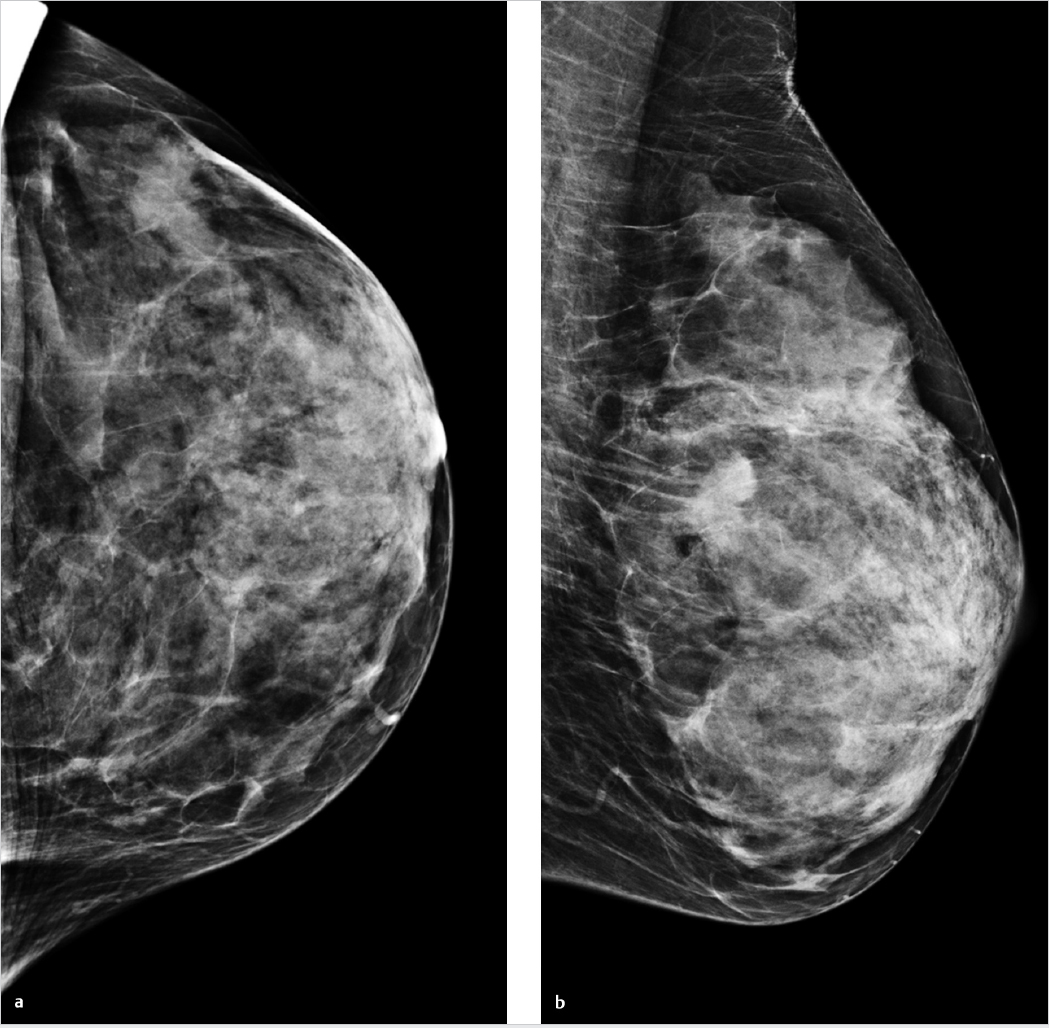
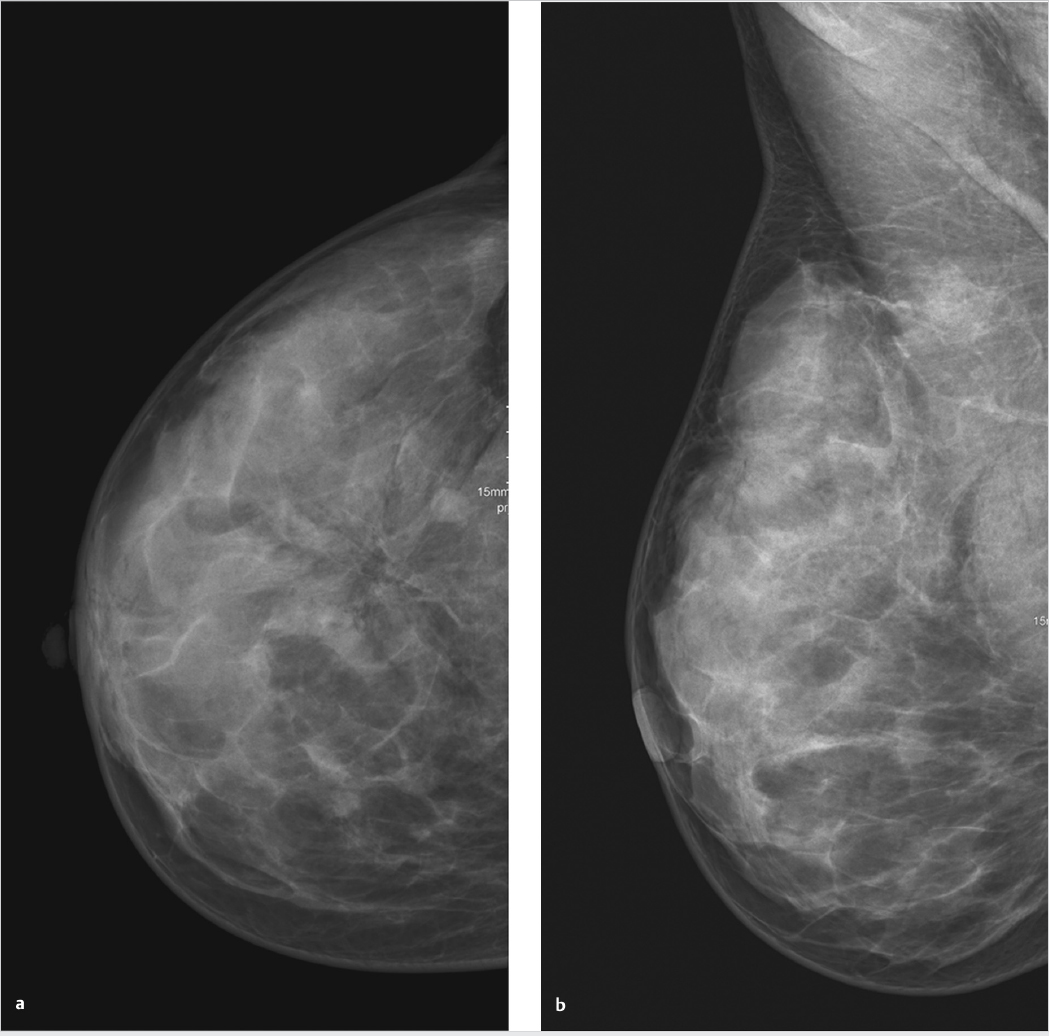
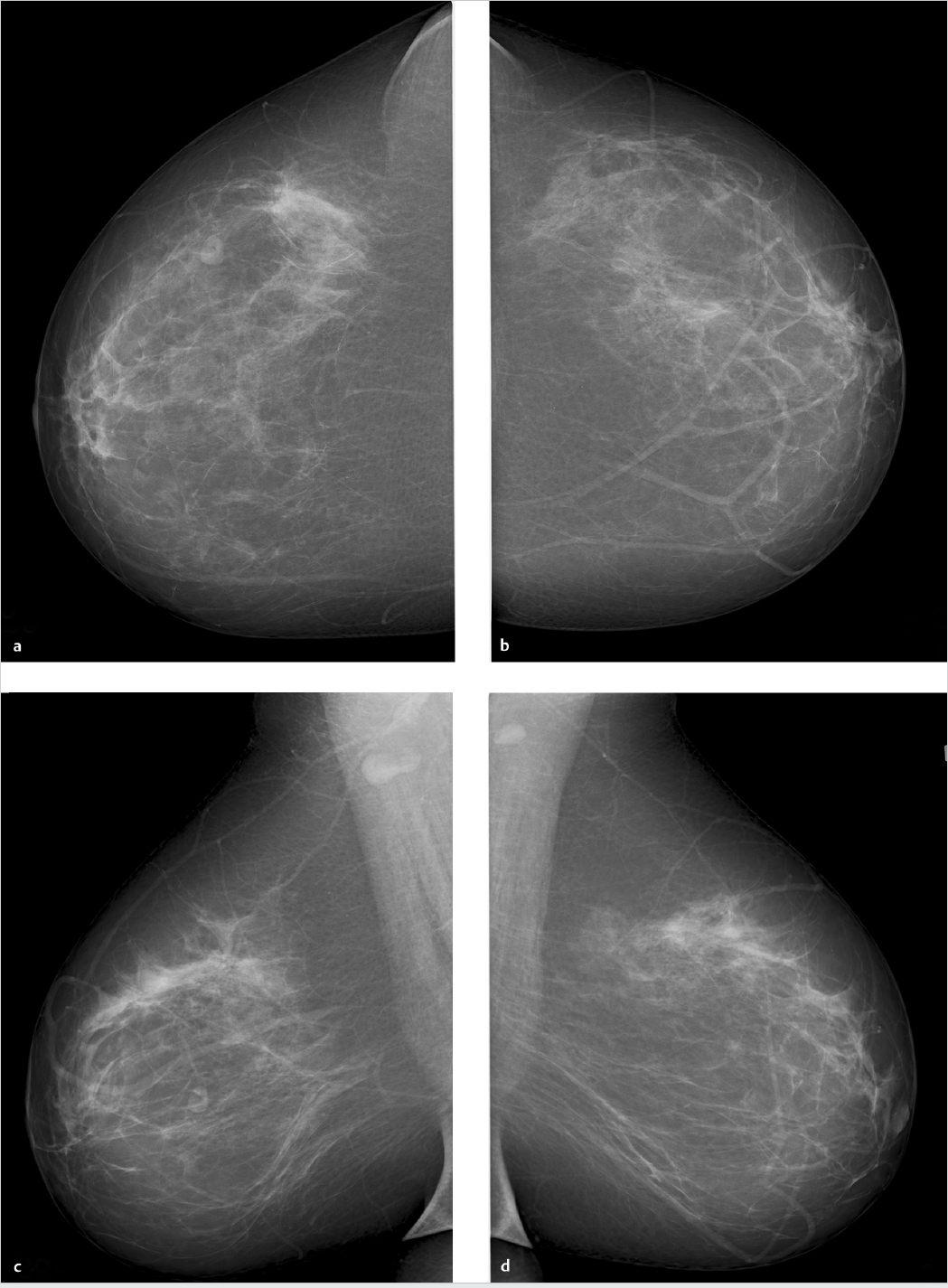
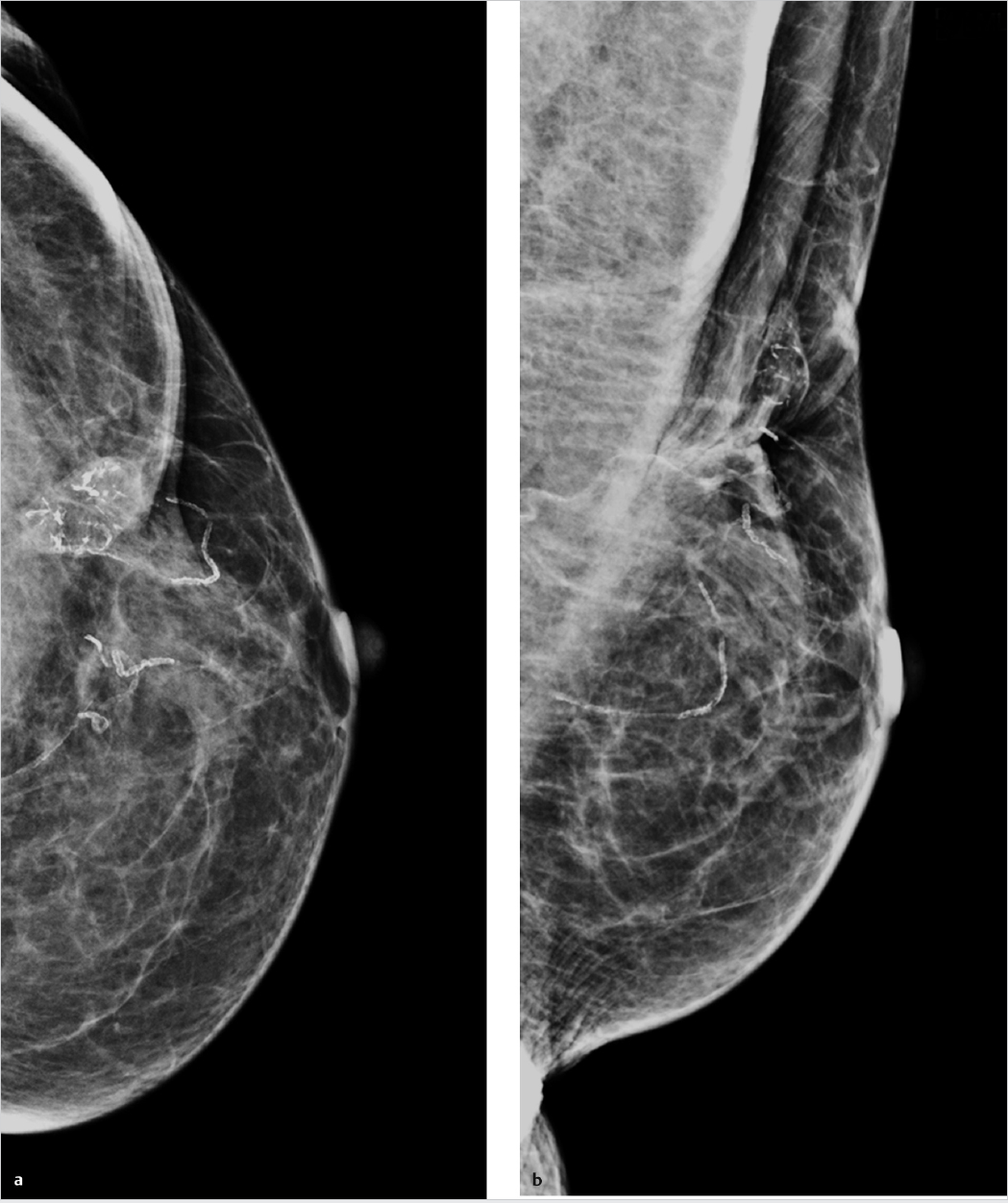
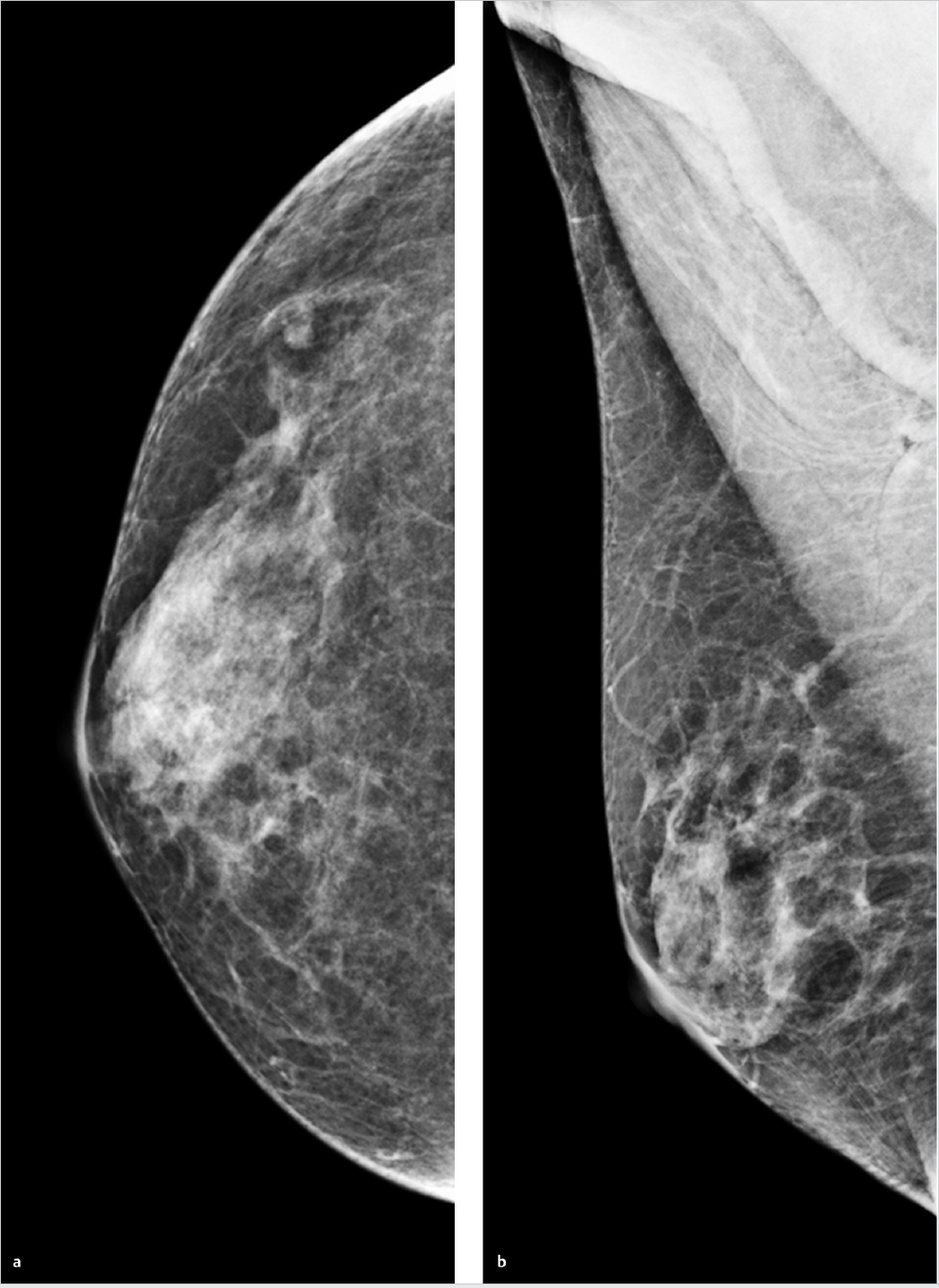
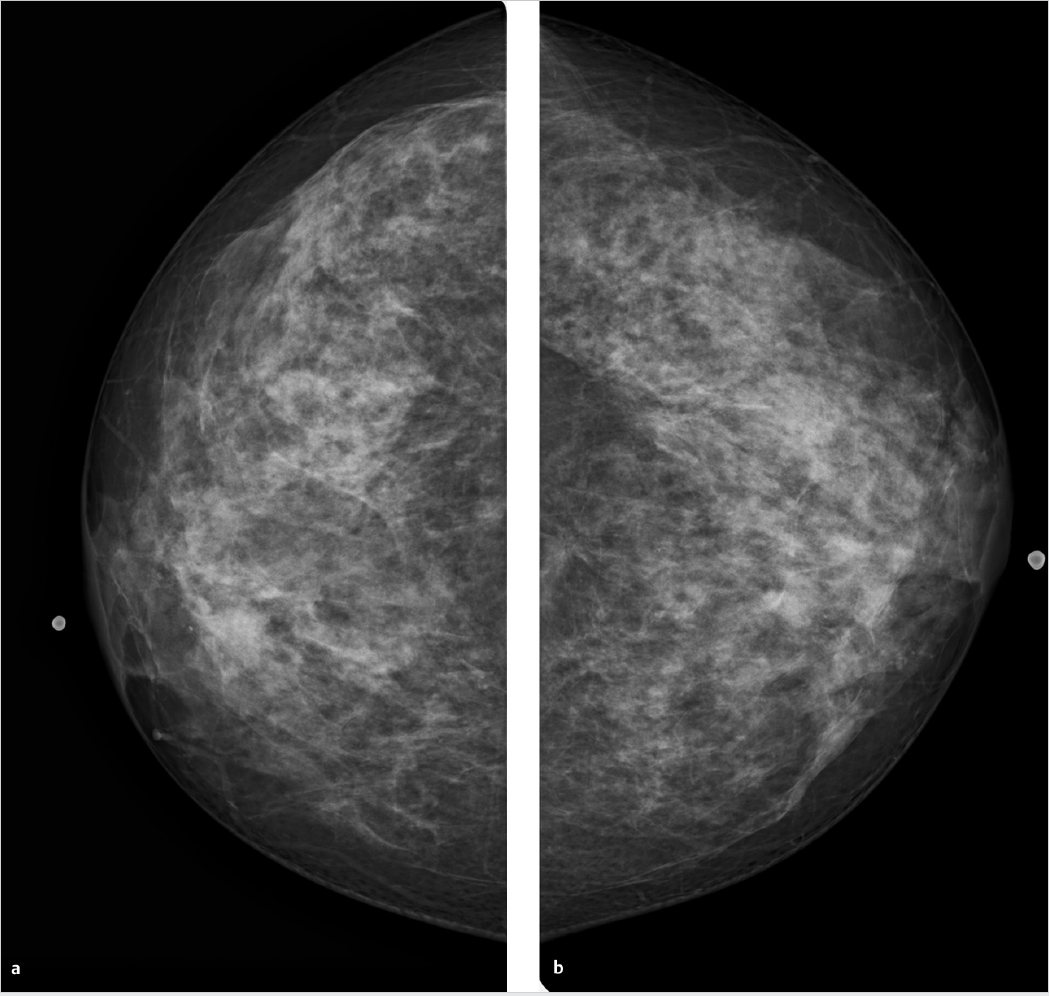
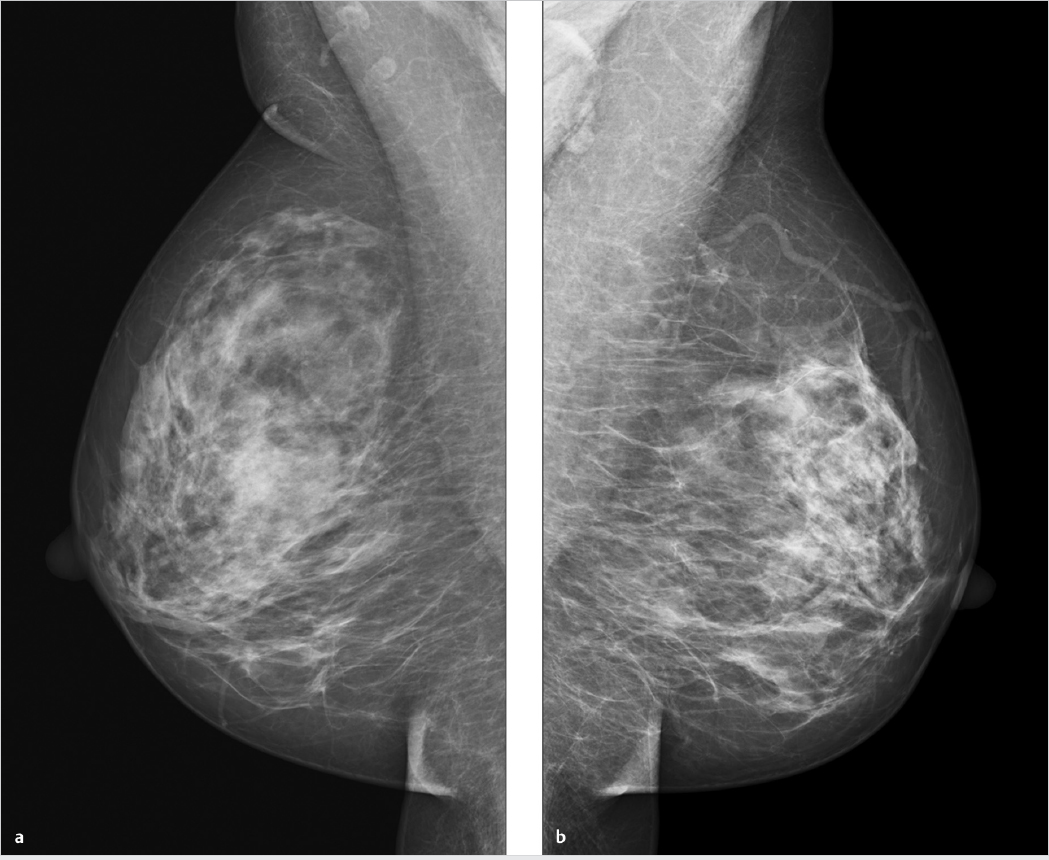
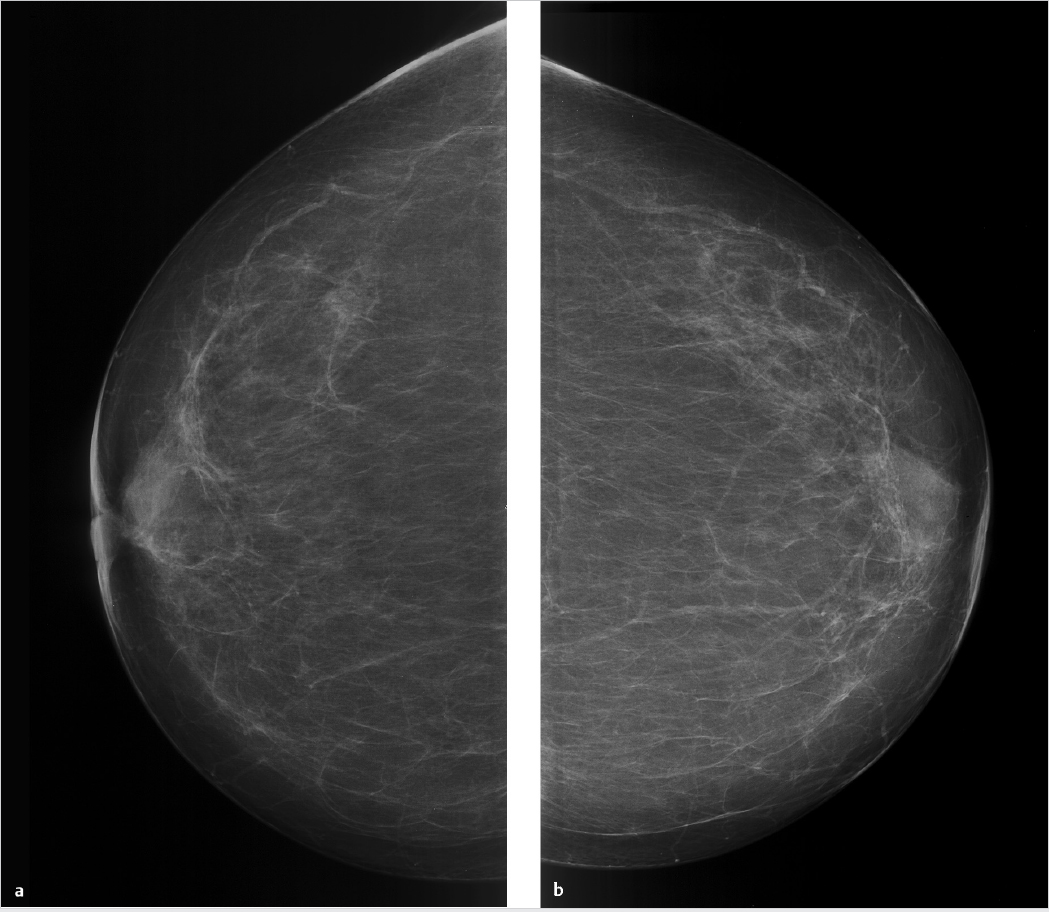
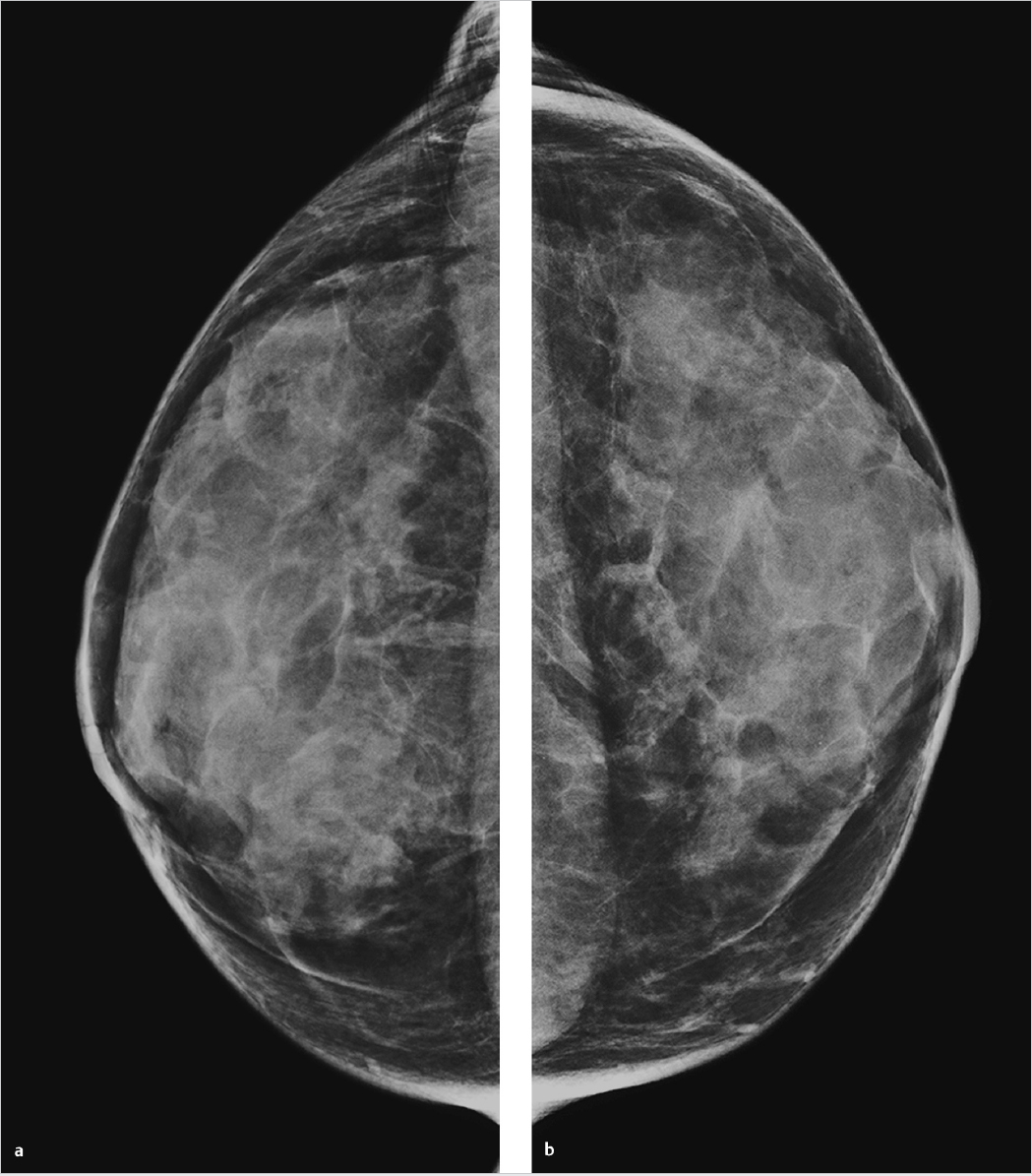
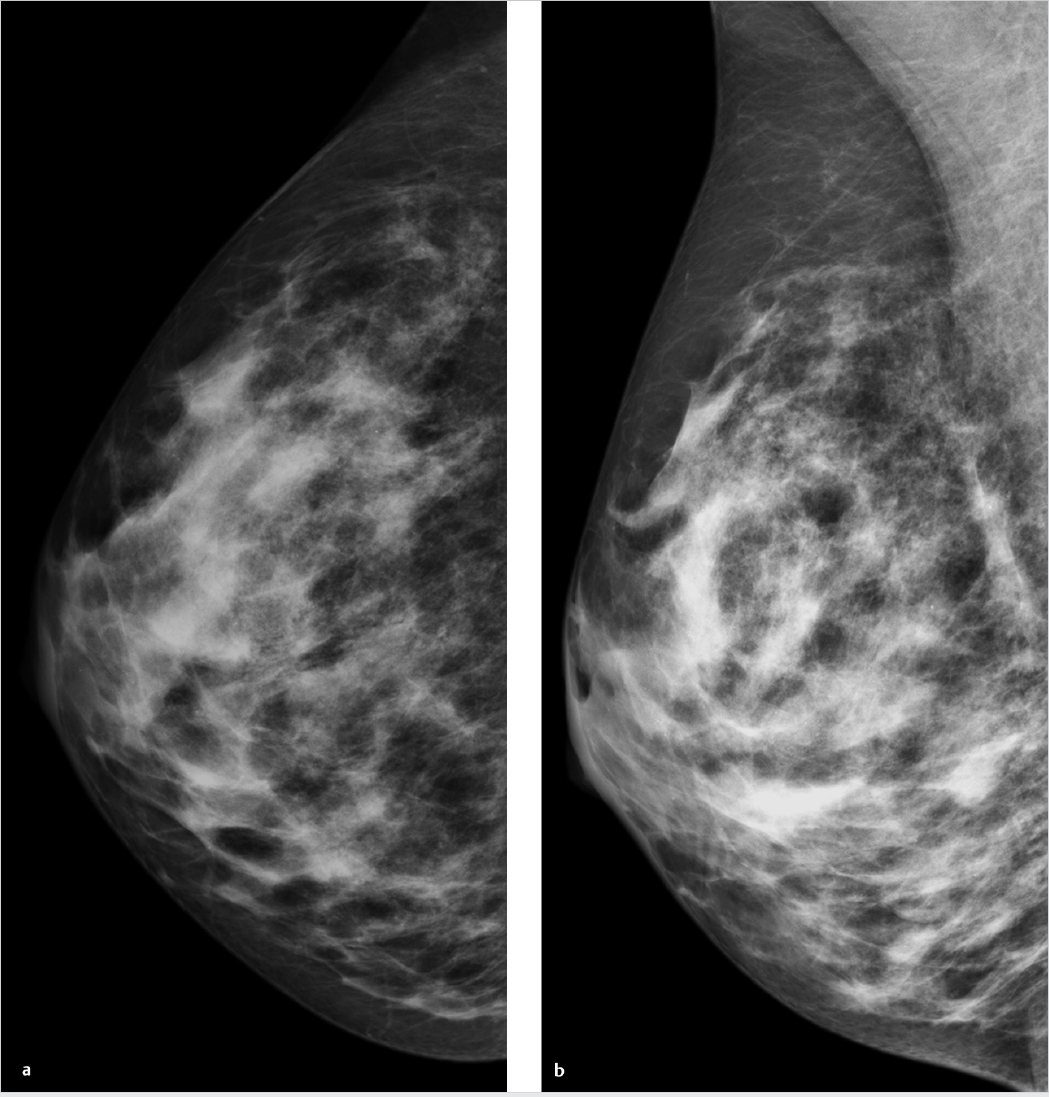
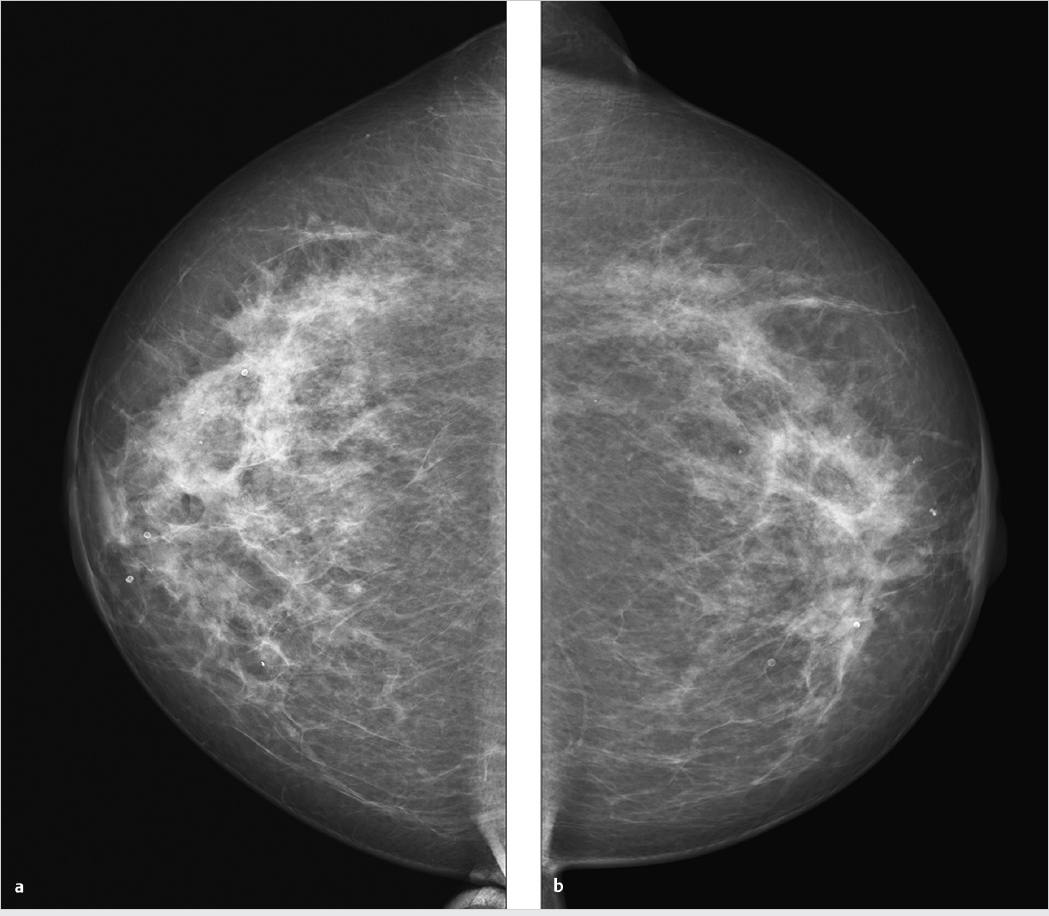
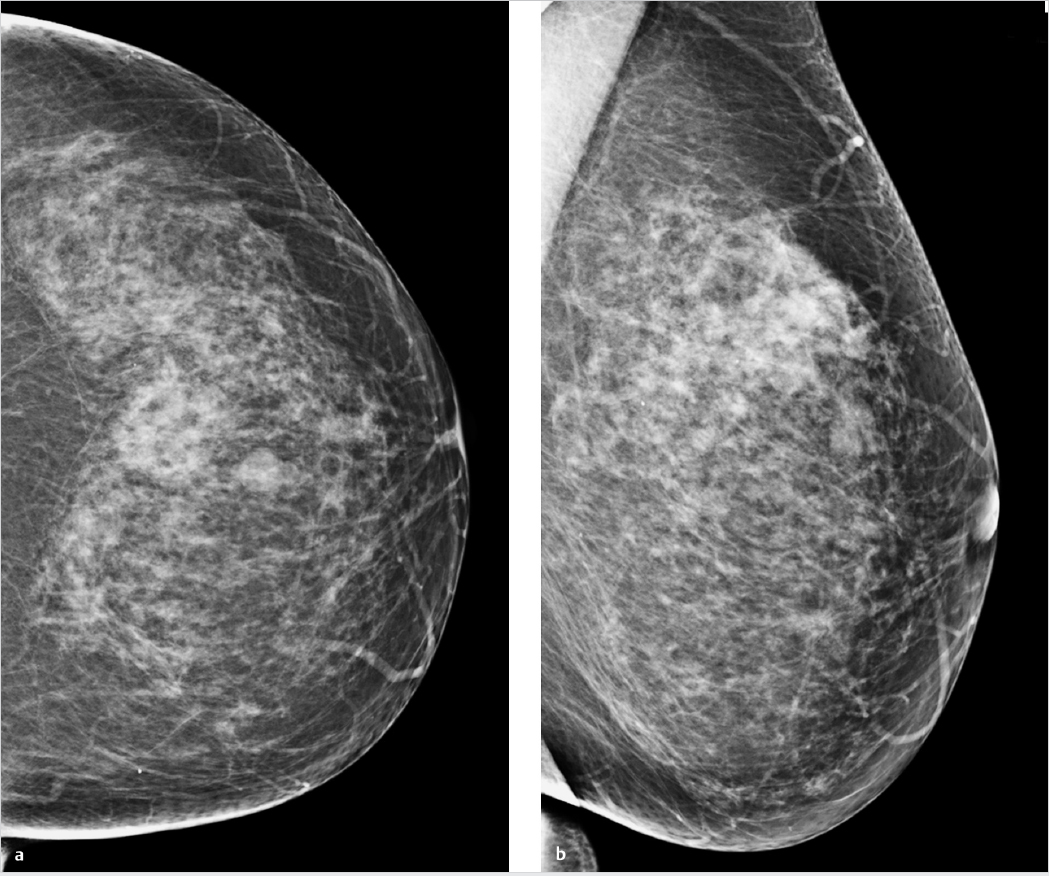
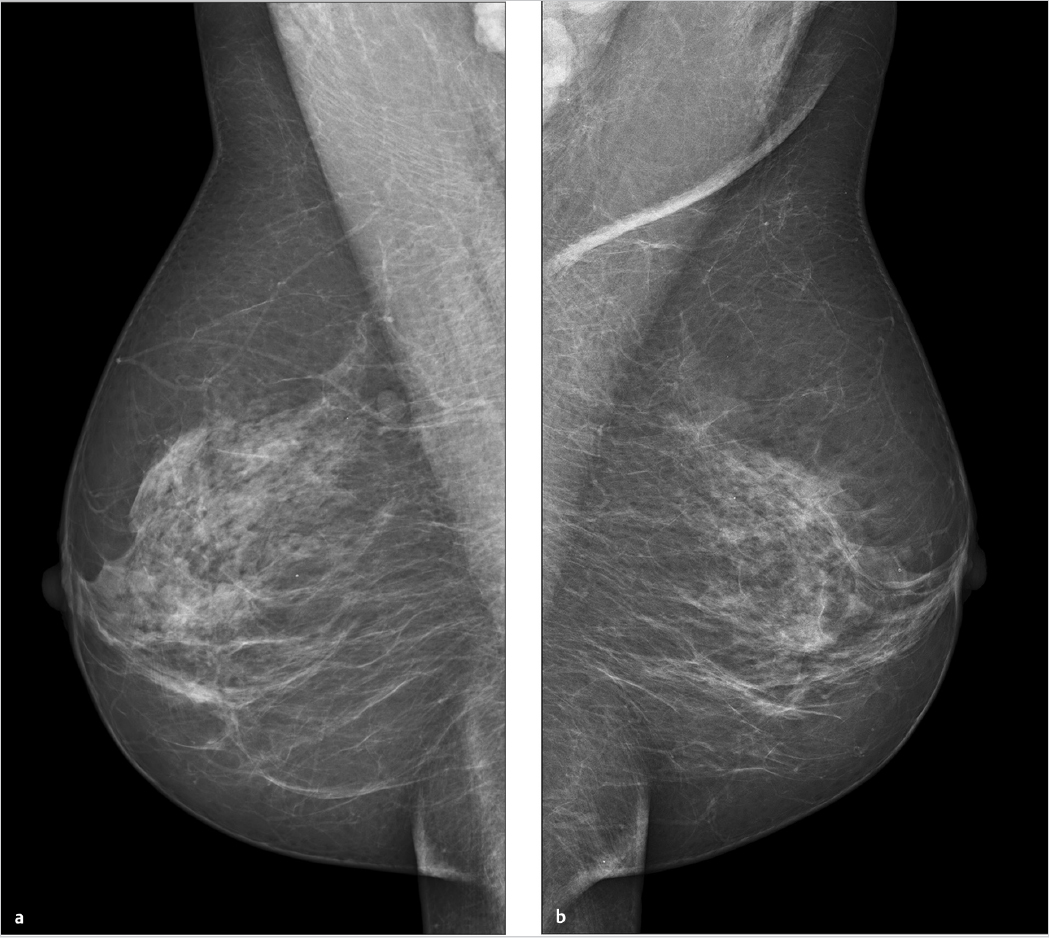
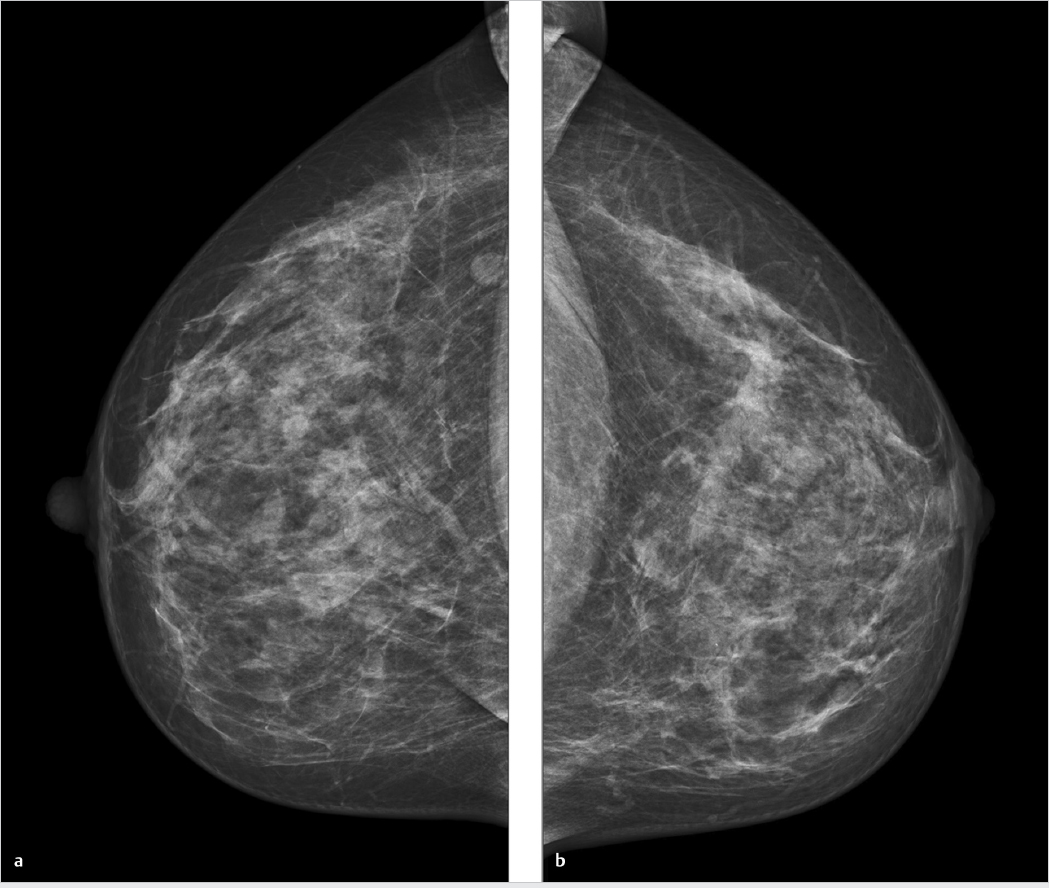
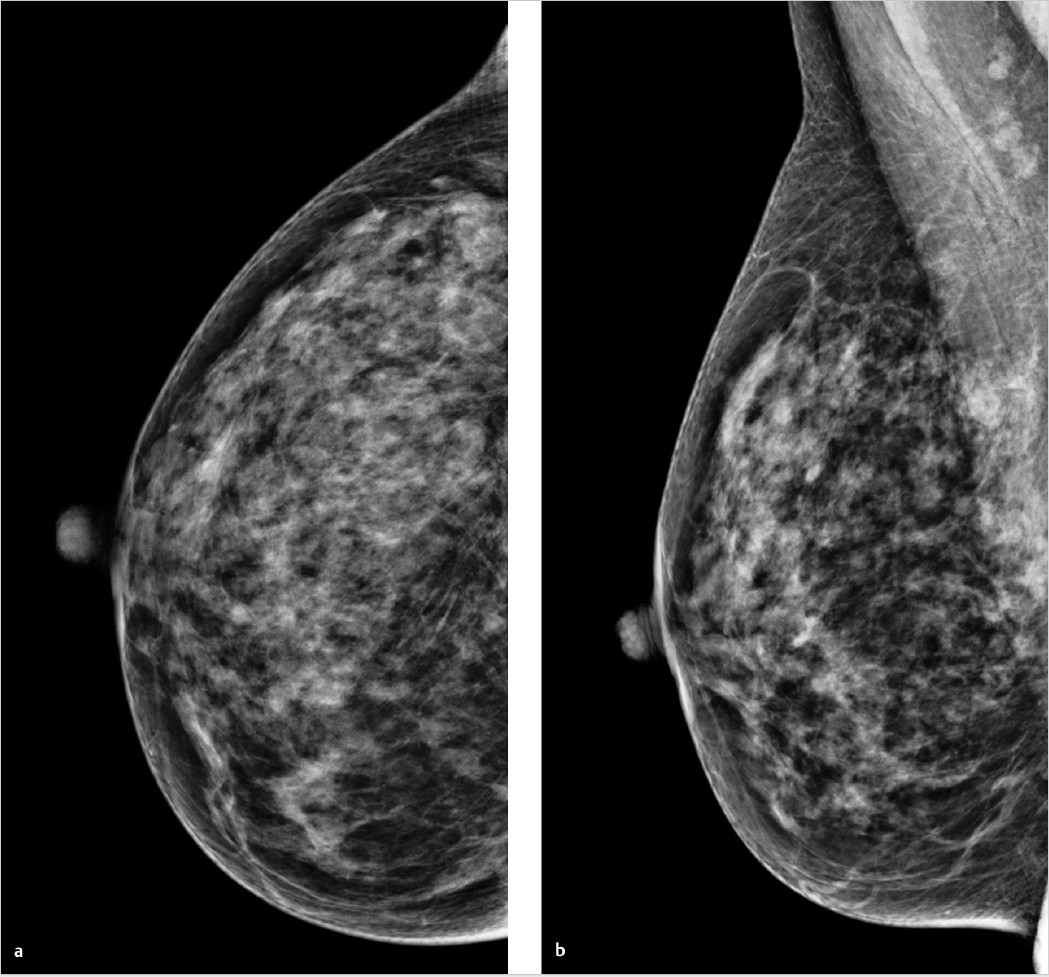
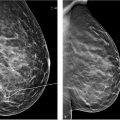
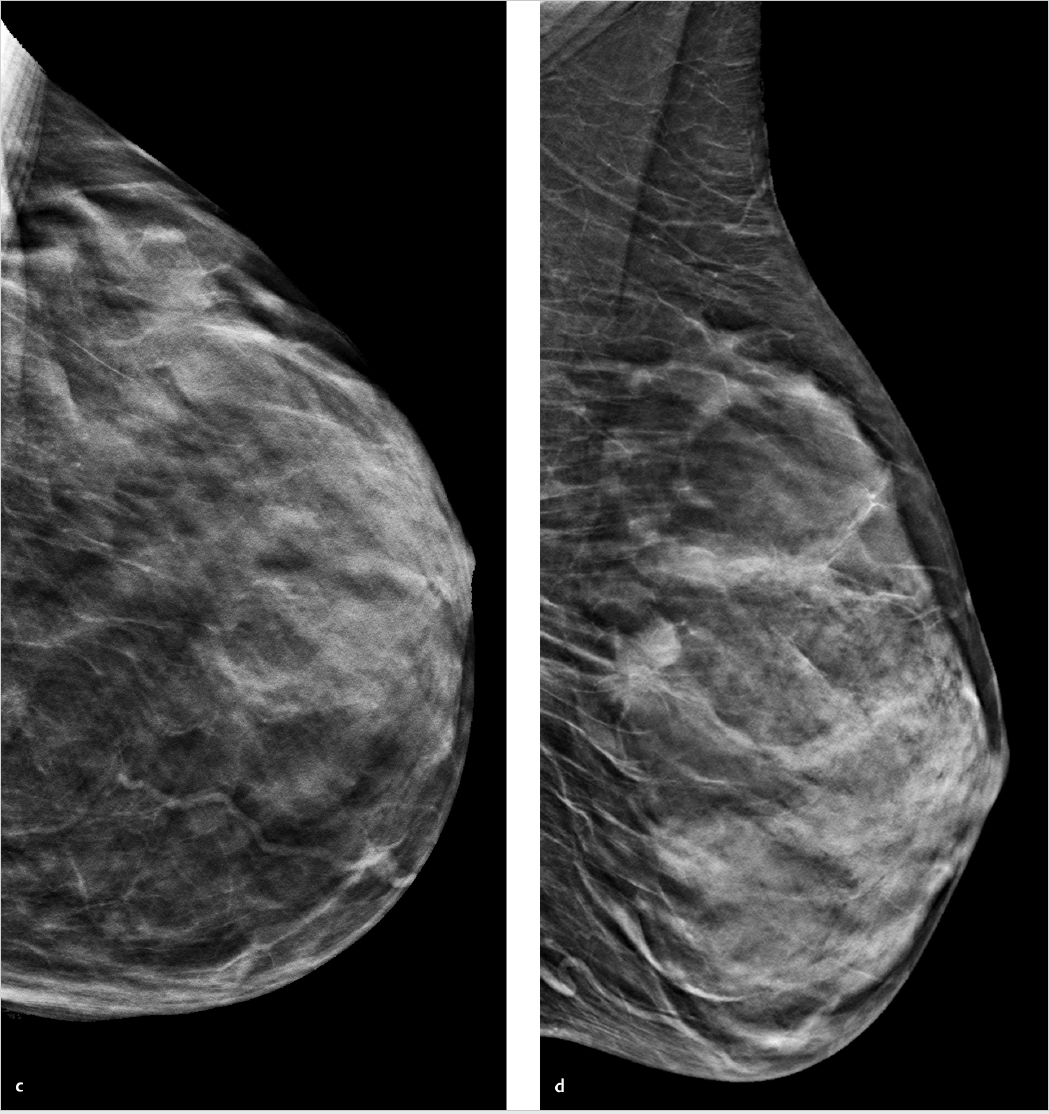
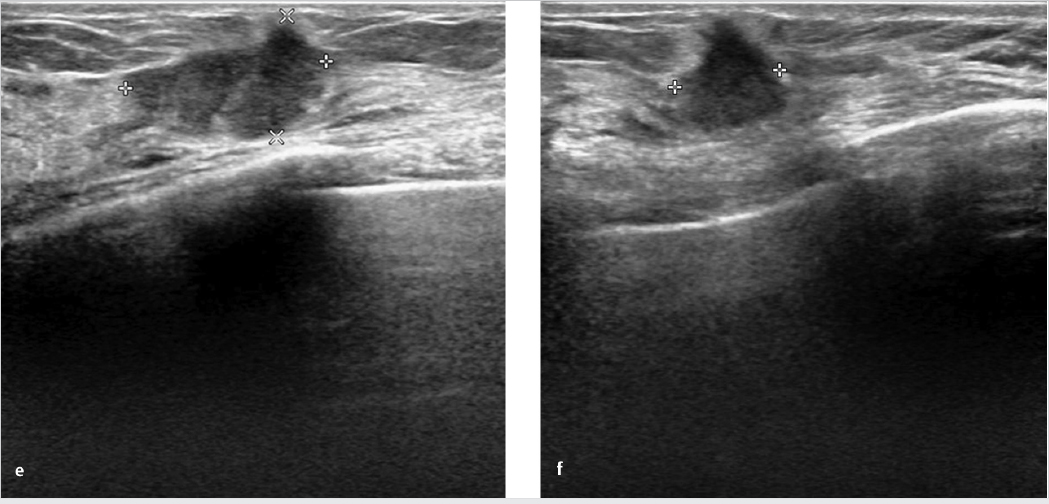
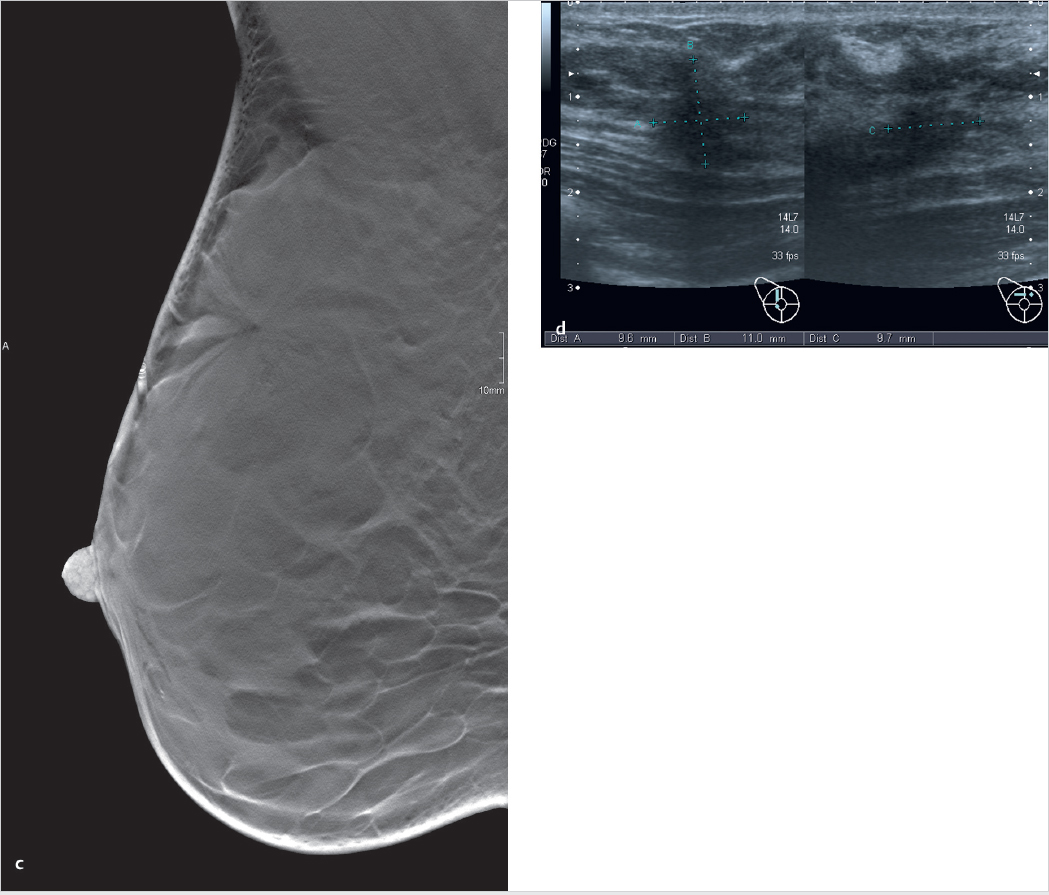
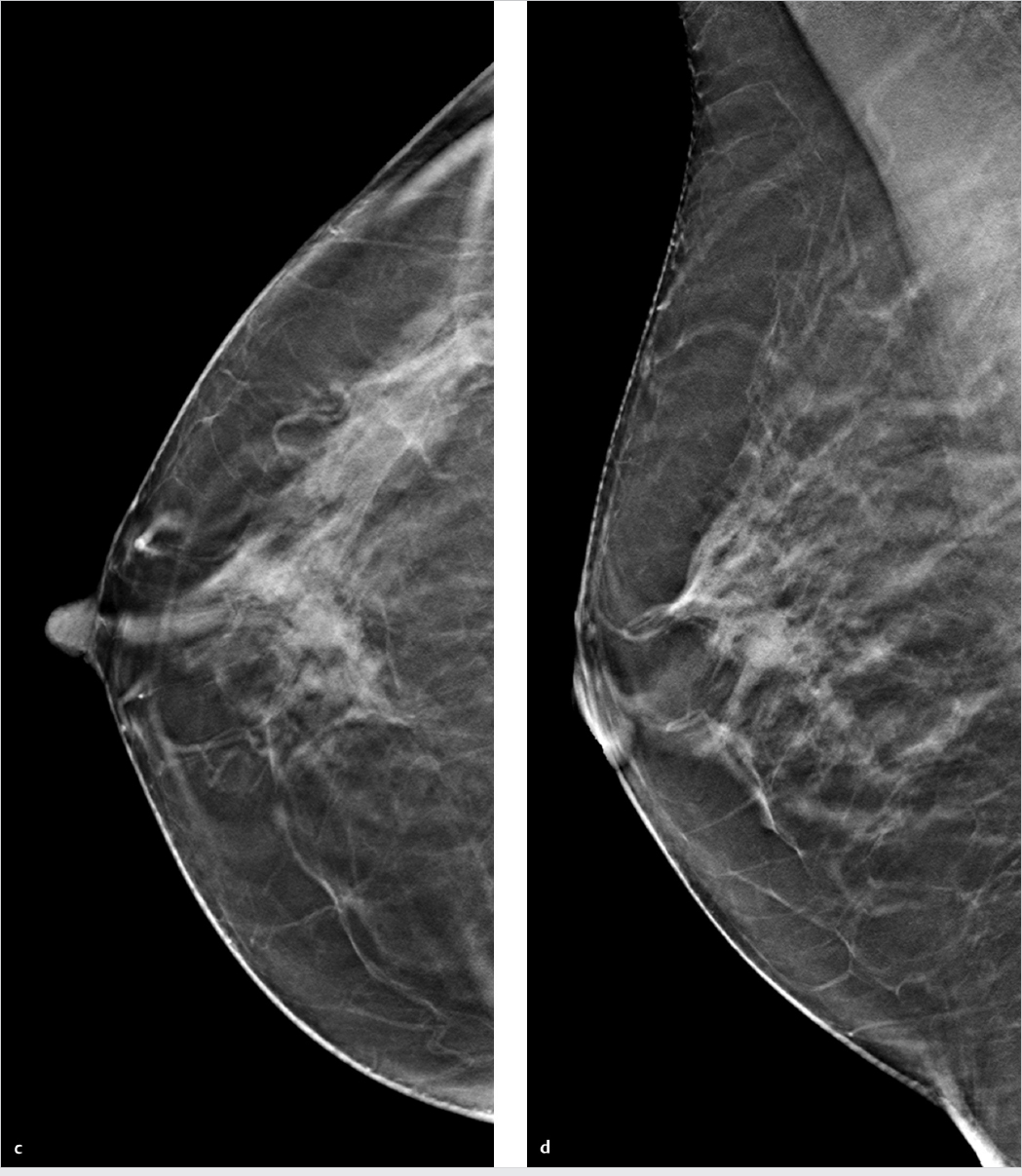
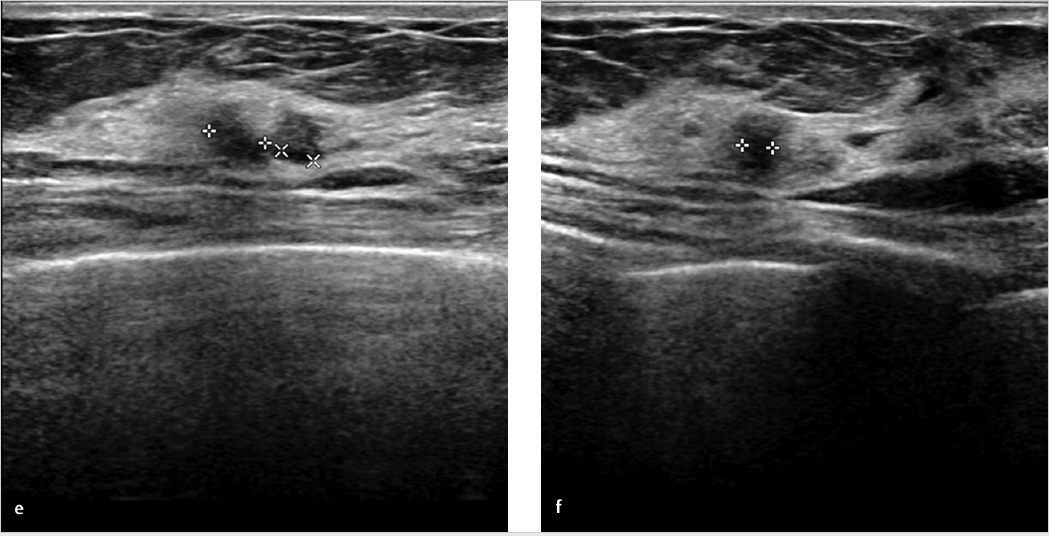
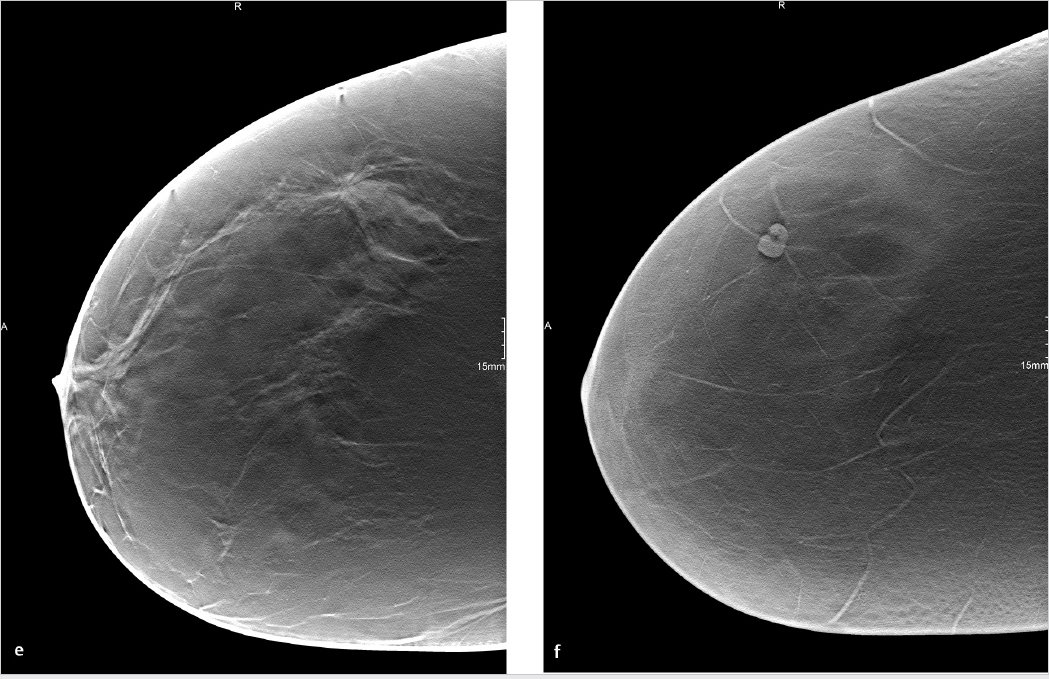
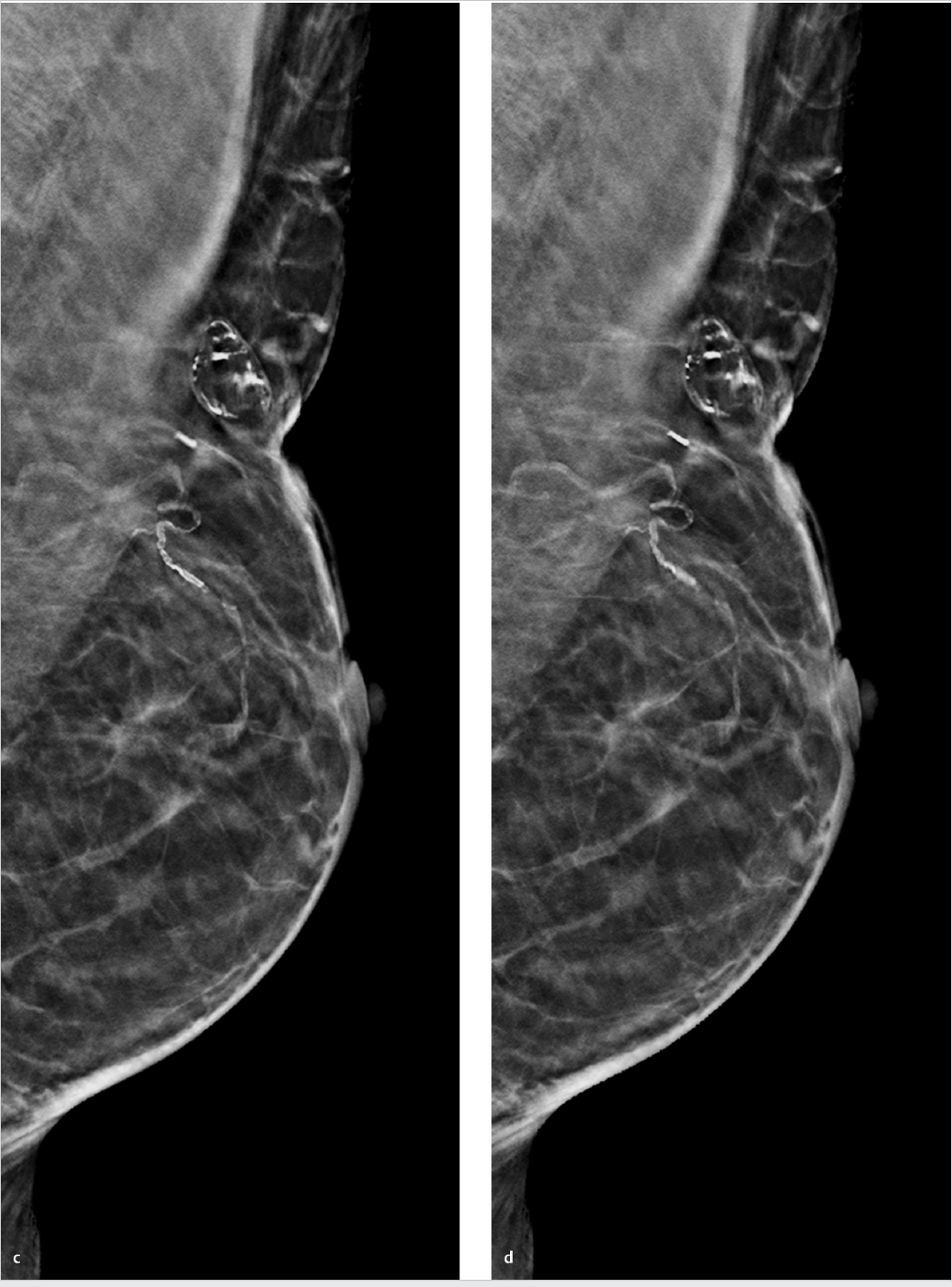
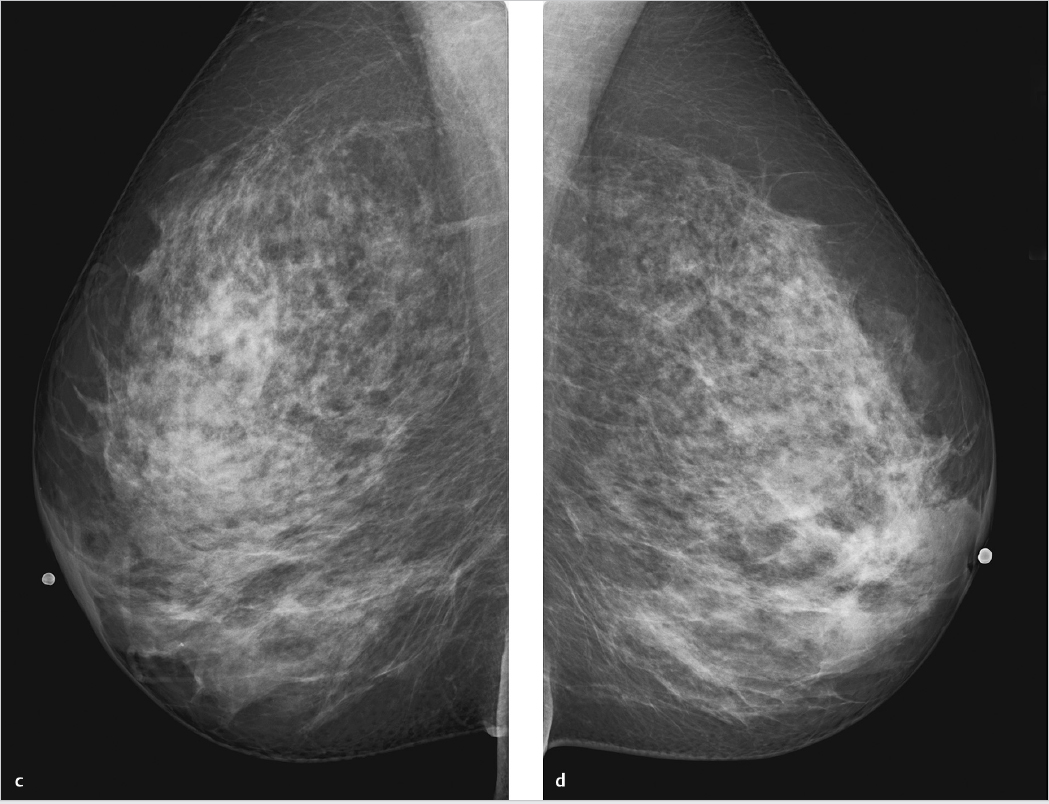
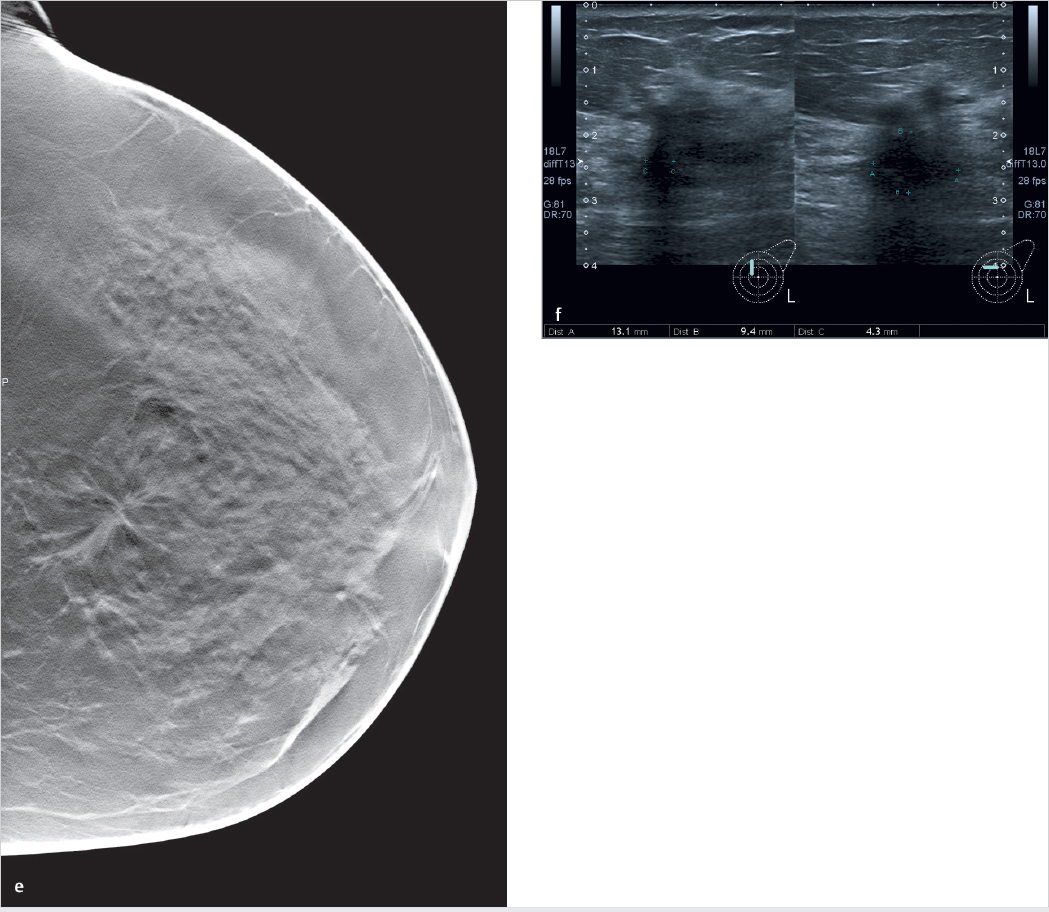
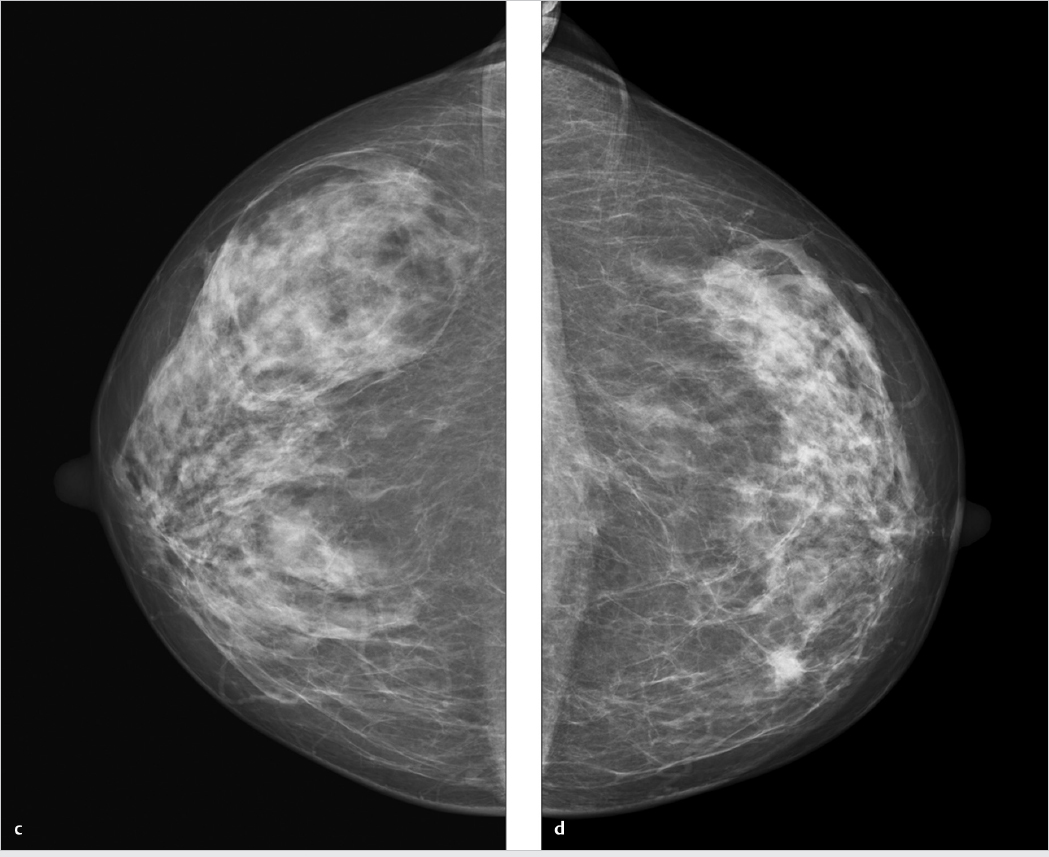
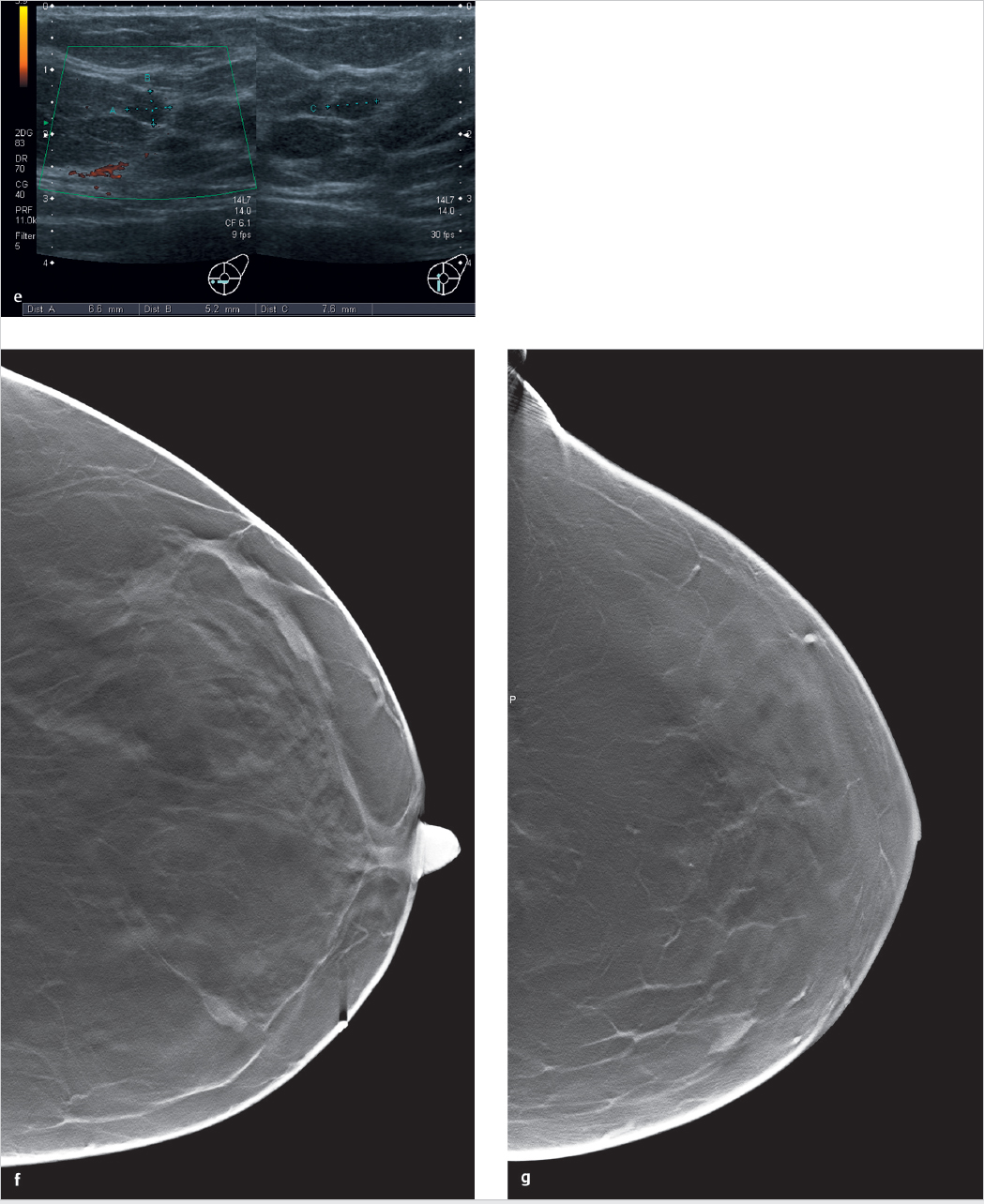
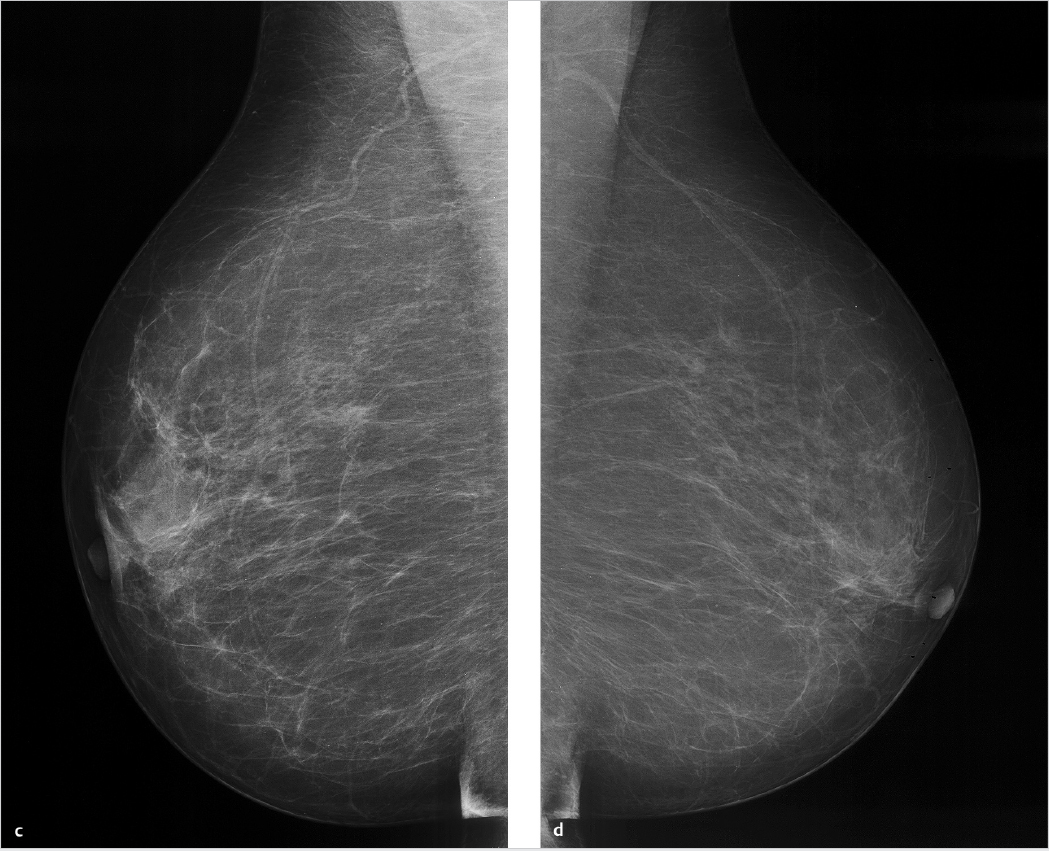
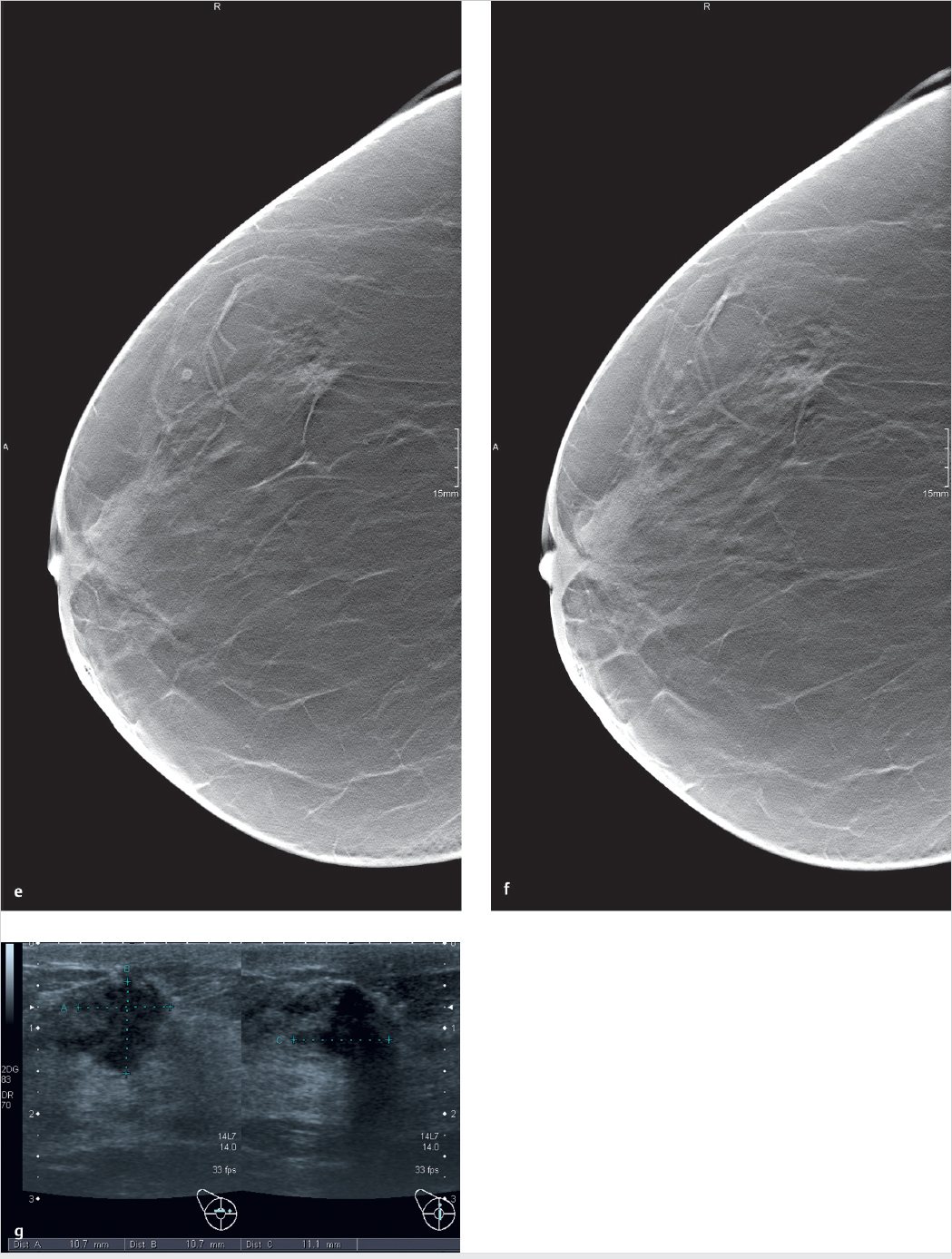
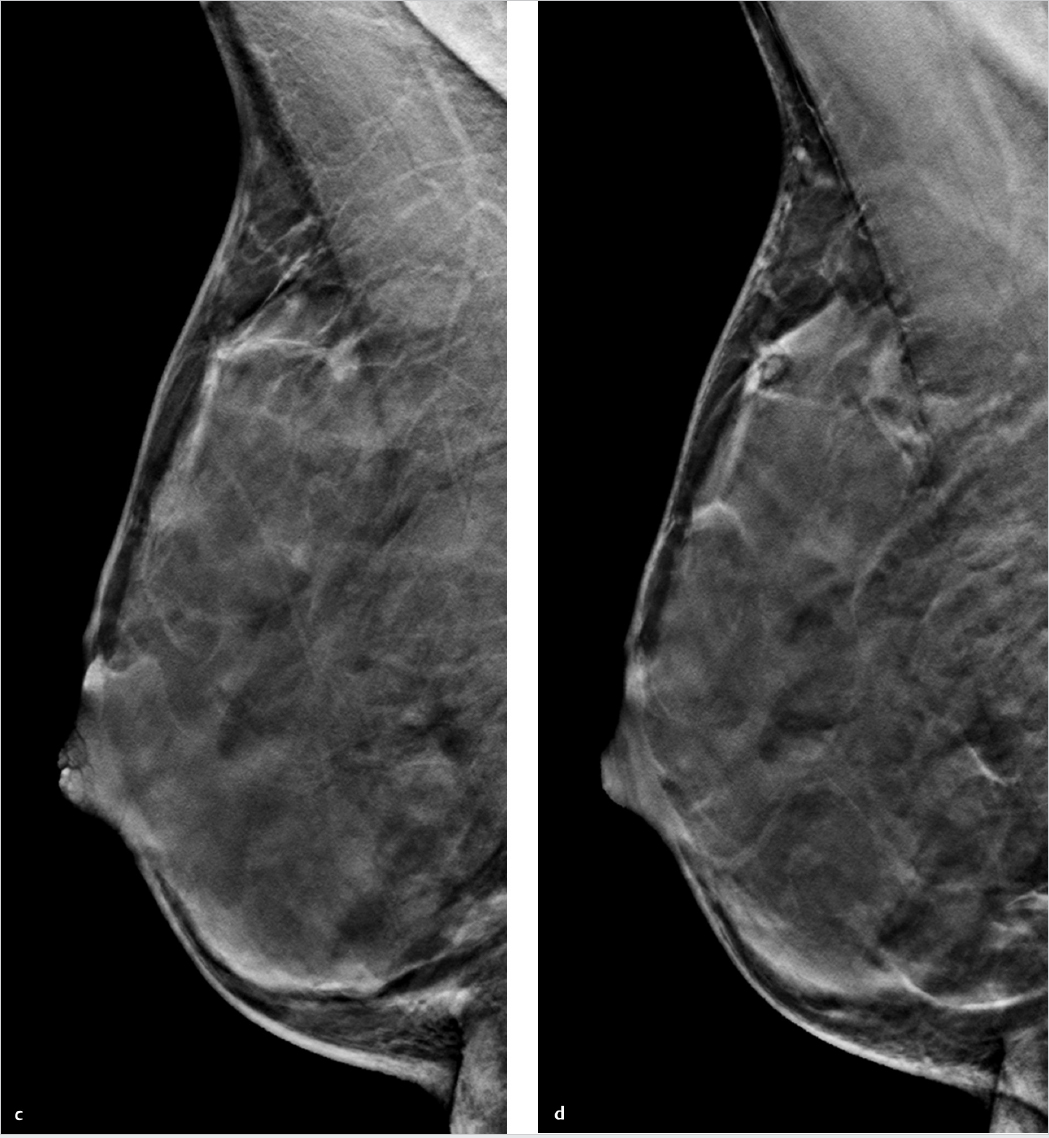
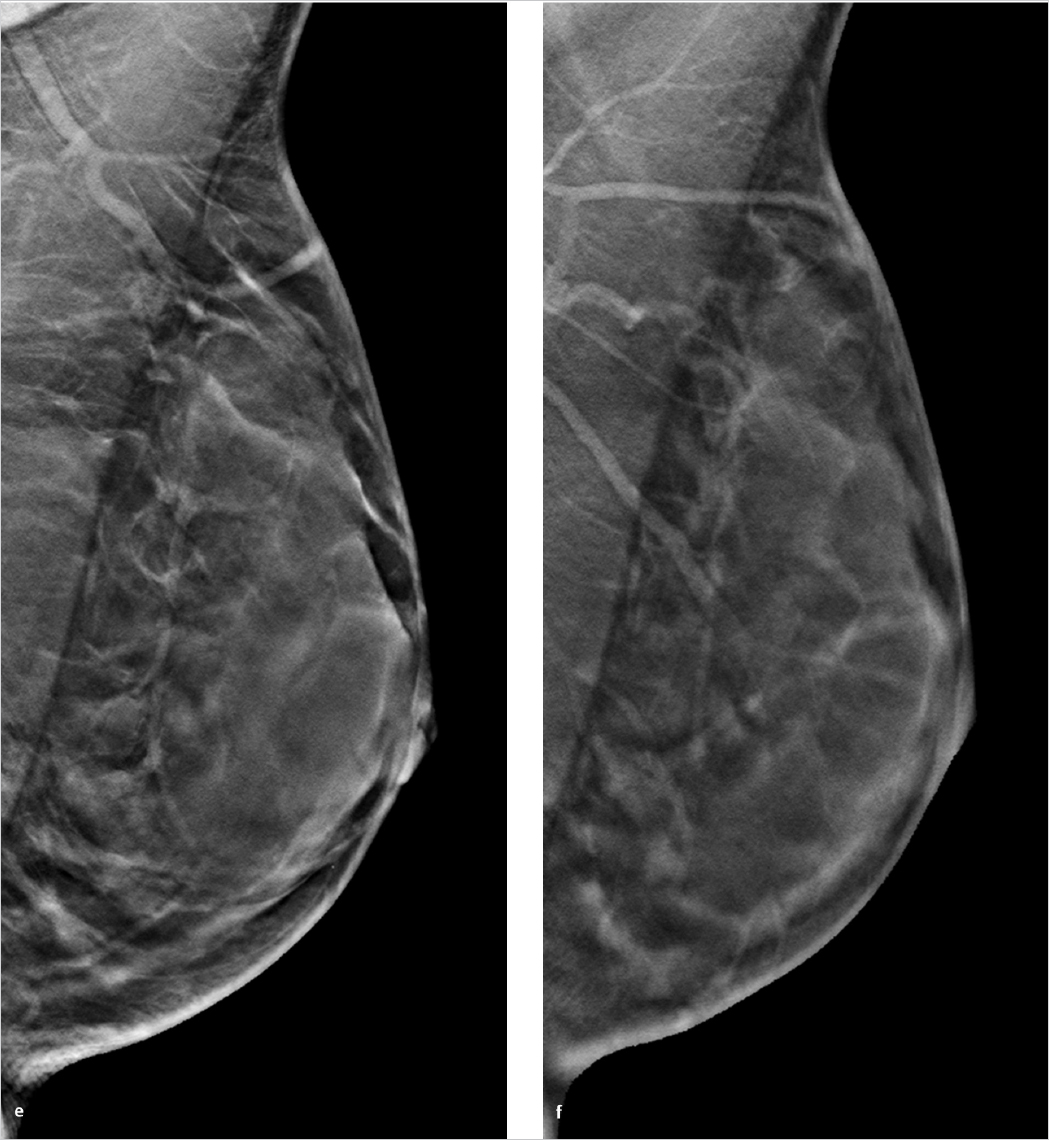
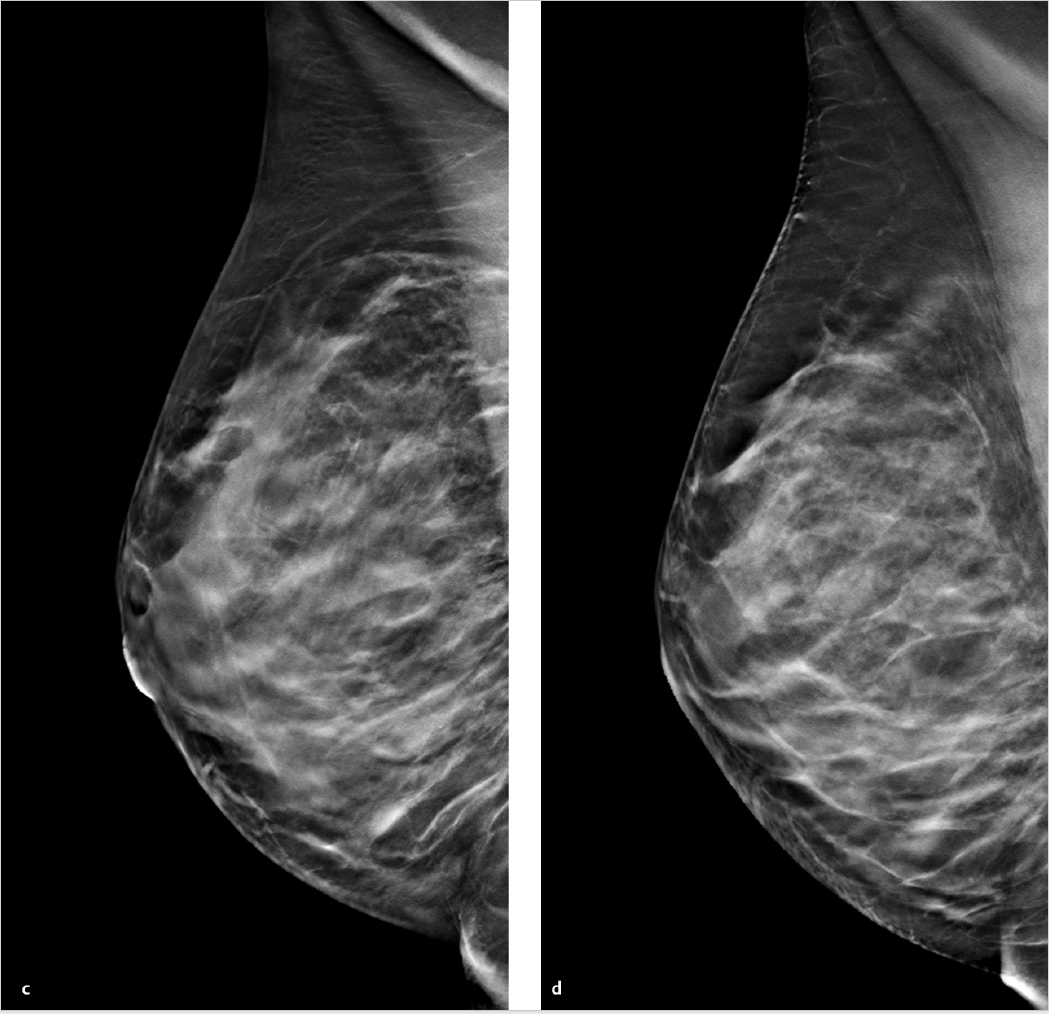
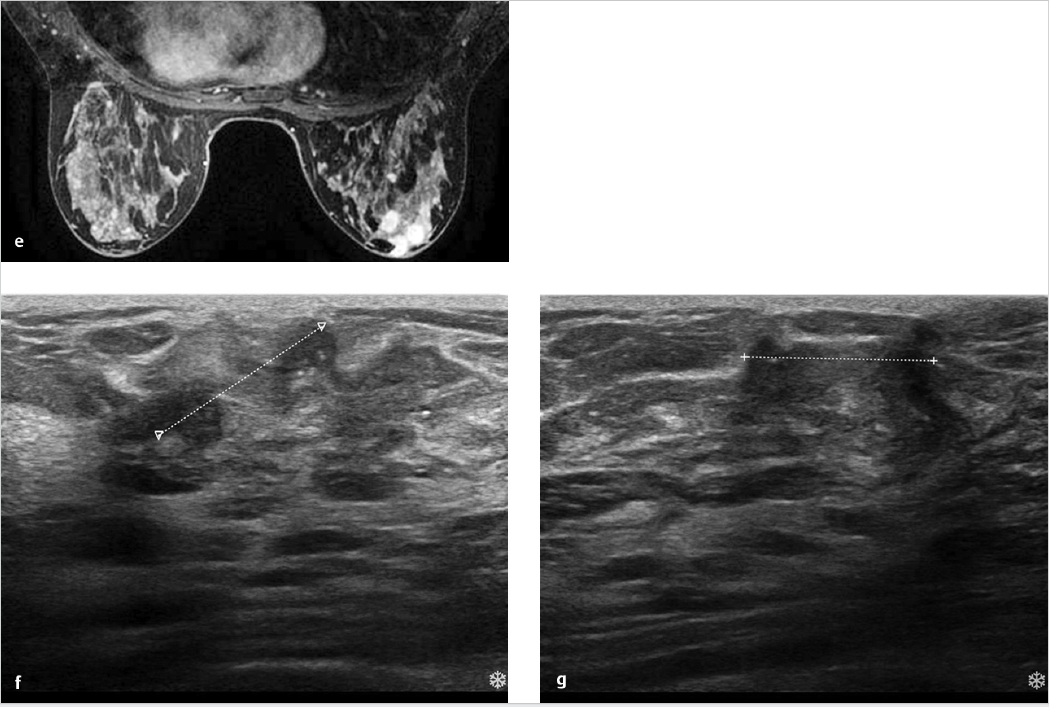
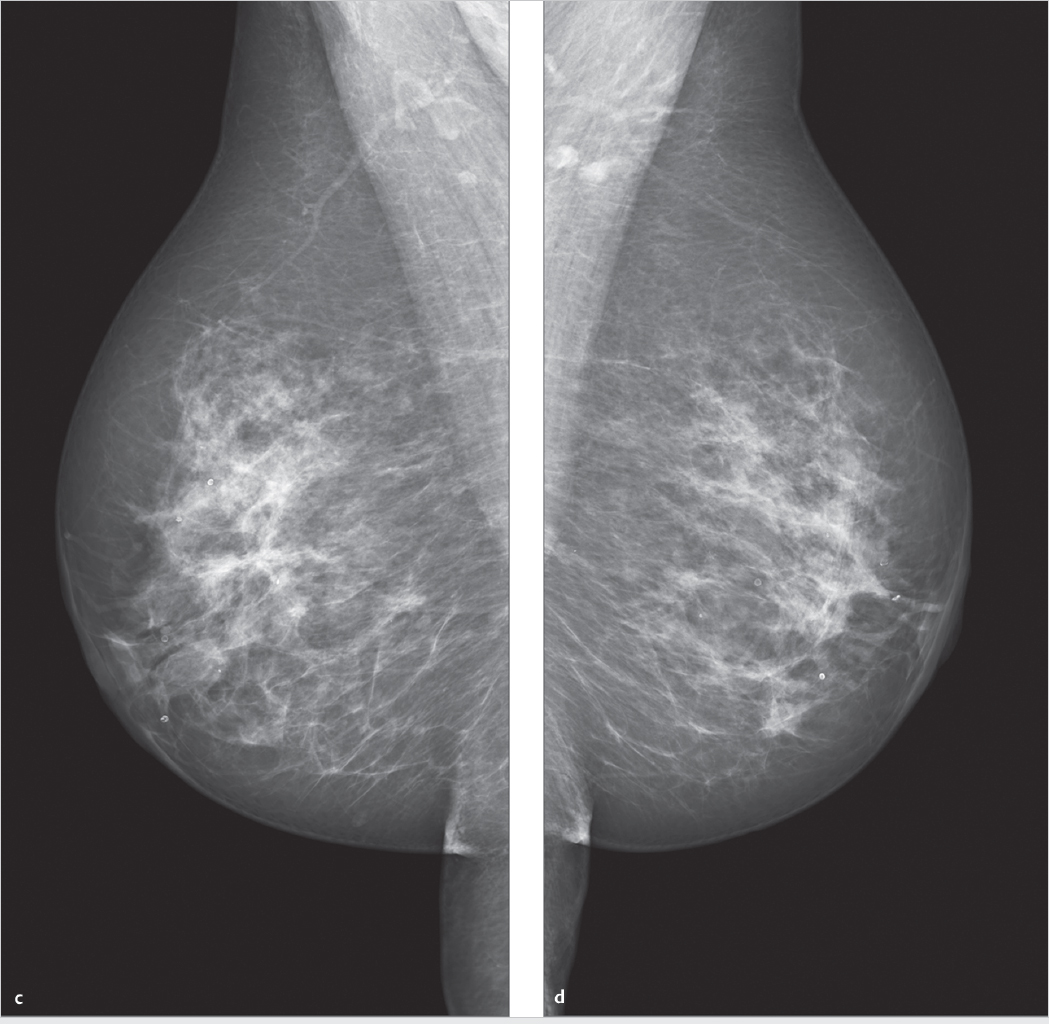
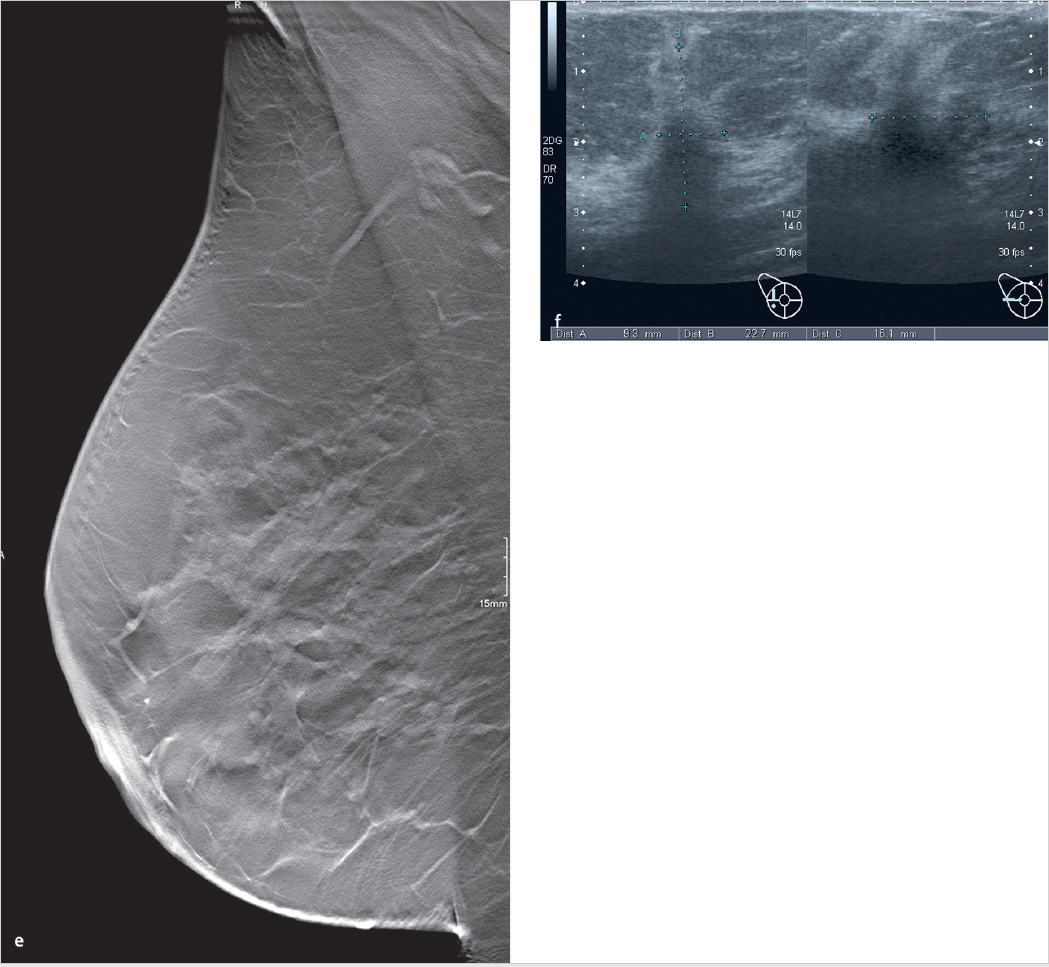
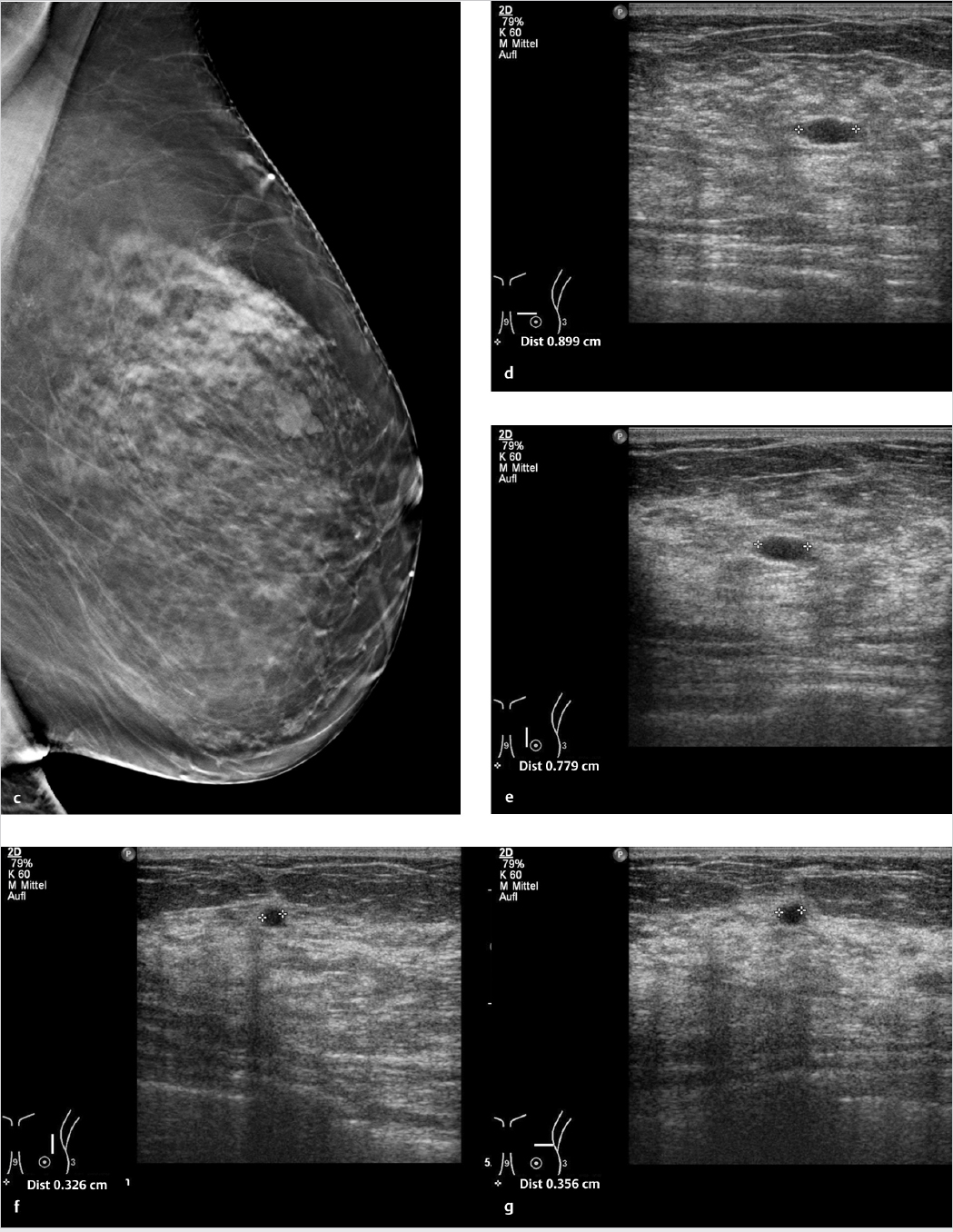
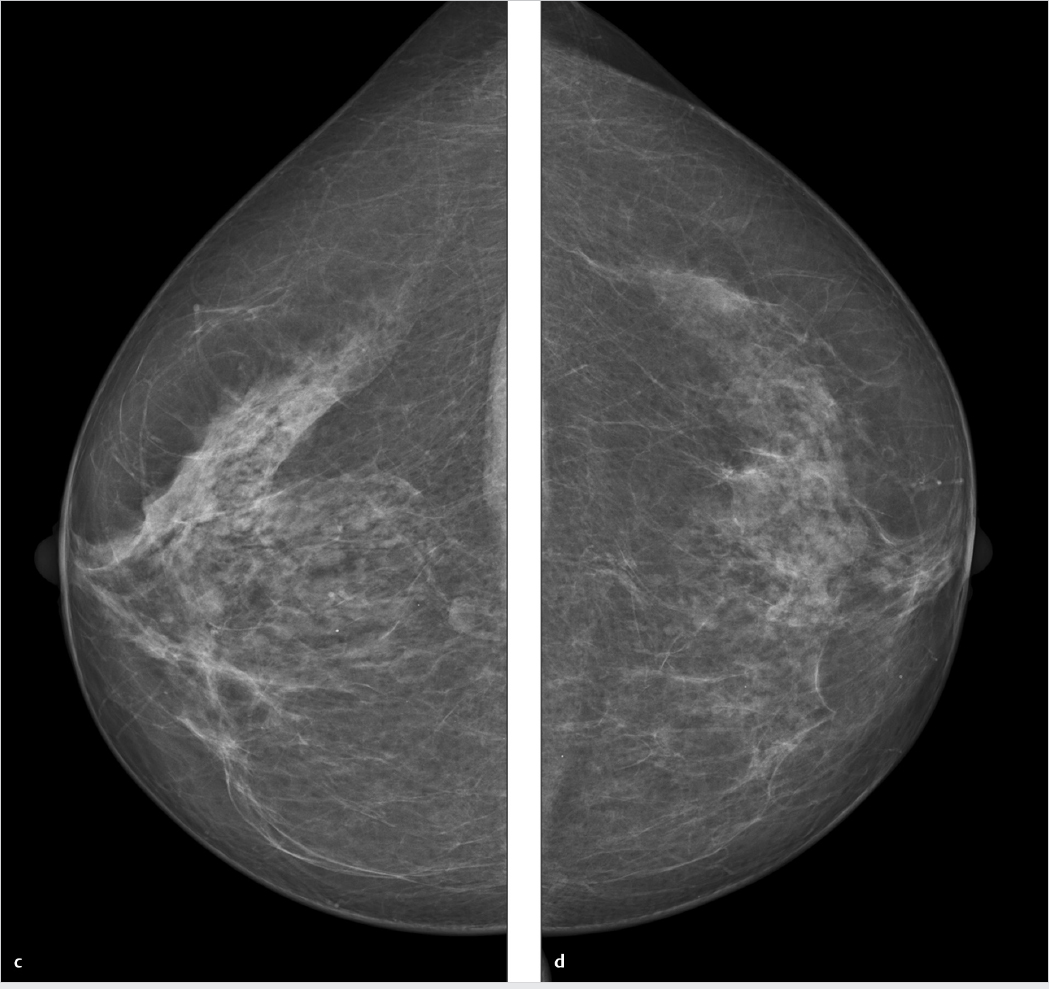
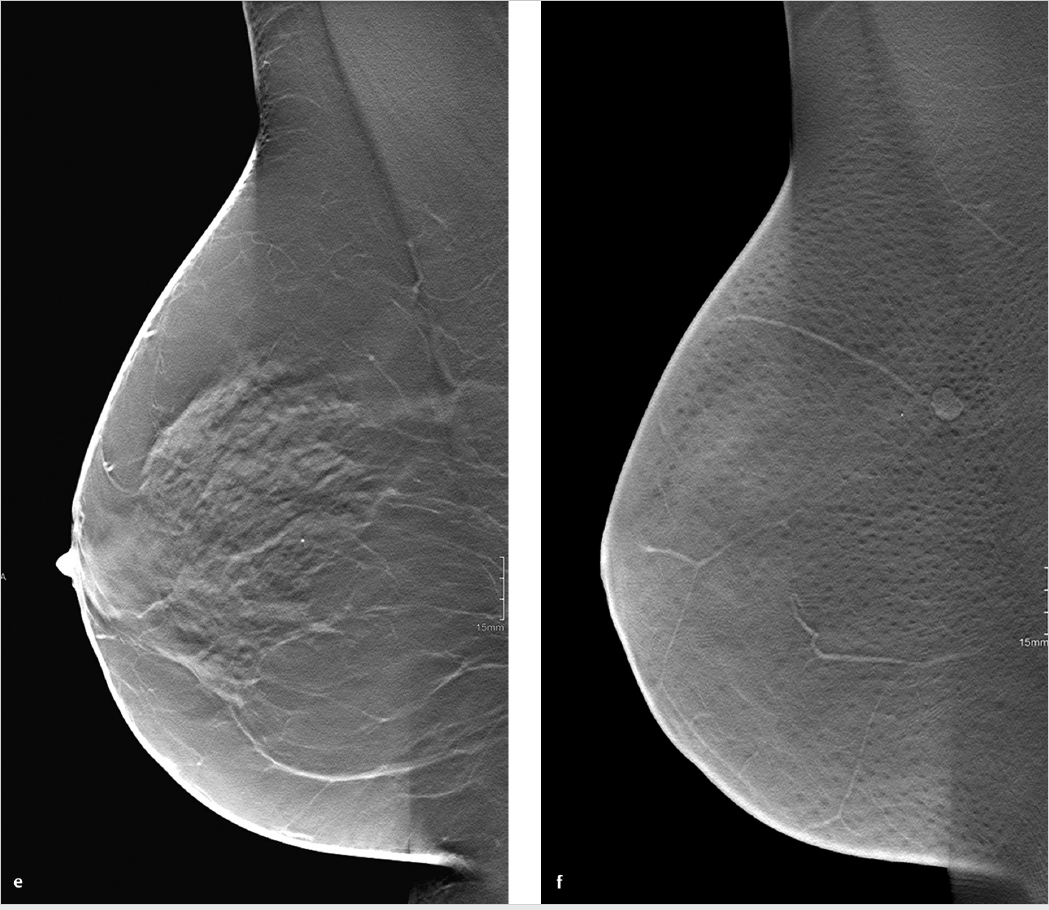
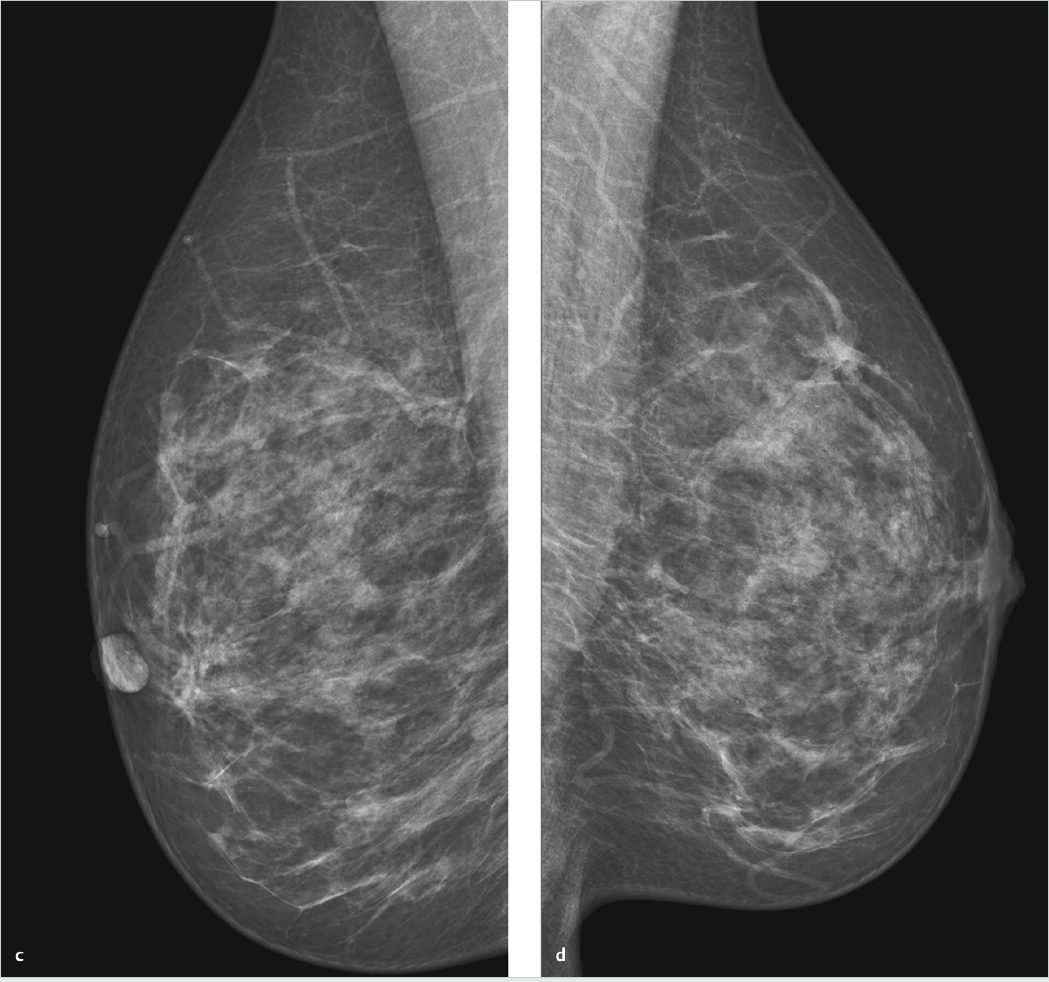
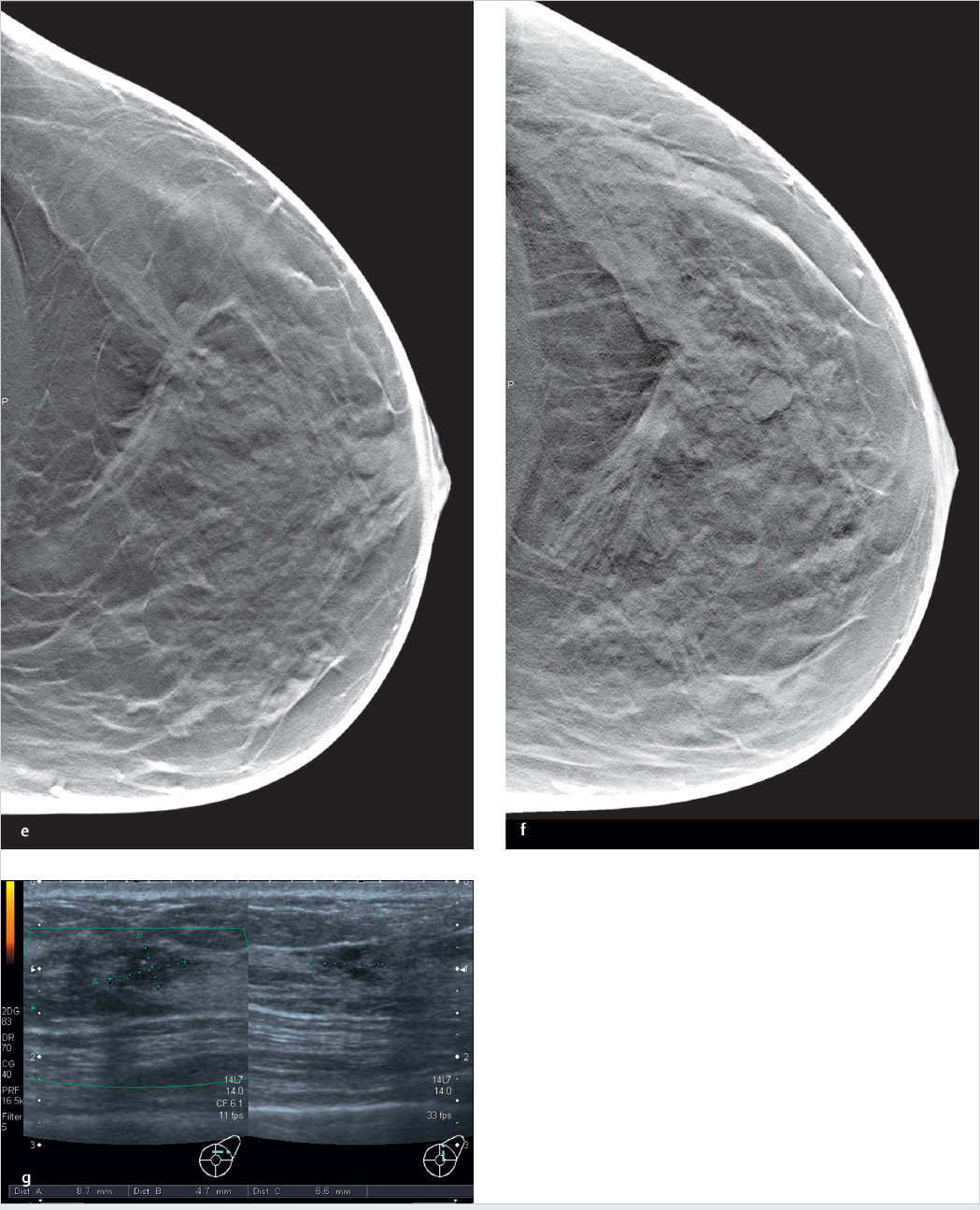
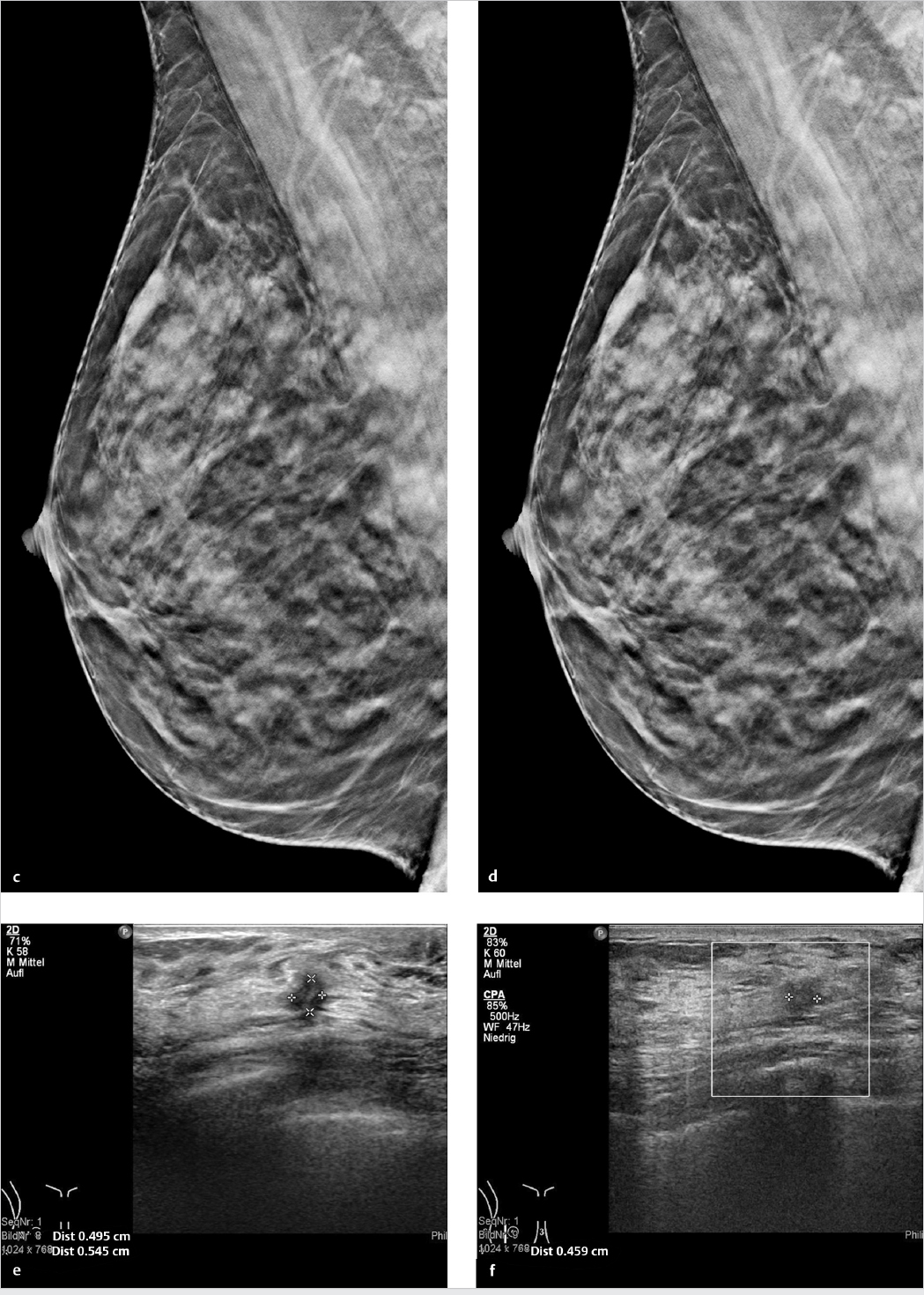
Chapter 5 The case reports in this chapter cover a range of findings that demonstrate both the capabilities and limitations of digital breast tomography. Cases imaged by multiple modalities are included, to permit a direct comparison of the findings. Note that all of the modalities in these cases were not necessary for a complete work-up, which did not follow a standard algorithm. There are several reasons why comprehensive images were available for selected cases: Some patients had already undergone various tests elsewhere before adjunctive tomosynthesis was performed, during interventional planning to establish their lesion histology. Other patients underwent more imaging studies than were strictly necessary because they were participants in clinical trials. As in the everyday practice of breast imaging, the cases are not arranged by topics. Each case is illustrated by selected, representative tomosynthesis image slices. In some cases, however, it is easier to detect lesions by scrolling through an image stack. Video sequences for nearly half the cases have been made available online, and it is always worthwhile to view the sequences that cover a complete digital breast tomosynthesis (DBT) data set. A 72-year-old woman with a family history of breast cancer. For several months, she has noticed skin dimpling at the 3 o’clock position in the left breast, with increasing local firmness. Clinical examination reveals a typical plateau sign 9 cm lateral to the nipple and a mass of approximately 2 cm fixed to the chest wall. Left breast: American College of Radiology (ACR) 3. Skin retraction is noted in the upper outer quadrant of the left breast, 9 cm from the nipple, also a 2.1-cm spiculated mass with ill-defined margins. Classified as Breast Imaging Reporting and Data System (BI-RADS) 5 (Fig. 5.1a, b). Tomosynthesis views of the left breast in the craniocaudal (CC) and mediolateral oblique (MLO) projections demonstrate a spiculated mass and skin retraction. The lesion appears less dense in the CC view than on mammograms. Classified as BI-RADS 5 (Fig. 5.1c, d). Hypoechoic mass with ill-defined margins in the left breast, measuring 20 × 11 × 12 mm. Classified as BIRADS 5. The lesion definitely correlates with clinical and mammographic findings (Fig. 5.1e, f). Ultrasound-guided core-needle biopsy was performed, identifying the lesion as grade 2 invasive carcinoma (no special type). Invasive breast carcinoma. The spiculated mass is defined much more clearly on three-dimensional (3D) tomosynthesis than on standard mammograms. In this case, tomosynthesis aids in mass detection and localization, but it does not increase sensitivity or specificity because the lesion was also visible on mammograms. Fig. 5.1 Case 1. 72-year-old woman with skin retraction. (a) Digital mammogram of the left breast, CC projection. (b) Digital mammogram of the left breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the left breast, CC projection. (d) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. (e) Ultrasound scan of the mass. (f) Ultrasound scan of the mass, second plane. Woman 41 years of age with no family history of breast cancer, not on hormone therapy. She is a primipara (P1) and breastfed for 8 months. Status post-excisional biopsy of the left breast in 2008 with benign histology. Left breast: ACR 4. Spiculated lesion visible in the MLO view, less visible in the CC view but presumably located in the upper outer quadrant. Classified as BI-RADS 4 (Fig. 5.2a, b). DBT of the left breast in the MLO projection. A lead bead has been placed to mark the suspicious area. DBT displays the spiculated lesion with much greater clarity than mammography (Fig. 5.2c, Video 5.1). Prepectoral hypoechoic area with ill-defined margins in the upper outer quadrant of the left breast, measuring 1.0 × 1.1 × 1.0 cm (Fig. 5.2d). Ultrasound-guided core-needle biopsy revealed fibrocystic changes. As this did not adequately explain the spiculated mass, stereotactic vacuum biopsy was performed. Histology showed fibrocystic changes, marked hyalinosis, and periductal fibrosis. This finding was interpreted as a radial scar and classified as a B3 lesion. Local excision was performed after stereotactic wire localization. Radial scar. This case illustrates the superiority of DBT in the detection of spiculated lesions. After the site has been marked with a lead bead, DBT can establish definite correlation of the sonographic and mammographic findings. Fig. 5.2 Case 2. 41-year-old woman, status post-excisional biopsy with benign histology. (a) Mammogram in the CC projection. (b) Mammogram in the MLO projection. (c) Representative tomosynthesis slice, MLO projection. (d) Ultrasound scans of the lesion. Asymptomatic 60-year-old woman with a family history of breast cancer, 9 years after excisional biopsy of the left breast for atypical ductal hyperplasia. Right breast: ACR 3. Moderately coarse pattern of fibrocystic changes. CC projection shows a 5-mm area of slightly increased retroareolar density approximately 3 cm from the nipple (Fig. 5.3a), not visible in the oblique view (Fig. 5.3b). Classified as BI-RADS 4. CC and MLO tomosynthesis views of the right breast demonstrate a spiculated mass located approximately 3 cm behind the nipple. Classified as BI-RADS 5 (Fig. 5.3c, d). Hypoechoic mass with ill-defined margins in the right breast, measuring 6 × 3 × 3 mm, consisting of two parts. The lesion correlates with the mammographic findings. Classified as BI-RADS 5. (Fig. 5.3e, f). Ultrasound-guided core-needle biopsy of the right breast identified the lesion histologically as a 7-mm grade 2 carcinoma of the invasive lobular type. Invasive lobular carcinoma. Only one mammographic view shows an area of increased density, while tomosynthesis clearly demonstrates a spiculated mass. In this case, then, tomosynthesis provides better lesion detection and characterization than mammography. Fig. 5.3 Case 3. 60-year-old woman, status post-excisional biopsy for atypical ductal hyperplasia. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the right breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the right breast, CC projection. (d) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (e) Ultrasound scan of the mass. (f) Ultrasound scan of the mass, second plane. Woman 44 years of age with no family history of breast cancer, not on hormone therapy. She is a primigravida (G1), P1, and breastfed for 6 months. Right breast: ACR 2. Spiculated mass in the upper outer quadrant, classified as BI-RADS 4 (Fig. 5.4a, c). Additional suspected intramammary lymph node. Left breast: ACR 2. Classified as BI-RADS 2 (Fig. 5.4b, d). CC view shows a spiculated mass in the upper outer quadrant of the right breast (Fig. 5.4e) and an intramammary lymph node (Fig. 5.4f, Video 5.2). Ultrasonography does not show a correlate for the mammographic lesion. The mass was investigated by stereotactic core-needle biopsy. Moderately differentiated carcinoma (no special type) with associated ductal carcinoma in situ (DCIS). Both the benign and malignant breast lesions can be accurately detected and characterized by tomosynthesis. Video 5.2 Case 4. DBT data set of the right breast, CC projection. Spiculated mass and intramammary lymph node. Fig. 5.4 Case 4. Screening examination of a 44-year-old woman. (a) Digital mammogram of the right breast, CC projection. ACR 2. Spiculated mass in the upper outer quadrant. Suspected intramammary lymph node. (b) Digital mammogram of the left breast, CC projection. (c) Digital mammogram of the right breast, MLO projection. (d) Digital mammogram of the left breast, MLO projection. (e) DBT of the right breast, CC projection. (f) DBT of the right breast, CC projection. Follow-up of an asymptomatic 78-year-old woman 7 years after diagnosis of DCIS. She has a known, firm, only slightly mobile 1.5-cm mass at the 2 o’clock position in the left breast. The mass is located 6 cm from the nipple, within a scarred area. No other clinical abnormalities. Left breast: ACR 2. Architectural distortion is present in the upper outer quadrant, owing to scarring. A 1.8-cm lucency with smooth margins and shell-like calcifications is visible in the scarred area. The mammographic architectural distortion correlates with the palpable mass and represents known liponecrosis. Vascular calcification is also noted. BI-RADS 2 (Fig. 5.5a, b). DBT of the left breast in the MLO projection. A scarred area after segmental mastectomy appears as an architectural distortion. The scarred region contains a typically well-circumscribed area of liponecrosis with central lucency and shell-like calcifications. Vascular calcification is also found. Classified as BI-RADS 2 (Fig. 5.5c, d). Liponecrosis at the segmental mastectomy site. Tomosynthesis provides excellent delineation of the lipo-necrosis (oil cyst) in the scarred area. The 3D technique provides views that are not obscured by superimposed tissues. Fig. 5.5 Case 5. Follow-up imaging of a 78-year-old woman with a history of DCIS. (a) Digital mammogram of the left breast, CC projection. (b) Digital mammogram of the left breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. (d) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. Asymptomatic 71-year-old woman with no visible or palpable abnormalities in either breast. Status post-ovarian cancer 10 years earlier. Right breast: ACR 3. Nodular pattern of fibrocystic changes. A 5-mm prepectoral mass is visible in the upper outer quadrant at the 11 o’clock position, 5 cm from the nipple, and has partially irregular margins. Classified as BI-RADS 4 (Fig. 5.6a, b). MLO view of the right breast shows an elliptical mass with smooth margins and central lucency, typical of a nonspecific lymph node. Right breast is reclassified as BIRADS 2 (Fig. 5.6c). Nonspecific right intramammary lymph node. The mass is clearly visualized by supplemental 3D tomosynthesis. DBT improves specificity in this case and permits downgrading of the BI-RADS 4 mammographic lesion to BI-RADS 2. Fig. 5.6 Case 6. Screening examination of a 71-year-old woman. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the right breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. Asymptomatic 51-year-old woman. G1, P1, did not breastfeed. She has an older sister diagnosed with breast cancer at age 50 years. Patient is not on hormone therapy. Right breast: ACR 3. No mass or microcalcifications. Classified as BI-RADS 2 (Fig. 5.7a, c). Left breast: ACR 3. Central, questionable spiculated lesion in the CC view with no visible correlate in the MLO view. Classified as BIRADS 4 (Fig. 5.7b, d). Tomosynthesis shows a definite spiculated lesion in the upper central breast (Fig. 5.7e, Video 5.3). Hypoechoic mass with ill-defined margins in the upper breast, 1.3 × 0.9 × 0.4 cm (Fig. 5.7f). Ultrasound-guided core-needle biopsy identified the mass as moderately differentiated invasive lobular carcinoma, which was marked with a clip after the intervention. Final diagnosis after segmental mastectomy: 1.8-cm invasive lobular carcinoma accompanied by foci of atypical lobular hyperplasia. Invasive lobular carcinoma. The mammograms were interpreted externally by two experienced readers. One scored the images as BI-RADS 2, the other as BI-RADS 4. This prompted a recall for further evaluation. The spiculated lesion can be detected more easily and confidently on tomosynthesis than on mammography. In this case, however, breast ultrasonography would also have been sufficient to confirm the diagnosis. Video 5.3 Case 7. DBT data set of the left breast, CC projection. Spiculated lesion in the upper central portion of the breast. Fig. 5.7 Case 7. Screening examination of a 51-year-old woman. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the left breast, CC projection. (c) Digital mammogram of the right breast, MLO projection. (d) Digital mammogram of the left breast, MLO projection. (e) Single slice from 3D tomosynthesis data set of the left breast, CC projection. (f) Ultrasound scans of the mass. Asymptomatic woman with three children, each breastfed for 3 months. She has no family history of breast cancer and is on transdermal hormone replacement therapy (HRT). No palpable masses or enlarged locoregional lymph nodes. Well-healed scars are present from previous bilateral open breast biopsies (2000). Right breast: ACR 3. Skin and nipple appear normal. No suspicious mammographic masses or suspicious micro-calcifications. Classified as BI-RADS 1 (Fig. 5.8a, c). Left breast: ACR 3. Skin and nipple appear normal. CC projection shows an 8-mm mass in the medial half of the left breast, 4 cm from the nipple. No visible correlate in the MLO projection. No suspicious microcalcifications. Classified as BI-RADS 4 (Fig. 5.8b, d). Targeted ultrasound scans of the left breast show a mass in the lower inner quadrant, measuring 6.6 × 5.2 × 7.6 mm, with central internal echoes and no architectural distortion (Fig. 5.8e). Lesion location was marked on the skin with a lead bead marker. DBT of the left breast with the skin marker in place. CC view demonstrates an elongated, low-density mass with predominantly smooth margins located close to the marker (Fig. 5.8f). A similar mass is found at a more cranial level in the same region (Fig. 5.8g). The images suggest a low index of suspicion. Classified as BI-RADS 3 (Video 5.4). Based on the suspicious mammographic mass and its ultrasonographic correlate, detailed informed consent was obtained for an ultrasound-guided core-needle biopsy of the left breast. Histology revealed adenosis, ordinary ductal hyperplasia, columnar cell metaplasia, and focal oncocytic metaplasia, with no evidence of malignancy (B2). The findings were unchanged at 1-year follow-up. Fibrocystic changes with no evidence of malignancy. The suspicious mammographic mass was identified as a summation artifact on tomosynthesis, but the patient still wanted a definitive histologic diagnosis. In retrospect, and based on growing experience with tomosynthesis, biopsy could have been withheld in the present case. Video 5.4 Case 8. DBT data set of the left breast, CC projection with a lead bead marker. Two well-circumscribed, elongated low-density lesions. Fig. 5.8 Case 8. Asymptomatic patient had previous bilateral open biopsies with benign results. (a) Digital mammogram of the right breast, MLO projection. (b) Digital mammogram of the left breast, MLO projection. (c) Digital mammogram of the right breast, CC projection. (d) Digital mammogram of the left breast, CC projection. (e) Ultrasound scans of the mass. (f) Single slice from 3D tomosynthesis data set of the left breast, CC projection. (g) Single slice from 3D tomosynthesis data set of the left breast, CC projection. Asymptomatic 74-year-old woman. G2, P1, breastfed for 6 months. No family history of breast cancer, no hormone therapy. No palpable masses. The right breast has been smaller than the left for many years. Right nipple retraction has been present for approximately 6 months. Right breast: ACR 2. CC view shows a spiculated lesion in the outer half of the breast and a retroareolar density with architectural distortion. Classified as BI-RADS 4 (Fig. 5.9a, c). Left breast: ACR 2. No focal lesions. Classified as BI-RADS 2 (Fig. 5.9b, d). DBT of the right breast in the CC projection. The mammographic lesion in the lower outer quadrant appears on tomosynthesis as an ill-defined mass with radiating spicules (Fig. 5.9e). DBT also shows an ill-defined retroareolar density measuring up to 1.5 cm in its largest dimension (Fig. 5.9f). Overall classification is BI-RADS 5 (Video 5.5). Scans of the right breast show a hypoechoic retroareolar mass with irregular margins, measuring 1.1 × 1.1 × 1.1 cm (Fig. 5.9g). Ultrasonography does not detect a mass at the site of the other mammographic density. Ultrasound-guided core-needle biopsy of the retroareolar mass in the right breast showed moderately differentiated invasive carcinoma of no special type (NST), with a small intraductal component. Classified histologically as a B5 b lesion. The mass in the lower outer quadrant was also biopsied after wire localization and proved to be a moderately differentiated invasive lobular carcinoma. Moderately differentiated invasive carcinoma NST in the retroareolar area of the right breast, plus moderately differentiated invasive lobular carcinoma in the lower outer quadrant. The retroareolar lesion is best demonstrated by ultrasonography, while the lesion in the lower outer quadrant is most accurately detected and characterized by tomosynthesis. This case illustrates the value of breast ultrasonography and tomosynthesis as complementary modalities. Video 5.5 Case 9. DBT data set of the right breast, CC projection. Ill-defined lesion with radiating spicules in the lower outer quadrant of the breast, plus an ill-defined retroareolar density up to 1.5 cm in its largest dimension. Fig. 5.9 Case 9. Screening examination of a 74-year-old woman. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the left breast, CC projection. (c) Digital mammogram of the right breast, MLO projection. (d) Digital mammogram of the left breast, MLO projection. (e) Single slice from 3D tomosynthesis data set of the right breast, CC projection. (f) Single slice from 3D tomosynthesis data set of the right breast, CC projection. (g) Ultrasound scans of the mass. A 42-year-old woman with significant bilateral fibrocystic breast changes and right mastodynia. No family history of breast cancer. No visible abnormalities. Palpable findings are consistent with fibrocystic changes. Bilateral mammograms in the CC projection. Both breasts are classified as ACR 4. Images show a fibrocystic parenchymal pattern with increased radiographic density. No masses or microcalcifications are seen. Both breasts are classified as BI-RADS 2 (Fig. 5.10a, b). Bilateral DBT in the MLO projection. Tomosynthesis also shows significant bilateral fibrocystic changes with increased parenchymal density. Both breasts are classified as BI-RADS 2 (Fig. 5.10c–f). No suspicious masses in either breast. Significant bilateral fibrocystic changes. BI-RADS 2. In this patient with very dense breast parenchyma, only one mammographic view was obtained (CC) and this was supplemented by tomosynthesis in the MLO projection. With this combination, which has been investigated in several studies, mammography can detect microcalcifications, while complementary-view tomosynthesis can detect or exclude masses. Ultrasonography is also a necessary adjunct, however, even when tomosynthesis is used. Fig. 5.10 Case 10. Significant fibrocystic changes in a 42-year-old woman. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the left breast, CC projection. (c) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (d) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (e) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. (f) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. A 42-year-old woman found three palpable masses in the periareolar region during breast self-examination. Clinical examination finds corresponding firm masses up to 1 cm in size, suspicious for malignancy, in the periareolar region of the right breast. They are located at the 5o’clock, 9 o’clock, and 11 o’clock positions. Right breast: ACR 4. Patchy fibrocystic changes with no evidence of masses or microcalcifications. Right breast changes are classified as BI-RADS 2 (Fig. 5.11a, b). DBT of the right breast in the MLO projection. Supplemental tomosynthesis of the right breast shows no abnormalities at the location of the palpable masses. Classified as BI-RADS 2 (Fig. 5.11c, d). MRI of the right breast demonstrates the three periareolar lesions as spiculated masses with suspicious enhancement and rapid washout (Fig. 5.11e). On ultrasound scans of the right breast, the three suspicious palpable masses appear as hypoechoic lesions with ill-defined margins that coincide precisely with the clinical findings. Classified as BI-RADS 5 (Fig. 5.11f, g). The three masses were investigated by ultrasound-guided core-needle biopsy, which identified each lesion as grade 2 invasive carcinoma NST. Their individual sizes were determined histologically as 7, 8, and 11 mm. Multifocal invasive carcinoma NST. Ultrasonography and MRI are the only modalities that showed abnormalities at the sites of the three palpable masses. Owing to the high radiographic density of the breast parenchyma (ACR 4), neither mammography nor tomosynthesis could detect the lesions in this patient. Both techniques were false negative because even in DBT, lesion detection requires a density difference between the tumor and surrounding tissue. Tomosynthesis cannot exclude tumors in dense glandular tissue, and an accurate diagnosis in these cases always requires additional evaluation by ultrasonography. Fig. 5.11 Case 11. 42-year-old woman with palpable masses found on breast self-examination. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the right breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (d) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (e) MRI of the right breast: axial T 1-weighted sequence after contrast administration. (f) Ultrasound scan of the masses (12.5-MHz probe). (g) Ultrasound scan of the masses, second plane. Asymptomatic 71-year-old woman. G1, P1, breastfed for several weeks. Patient is on HRT. No family history of breast cancer. Localized firmness of the right breast is noted at the 9 o’clock position, with associated skin retraction when the arm is raised. Right breast: ACR 3. MLO projection shows areas of lipoid necrosis plus architectural distortion in the upper outer quadrant. CC projection shows asymmetry but no definite correlate with the MLO findings. Classified as BI-RADS 4 (Fig. 5.12a, c). Left breast: ACR 3. No mammographic lesions. Multiple sites of lipoid necrosis. Classified as BIRADS 2 (Fig. 5.12b, d). MLO view of the right breast confirms the architectural distortion, which is best appreciated by scrolling through the complete DBT data set. Classified as BI-RADS 4 (Fig. 5.12e, Video 5.6). Ultrasound scans of the right breast demonstrate an irregular hypoechoic mass with ill-defined margins at the 9o’clock position, measuring 0.9 × 2.2 × 1.6 cm. Suspected tumor spicules radiate to the skin (Fig. 5.12f). Ultrasound-guided core-needle biopsy identified the mass as poorly differentiated invasive carcinoma. Treatment consisted of breast-conserving surgery and adjuvant radiotherapy. Poorly differentiated carcinoma NST 3 cm in diameter. The architectural distortion in this case is particularly well demonstrated by scrolling through the tomosynthesis data set. Ultrasonography is best for tumor detection. All the modalities underestimated tumor size relative to actual histologic size. Fig. 5.12 Case 12. 71-year-old woman with localized firmness and skin retraction on elevation of the arm. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the left breast, CC projection. (c) Digital mammogram of the right breast, MLO projection. (d) Digital mammogram of the left breast, MLO projection. (e) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (f) Ultrasound scans of the mass. A 59-year-old woman has a family history of breast cancer and known fibrocystic changes. She has no complaints and no visible or palpable abnormalities in either breast. Left breast: ACR 3. A mass measuring 8 × 9 mm, partially obscured by parenchyma but elsewhere showing relatively smooth margins, is located approximately 5 cm from the nipple at the 11 o’clock position. A second, smaller mass of similar shape, 4 mm in diameter, is located 6 cm from the nipple at the 1 o’clock position. Both lesions are classified mammographically as BI-RADS 4 (Fig. 5.13a, b). DBT of the left breast in the MLO projection. Both masses have completely smooth margins by tomosynthesis and are downgraded to BI-RADS 2 (Fig. 5.13c). Ultrasound scans of the left breast show two well-circumscribed, elliptical, echo-free masses at the 11 o’clock and 1o’clock positions. The lesion at the 11 o’clock position measures 9 × 8 mm and shows posterior echo enhancement (Fig. 5.13d, e). The lesion at the 1 o’clock position measures 3 × 4 mm (Fig. 5.13f, g). Classified as BI-RADS 2. BI-RADS 2, benign breast cysts. Tomosynthesis allows a more precise characterization of focal lesions than mammography because the margins are not obscured by superimposed parenchyma. Several large studies have confirmed that tomosynthesis can lower recall rates in screening. Ultrasonography in the present case confirms the tomosynthesis findings and is unquestionably the preferred technique for evaluating breast cysts. Compared with the combination of mammography and ultrasonography, tomosynthesis provides no additional information for the detection and characterization of breast cysts. Fig. 5.13 Case 13. Fibrocystic breast changes in a 59-year-old woman. (a) Digital mammogram of the left breast, CC projection. (b) Digital mammogram of the left breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the left breast, MLO projection. (d) Ultrasound scan of the mass at the 11 o’clock position (12.5-MHz probe). (e) Ultrasound scan of the mass at the 11 o’clock position (12.5-MHz probe), second plane. (f) Ultrasound scan of the mass at the 1 o’clock position. (g) Ultrasound scan of the left breast mass at the 1 o’clock position, second plane. Woman 57 years of age, three children, did not breast-feed. No family history of breast cancer. Left mastodynia has been present for several months. No palpable abnormalities. Right breast: ACR 2. Retroareolar architectural distortion with a subtle spiculated lesion, not visible in the CC view. Scattered microcalcifications. Small, well-circumscribed mass near the chest wall. Classified as BI-RADS 3 (Fig. 5.14a, c). Left breast: ACR 2. No masses or suspicious microcalcifications (Fig. 5.14b, d). MLO view of the right breast shows no evidence of a spiculated lesion or suspicious mass (Fig. 5.14e). The small, well-circumscribed mass at skin level is identified as a skin wart (Fig. 5.14f, Video 5.7). No evidence of a mass. Normal findings, classified as BI-RADS 2. The findings were unchanged at 2-year follow-up. Tomosynthesis can resolve the questionable spiculated lesion on mammography and can accurately localize the well-circumscribed lesion to skin level. Video 5.7 Case 14. DBT data set of the right breast, MLO projection. Small mass with smooth margins, a wart at skin level. Fig. 5.14 Case 14. 57-year-old woman with mastodynia. (a) Digital mammogram of the right breast, MLO projection. (b) Digital mammogram of the left breast, MLO projection. (c) Digital mammogram of the right breast, CC projection. (d) Digital mammogram of the left breast, CC projection. (e) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (f) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. Woman 48 years of age with no family history of breast cancer, not on hormone therapy. G2, P2, did not breast-feed. Status post-excisional biopsy of the left breast in 1996 with benign histology. Right breast: ACR 3. A benign-appearing lesion is seen in the lower outer quadrant, classified as BI-RADS 2 (Fig. 5.15a, c). Left breast: ACR 3. A 1-cm spiculated mass is found in the upper outer quadrant, 5.7 cm from the nipple. It is accompanied by scattered microcalcifications and additional masses whose margins are difficult to evaluate. The spiculated lesion is classified as BI-RADS 4 (Fig. 5.15b, d). CC view of the left breast shows a 1-cm spiculated mass 6 cm from the nipple, with scattered microcalcifications (Fig. 5.15e). Multiple masses with smooth margins are also visible (Fig. 5.15f, Video 5.8). Ultrasound scan of the left breast shows an irregularly shaped hypoechoic mass at the 12 o’clock position, measuring 0.9 × 0.5 × 0.7 cm (Fig. 5.15 g). Vacuum biopsy of the mass gave a histologic diagnosis of focal atypical epithelial hyperplasia and an intraductal papilloma. Owing to the B3 classification, the lesions were surgically excised. Atypical ductal hyperplasia and intraductal papilloma. Tomosynthesis confirms the mammographically suspicious lesion. The other mammographic densities are definitely characterized as benign by DBT. Video 5.8 Case 15. DBT data set of the left breast, CC projection. Multiple smooth-bordered masses plus a 1-cm spiculated mass 6 cm from the nipple, with scattered micro-calcifications. Fig. 5.15 Case 15. 48-year-old woman, status post-excisional biopsy with benign histology. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the left breast, CC projection. (c) Digital mammogram of the right breast, MLO projection. (d) Digital mammogram of the left breast, MLO projection. (e) Single slice from 3D tomosynthesis data set of the left breast, CC projection. (f) Single slice from 3D tomosynthesis data set of the left breast, CC projection. (g) Ultrasound scans of the mass in the left breast. Asymptomatic 58-year-old woman with a family history of breast cancer and known significant fibrocystic changes. Both breasts have palpable nodularity but no other abnormalities. Right breast: ACR 4. Nodular pattern of fibrocystic changes with scattered, monomorphic microcalcifications. Suspicious masses are not seen in either the CC or MLO views. Classified as BI-RADS 2 (Fig. 5.16a, b). MLO view of the right breast shows subtle retroareolar spiculations 2 cm from the nipple, with an associated mass measuring approximately 5 × 5 mm. Classified as BIRADS 4 (Fig. 5.16c, d). Ultrasound scans of the right breast show a periareolar hypoechoic area with ill-defined margins and associated architectural distortion. It measures 5 × 5 × 5 mm. Classified as BI-RADS 5 (Fig. 5.16e, f). Ultrasound-guided core-needle biopsy identified the mass as a grade 1 carcinoma, 5 mm in diameter. Grade 1 invasive breast carcinoma NST. The spiculated mass is detected by tomosynthesis but not by mammography. The use of 3D tomosynthesis in this case increases sensitivity and allows detection of a breast cancer that is occult on standard mammograms. Fig. 5.16 Case 16. 58-year-old woman with significant fibrocystic changes and palpable nodularity in both breasts. (a) Digital mammogram of the right breast, CC projection. (b) Digital mammogram of the right breast, MLO projection. (c) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (d) Single slice from 3D tomosynthesis data set of the right breast, MLO projection. (e) Ultrasound scan of the mass. (f) Ultrasound scan of the mass, second plane.
Illustrative Case Reports
5.1 Introduction
5.2 Cases
5.2.1 Case 1
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.2 Case 2
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.3 Case 3
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.4 Case 4
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.5 Case 5
History
Mammography
DBT
Final Diagnosis
Discussion
5.2.6 Case 6
History
Mammography
DBT
Final Diagnosis
Discussion

5.2.7 Case 7
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.8 Case 8
History
Mammography
Ultrasonography
DBT
Further Case History
Final Diagnosis
Discussion
5.2.9 Case 9
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.10 Case 10
History
Mammography
DBT
Ultrasonography
Final Diagnosis
Discussion
5.2.11 Case 11
History
Mammography
DBT
Breast Magnetic Resonance Imagining (MRI)
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.12 Case 12
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.13 Case 13
History
Mammography
DBT
Ultrasonography
Final Diagnosis
Discussion
5.2.14 Case 14
History
Mammography
DBT
Ultrasonography
Final Diagnosis
Further Case History
Discussion
5.2.15 Case 15
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
5.2.16 Case 16
History
Mammography
DBT
Ultrasonography
Further Case History
Final Diagnosis
Discussion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree