to eliminate residual disease. When features of advanced-stage disease such as locoregional spread into adjacent structures are present, complete resection of tumor leads to prolonged survival. In these patients, neoadjuvant chemotherapy may provide superior survival benefit when compared with adjuvant chemotherapy. Postoperative radiation therapy is typically administered in cases of incompletely resected stage III tumors. Chemotherapy after surgery may also be administered in this setting. The treatment of stage IVa thymomas is the same as that of stage III tumors. However, stage IVb tumor is typically treated with palliative chemotherapy only.
Role of MR imaging
MR imaging is rarely the first imaging modality used for investigation of chest symptoms or an abnormality detected on chest radiography, because CT is generally considered to be superior to MR imaging in the evaluation and characterization of most anterior mediastinal masses. One study analyzing 127 anterior mediastinal masses of various causes, including thymic epithelial neoplasms such as thymoma and thymic carcinoma, other primary malignancies of the anterior mediastinum such as mature teratoma and malignant germ cell tumors, as well as lymphoma, demonstrated a slight advantage in the ability to correctly diagnose the lesion by CT (61%) compared with MR imaging (56%). However, this was not the case for thymic cysts, which were better visualized on MR imaging. In general, the correct diagnosis was reached in 86% using a combination of CT and MR imaging. When a cystic mass is suspected or is to be investigated, MR imaging is the most useful imaging modality because it is superior to CT in distinguishing cystic from solid masses (for instance, thymic cysts from thymic neoplasms) and in identifying cystic/necrotic components within solid masses. MR imaging is also useful in differentiating thymic hyperplasia from thymic tumors and in evaluating patients with an anterior mediastinal mass suspicious for thymoma in whom iodinated contrast is contraindicated. Such patients should be imaged with MR imaging rather than an unenhanced chest CT because vessel and pericardial invasion (stage III) must be identified before surgery to enable neoadjuvant therapy in patients with thymoma. This invasion is readily demonstrated with MR imaging in such patients using black blood or white blood techniques.
The versatility of MR imaging may prove superior to that of CT in certain scenarios, which is elaborated on in the discussion of the differential diagnosis. In brief, chemical shift imaging can differentiate between normal thymus and thymic involvement with tumor, dynamic imaging can be used to distinguish thymoma from other anterior mediastinal tumors, and multishot spiral sequencing can be used for real-time imaging and evaluation of phrenic nerve involvement before surgery.
Imaging of Thymoma
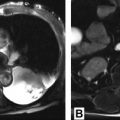
The primary role of MR imaging in the evaluation of patients with thymoma is the staging of disease when allergy to contrast media and/or renal failure precludes the utilization of contrast-enhanced CT ( Fig. 1 ).
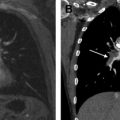
The typical appearance of thymoma is low to intermediate signal intensity on T1-weighted sequences and high signal intensity on T2-weighted sequences ( Fig. 2 ). As the signal intensity of thymoma on T2-weighted images may approach that of fat, fat-suppression techniques may be used to distinguish thymoma from adjacent mediastinal fat. Cystic changes and necrosis typically manifest as low signal intensity on T1-weighted images and high signal intensity on T2-weighted images ( Fig. 3 ). Fibrous septa and intratumoral nodularity demonstrate low signal intensity ( Fig. 4 ). The signal intensity of intratumoral hemorrhage is highly variable and depends on its age. For instance, hemosiderin typically manifests as low signal intensity on T1- and T2-weighted sequences, whereas acute or subacute hemorrhage may demonstrate T1 hyperintensity ( Fig. 5 ). As the main role of clinical staging is to identify local spread (ie, pericardium, vessels, and heart) as well as pleural spread, which is often resected, the entire chest should be imaged, not limiting the field of view to the anterior mediastinum. Intravenous contrast can be helpful in the identification of small pleural metastases as tumor enhances ( Fig. 6 ). The use of black blood or white blood techniques is helpful for evaluation of vascular invasion. Vessel distortion or tumor in the lumen of a vessel constitutes direct proof of stage III disease. Cardiac-gated black or white blood techniques are useful for better localization of tumors involving the heart, and perfusion studies are helpful when extensive cardiac muscle involvement is suspected for surgical planning.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree