Age
Condition
<18 years
Spondylolysis/spondylolisthesis
Scheuermann disease
18–50 years
Acute lumbago/acute cervicalgia
Internal disk disruption
>50 years
Chronic lumbago/facet osteoarthopathy
Lumbar stenosis
Osteoporosis and compression fracture
It is important for physicians dealing with athletes suffering from back or neck pain to understand the differences between serious and mild spinal injuries. In order to make a precise diagnosis, a good knowledge of the basic anatomy of the spine and its related structures, familiarity with mechanisms of injury and common causes of back and neck pain, and a thorough understanding of the clinical presentation of the disorders in these areas is necessary.
10.2 Functional Anatomy
The spine can be divided in five sections: cervical (7 vertebrae), thoracic (12 vertebrae), lumbar (5 vertebrae), sacral, and coccygeal. Special units exist for the “start-”(craniocervical junction) and “end-connections” (sacroiliac junction), articulating the spine respectively with the head and with the pelvis.
Normally the cervical and lumbar spine have a lordotic curve, whereas the thoracic spine is kyphotic. The main functions of the spine are to support the head, pelvic girdle, and abdominal organs, attachment of the thorax, protection of the spinal cord, and transfer of weight and bending movements of the head, trunk, and pelvis.
The spine consists of bones, joints, ligaments, and muscles. The vertebrae are joined by joints between the bodies (disks) and the neural arches (facets). The anterior column consists of the vertebral bodies, intervertebral disks, and the anterior and posterior ligaments. Other ligaments are the inter- and supraspinous ligaments and the ligamentum flavum. The posterior column includes the neural arch, facet (zygapophyseal) joints, spinal process, and pars interarticularis (the area between the upper and lower facet joints). Important neural structures (spinal cord, conus medullaris, and cauda equine) lie within the spinal canal that runs through the vertebral foramen.
The intervertebral disks are fibrocartilaginous structures located between the vertebral bodies. It has three components: (1) the annulus fibrosus, the outer circumferential ring with collagen layers arranged in a “criss-cross” type pattern to resist torsional, axial, and tensile loads; (2) the nucleus pulposus, the central core which is composed of 70 % water, determines the disk height and provides resistance to axial compression; and (3) cartilaginous vertebral endplates.
Different muscle groups act on the spine which can be divided into (1) the anterior muscle group (interspinal, intertransverse); (2) the middle muscle group semispinalis, multifidus, and rotators; (3) the posterior muscle group (erector spinae, iliocostal thoracis, longissimus thoracis, and iliocostal lumborum); and (4) the accessory muscle group (latissimus dorsi and trapezius). The anatomy of the neck is also complex; however, it is beyond the scope of this book to give a detailed description.
10.3 Etiology and Injury Mechanism
Acute muscle strains, ligament sprains, and soft tissue contusions are a very common cause of back and neck pain in athletes (Mautner and Huggins 2012). However, most low back injuries are not the result of a single exposure to a high-magnitude load, but instead a cumulative trauma from sub-failure magnitude loads: for instance, repeated small loads (e.g., bending) or a sustained load (e.g., sitting). In particular, low back injury has been shown to result from repetitive motion at end range. Sports that use repetitive impact (e.g., running), a twisting motion (e.g., golf), or weight loading at the end of a range of motion (e.g., weightlifting), commonly cause damage to the lower back (Alexander 1985). For example, repetitive hyperextension of the low back (gymnastics, figure skating, diving) is a risk factor for the development of spondylolysis.
Contact sports such as football and ice hockey carry an inherent risk of cervical spine injury. The major mechanism of serious cervical injury is an axial load or a large compressive force applied to the top of the head (Chao et al. 2010). This mechanism is more dangerous when the neck is slightly flexed, because the spine is brought out of its normal lordotic alignment, which does not allow for proper distribution of force to the thorax. Flexion puts the cervical spine in a straight line; thus, the musculature cannot assist in absorbing the force. Injury to the cervical spine occurs when it is compressed between the body and the rapidly decelerating head. When a fracture results, if the bone fragments or herniated disk materials encroach on the spinal cord, neurologic damage will occur. This mechanism is the primary cause of cervical fracture, dislocation, and quadriplegia.
10.4 Sports Injuries
10.4.1 Sprains, Strains, and Muscle Contusions
The vast majority of back pain in the athlete occurs as a result of soft tissue sprain, strain, or contusion, and these are often a diagnosis of exclusion (Mautner and Huggins 2012). Sprain represents stretching of a ligament beyond its elastic limit. Strain is tearing of a muscle during concentric or eccentric loading. Contusion occurs after blunt trauma to the soft tissue and often leads to formation of a hematoma. These injuries are readily diagnosed based on history and clinical examination. Initially sprains, strains, and contusions can be very debilitating, but most respond to conservative management with rest, NSAIDS, and massage. Activities can be resumed when pain resolves. In case the pain does not disappear or neurological symptoms develop, further examinations should be considered.
10.4.2 Cervicalgia and Cervicobrachialgia
Most neck pain is regarded as nonspecific in the absence of radiological evidence of relevant pathoanatomy. Acute cervicalgia is characterized by a sudden onset of sharp neck pain with protective deformity and limitation of movement. It typically occurs either after a sudden, quick movement or on waking. There may have been unusual movements or prolonged abnormal postures prior to the onset of pain (Hutson and Speed 2010).
The “stinger” or “burner” phenomenon is seen frequently in American football and rugby and less often in other contact sports (Standaert and Herring 2009). The player experiences transient upper extremity burning-type pain that may also be accompanied by paresthesia and/or weakness. Traction or compression of the cervical nerve root and/or plexus brachialis is considered to be the underlying mechanism. Symptoms may be localized to the neck or may radiate to the arm and hand. The symptoms are usually transient, but persistent neurological dysfunction and recurrent stingers may occur.
10.4.3 Acute and Chronic Lumbago
Lumbago can be defined as mild to severe pain or discomfort in the area of the lower back (Patrick et al. 2014). The pain can be acute (sudden and severe) or chronic if it has lasted more than 3 months. Most people will experience lumbago at some point in their life and so do athletes. It can occur at any age but is a particular problem in younger people whose work involves physical effort and much later in life in the elderly. Athletes present with pain across the lower part of the back that sometimes radiates into the buttocks, the back of the thigh, or to the groin. The pain is usually worse on movement. There can be a tense spasm of the muscles surrounding the spine, which causes a stiff back with limitation of flexion and extension of the spine. In some severe cases, the back may tilt to one side causing a change in posture or a limp. If the pain is accompanied by a tingling sensation or numbness in the back or buttocks or leg, which may pass right down into the foot, this is called sciatica, and it indicates irritation of the sciatic nerve, which passes down from each side of the spine to the feet. In most cases it settles in a few days to weeks, but for some it is a persistent problem. In the majority of cases, it is impossible to identify the exact cause of low back pain. Due to a forceful sports-related movement, there may, for example, have been tiny strains or tears of some of the small muscles and ligaments, which can be difficult to pinpoint within the complex structure that is the human back. In most cases of lumbago, no imaging is necessary. However, in about a quarter of cases, a specific problem can be found. Often, these athletes are suffering from conditions like osteoarthritis of the facet joints, a slipped disk (prolapse of an intervertebral disk), a collapse or fracture of one or more vertebrae (especially in the elderly athletes, when they have fallen or there is a deformation of natural spine curvature (scoliosis) or more rarely, skeletal damage due to tumors or infection.
10.4.4 Intervertebral Disk Injuries With(out) Radiculopathy
Discogenic pathology is the primary cause in almost 50 % of young to middle-aged adults that complain of low back pain (LBP), whereas it is the cause of only a minority of cases in young inactive adolescents. Adolescent athletes, however, have a higher risk for internal disk disruption (IDD) than their inactive peers with back pain due to a discogenic cause in 11 % of cases (Haus and Micheli 2012; Mautner and Huggins 2012). The adolescent growth spurt appears to be the most vulnerable time for injuries to the lumbar intervertebral disk. Repetitive hyperflexion and extension loading on the lumbar disk during sports can lead to endplate irregularities, Schmörl nodes, annular tears, disk protrusions, and endplate fractures. Competitive sports and sports with more frequent trunk rotation, as, for example, gymnastics, soccer, tennis, and golf, are associated with early lumbar disk degeneration. Discogenic pain is often nonspecific. Some findings may suggest a discogenic nature of the pain: midline pain, pain with periods of unsupported sitting, and pain worsening with forward flexion. Posterior annular tears without nerve root compression can cause radicular type buttock, groin, and leg pain. On examination often there is a decreased flexibility. Neurologic deficits are absent.
In case of herniation of the nucleus pulposus with nerve root compression patients typically present with low back, buttock, or hip pain and radicular symptoms including numbness, tingling, and sharp radiating pain in the lower extremity. Pain can be made worse by coughing or sneezing. Besides a full examination of the spine, a careful neurologic examination has to be performed, looking for (subtle) deficits in strength, sensation, or reflexes. Special test like the straight leg raise and slump test can be helpful. One should realize that this classical radicular pattern might be absent in younger patients.
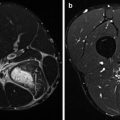
MRI allows excellent evaluation of the intervertebral disk and may show early degenerative changes including disk signal reduction, loss of height, bulging, apophyseal abnormalities, and Modic changes and its interaction with nearby structures like nerve roots (see Chap. 11). However, many asymptomatic patients will have abnormal MRI studies and this should be kept in mind. The natural history of low back pain is often favorable and the mainstay of treatment is nonsurgical. Athletes should be encouraged to remain active (activity modification), and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) as a first-line medication should be considered. Physical therapy to retrain the stabilizing spinal musculature results in less LBP recurrence.
10.4.5 Scheuermann Disease
The prevalence of Scheuermann disease is approximately 1–8 % (Haus and Micheli 2012; Lowe and Line 2007). The typical presentation is in the late juvenile age period (8–12 years). Cosmetic deformity caused by increased thoracal kyphosis is the most common complaint of patients with Scheuermann disease and is typically the primary reason for young patients to seek medical attention. The natural history remains controversial. Scheuermann disease tends to be symptomatic in the acute phase (during the teenage years) with thoracic pain worsening by activity and diminishing later in life. Patients with Scheuermann have more back pain than their healthy peers. This pain is believed not to interfere with daily activities. A recent study, however, reports a lower quality of life and more risk for disability in the activities of the daily living (Ristolainen et al. 2012).
The specific etiology remains unknown but is probably multifactorial. Genetic factors, failure in endplate ossification, chronic trauma (sports, hard labor), and hormonal factors are mentioned. Besides the most frequent “classic” Scheuermann found at the mid-thoracic spine, there also is a “lumbar” type (type II) localized at the thoracolumbar junction. This type II is typically seen in athletically active adolescent males or those involved in heavy lifting. There is a strong association with repetitive activities involving axial loading of the immature spine. In lumbar Scheuermann typically there is no kyphosis. Endplate irregularities can be more severe and can be confused with tumor, infection, or other conditions.
Imaging plays an important role in defining this condition. Radiological findings, including the typical Schmörl nodes, are discussed in Chaps. 11 and 12. Treatment of classic Scheuermann is controversial. Physical therapy is recommended and patients that are skeletally immature with a kyphosis between 45° and 65° are candidates for bracing. Surgery is generally considered if kyphosis is more than 65° and is associated with pain not alleviated by other methods. Unlike the classic type, the treatment of lumbar Scheuermann is more straightforward as its course is non-progressive. Symptoms generally resolve with rest, activity modification, and time (Afshani and Kuhn 1991; Lowe and Line 2007; Ristolainen et al. 2012).
10.4.6 Spondylolysis and Spondylolisthesis
Spondylolysis is defined as a unilateral or bilateral bony defect in the pars interarticularis (also known as the isthmus) of the vertebral posterior elements. In the general population, the incidence of spondylolysis is around 6–8 % (McTimoney and Micheli 2003). In the athletic population, however, the incidence of spondylolysis is much higher, up to 63 % (Rossi 1978). Spondylolysis is the primary cause of back pain in athletes and responsible for approximately 47 % of low back pain in this population (Micheli and Wood 1995). Spondylolysis is rarely seen in children younger than 5 years, which makes a congenital pathogenesis not very likely. The incidence increases with age until about 20, after which the incidence stabilizes (Brooks et al. 2010). Spondylolysis is more frequent in boys than in girls and more frequent in whites than in blacks (Leone et al. 2011). More recent studies suggest an equal prevalence between boys and girls (Haus and Micheli 2012). This might be due to a general increase in the number of female athletes, especially in sports such as ballet and gymnastics. Spondylolisthesis appears to be more frequent in girls (Loud and Micheli 2001).
The pathogenesis remains controversial. Most likely spondylolysis is a multifactorial condition in which a stress fracture occurs in a congenitally weak or dysplastic pars interarticularis (Leone et al. 2011). The mechanism of injury is often a combination of repetitive forces like flexion, extension, and rotation of the lumbar spine. Sports associated with an increased frequency of spondylolysis are typically sports requiring hyperextension motions such as gymnastics and diving. Contact sports such as football, soccer, hockey, and lacrosse also have an increased risk of spondylolysis (Afshani and Kuhn 1991). The injury may be unilateral or bilateral and occurs most commonly (in 95 % of cases) at the L5 vertebra. When the injury is bilateral, spondylolisthesis may occur. Spondylolisthesis generally refers to the forward translation of one vertebra relatively to the next more caudal vertebra. It mostly involves the L5–S1 segment. It has different etiologies (cfr. Wiltse classification) with isthmic spondylolisthesis being the most common subtype (Haus and Micheli 2012).
Spondylolysis may be completely asymptomatic. If there are symptoms, the athlete typically complains of a mechanical-type low back pain, typically getting worse with hyperextension and improving with rest. The pain may radiate to the buttocks or posterior thigh. The onset is often insidious, but can be precipitated by an acute injury. Common findings on physical examinations are a hyperlordotic posture and bilateral hamstring tightness. Hyperextension with a one-leg stance exacerbates the pain. Radicular signs are less common, but may occur in the presence of spondylolisthesis (Haus and Micheli 2012; Leone et al. 2011). The role of imaging is discussed in Chaps. 11 and 12.
The treatment of spondylolysis is initially conservative with cessation of sporting activities and spinal bracing for 3–6 months. The aim is to reduce pain and to facilitate healing. Surgical treatment is typically reserved for patients who do not respond to conservative treatment after 6 months. Surgery is necessary in 9–15 % of patients with spondylolysis and/or low-grade spondylolisthesis. Surgery should not be considered lightly as it often concerns young patients (Leone et al. 2011).
10.4.7 Lumbar Stenosis
Degenerative lumbar spinal stenosis is caused by mechanical factors and/or biochemical alterations within the intervertebral disk that lead to disk space collapse, facet joint hypertrophy, soft tissue infolding, and osteophyte formation, which narrows the space available for the thecal sac and exiting nerve roots (Lee et al. 2013; Issack et al. 2012). The clinical consequence of this compression is neurogenic claudication and varying degrees of leg and back pain. Symptoms include radicular pain, numbness, tingling, and weakness. It is a common diagnosis that is occurring with increased frequency in sports medicine clinics (Borg-Stein et al. 2012). Degenerative lumbar spinal stenosis is a major cause of pain and impaired quality of life in the elderly. The natural history of this condition varies; peripheral vascular disease presents similarly and must be considered in the differential diagnosis.
10.4.8 Sacroiliac Joint Injury/Inflammation
The sacroiliac (SI) joint may also give rise to low back pain. Symptoms usually develop insidiously and are worsened by sports activities (Brolinson et al. 2003). There is palpation tenderness over the SI-joint. Spine extension is often painful and the FABER test reproduces pain in the affected SI-joint. Straight leg raise testing is negative. Symptoms may be quite similar to those found in patients with spondylolysis. Inflammation of the SI-joint can be associated with several other conditions like Crohn’s disease, psoriasis, and ankylosing spondylitis (seronegative spondyloarthropathies) and Reiter’s syndrome. Serological screening and imaging (Chaps. 11 and 12) should be performed in case of doubt with regard to the diagnosis.
10.4.9 Fractures and Dislocations
Flexion injuries of the cervical spine can cause compression fractures of the vertebral bodies (McRae and Esser 2008). Flexion fractures occur most frequent at the level C5 and C6 in adolescents. When combined with significant axial loading, flexion injuries can result in burst fractures of the vertebral bodies with retropulsion of bony fragments into the spinal canal (Maxfield 2010). The spine is particularly vulnerable for rotational forces; combined rotational forces can result in more severe subluxation due to increased disruption of supporting tissue. Because of the small, flat, almost horizontal configuration of the articular processes of the cervical spine, dislocation can occur relatively easy in case of trauma (Boran et al. 2011).
Acute fractures of the thoracolumbar spine are less frequent than cervical injuries and tend to be less catastrophic. In the thoracolumbar region, compression fractures are the most common type in young athletes. Compression fractures, as the name suggests, occur due to a compression force on the spine. This may happen during a traumatic injury such as a fall from a height, landing on the feet or buttocks (McRae and Esser 2008). More frequently, vertebral compression fractures occur in older people with osteoporosis or other preexisting spinal conditions where the bone is weak. There may not be one particular incident that causes it and pain may develop gradually.
Avulsion fractures of the spinous and transverse processes are also seen in athletes. Avulsion of the spinous process of the C7 and Th1 vertebrae are known as clay-shoveler fractures.
10.5 Spinal Injuries Associated with Specific Sports
Some sports are associated with a higher than normal percentage of spine injuries.
Acute spinal trauma can be seen in many sports and is related to an increased risk for trauma. These traumatic injuries do not differ significantly from those seen in non-sports-related trauma, e.g., falls or motor vehicle accidents.
More specific spine injuries are seen in chronic overload and/or strain to the spine occurring in some sports. These will be discussed in detail in this chapter.
The most common sports responsible for spinal injuries are equestrian events (41.8 %), rugby (16.3 %), diving (15.3 %), Gaelic football and hurling (9.6 %), cycling (4.2 %), and miscellaneous (12.7 %) (Boran et al. 2011). In general more males (74 %) than females (26 %) are injured, and the average age is 30.2 years (range 14–72 years).
Injuries are mostly to the cervical spine (60 %) and less to the thoracic (21 %) or lumbar spine (19 %). In 40 % of patients, more than one vertebral level is affected (Boran et al. 2011).
10.5.1 Sports Involving High-Velocity Incidents or Falls
10.5.1.1 Skiing and Snowboarding
Spinal injuries associated with recreational skiing and snowboarding mostly result from high-energy falls and to a lesser degree from collisions with other skiers, trees, or equipment. In competition snowboarding, spinal injuries are specifically related to the risks associated with jumping and performing moves.
Orthopedic injuries sustained in alpine skiing/snowboarding are numerous, with spinal injuries comprising between 1 and 20 % of all injuries (Floyd 2001; Levy and Smith 2000; Prall et al. 1995; Yamakawa et al. 2001). Snowboarding accidents result in more fractures, especially in the upper limbs, fewer knee injuries, and more severe injuries caused by impacts rather than by torsions (Yamakawa et al. 2001). Spinal injuries are more than two times more frequent in snowboarders compared to skiers.
The incidence of spinal injury in skiing and snowboarding is in general very low (0.001/1,000 skier-days). Although less frequent, spine and spinal cord injuries are the most debilitating and costly of serious injuries sustained by skiers (Prall et al. 1995). The majority (80 %) of spinal lesions are thoracic or lumbar, and multilevel lesions are seen in 20 % of patients. Compression fractures with loss of height of the anterior part of the vertebral body are the most frequent thoracic and lumbar lesions seen in 38–90 % of patients (Floyd 2001; Prall et al. 1995). Severe and/or unstable thoracic or lumbar fractures are seen in less than 5 % of patients. Snowboarders in general have the same pattern of lesions except for transverse process fractures that are significantly more frequent.
Cervical lesions on the other hand, although more rare, are usually more severe. In one major study, spinal cord injuries were seen in 17 % of ski accidents with spinal fractures, usually in association with cervical lesions (Prall et al. 1995).
There is a significantly higher incidence of spinal injury among beginner snowboarders than among beginner skiers. Furthermore, intermediate or expert snowboarders were more likely to be injured because of jumping than beginners, whereas about 70 % of spinal injuries caused by skiing results from a simple fall (Yamakawa et al. 2001).
As a final note in skiers and snowboarders under 13 years of age, helmet use does not increase the incidence of cervical spine injury but does reduce the incidence of head injury (Macnab et al. 2002).
10.5.1.2 Cycling
Although the vast majority of injuries suffered while cycling are minor, acute spinal injuries have been reported. Profound neurological deficits are reported in patients that are thrown over the handlebars while traveling downhill at speed (McGoldrick et al. 2012). Spinal injuries are more frequently seen in mountain bikers, due not only to the characteristics of the terrain but also to the readiness to assume a higher risk compared to cycle racing (Schueller 2010).
Neck and back pain is extremely common in cyclists, occurring in up to 60 % of riders. To avoid or lessen spinal pain, proper fit of the bicycle is critical. Proper frame selection and adjustment can be made by following existing guidelines for frame size, seat height, fore and aft saddle position, saddle angle, and reach and handlebar height (Mellion 1991). Especially an appropriate pedal unit position may reduce low back pain. Positioning the pedals behind the saddle axis permits more physiological spine angles in comparison with the classic one having the pedals in front of the saddle axis (Fanucci et al. 2002). Lower back pain is the most prevalent overuse injury seen in cyclists, with an incidence up to 45 %, and low back pain causes the highest rates of functional impairment and medical attention in cycling (Clarsen et al. 2010). This high incidence might be caused by the creep induced in the viscoelastic tissues of the spine as a result of cyclic loading that subsequently desensitizes the mechanoreceptors within, allowing full exposure to instability and injury (Solomonow et al. 1999).
10.5.1.3 Horseback Riding
Horseback riding is the most common sport responsible for a spinal injury. Spinal injuries are an inevitable risk of horse riding with the rider high from the ground, relatively unprotected, and the horse that travels at speeds of up to 65 km/h. Moreover, the spines of the riders are relatively unprotected since effective gear to protect the spine still does not exist. Compared to other sports, horse riding accounts for the largest number of hospital admittance days by far and between 7 and 10 % of all riders requiring hospital admission suffer from spinal injuries (Hessler et al. 2014). In the United States, the rate of serious injuries from horseback riding has been reported to range from 1 per 350 to 1,000 h of riding. In British Columbia, Canada, the rate of hospital admissions for horseback riding injuries is 0.49 per 1,000 h of riding. In the Netherlands, every year, one out of seven riders will sustain an injury (Siebenga et al. 2006). Several studies have suggested that horseback riding is riskier than motorcycle riding, skiing, football, and hockey (Lin et al. 2011; Siebenga et al. 2006). In some countries, 70 % of all spine fractures caused by sports activities are sustained by equestrian activities (Hipp et al. 1977). Although numerically few, spine and spinal cord lesions from horse riding accidents are frequently catastrophic giving rise to paralysis or dead (Silver 2002). The injury of actor Christopher Reeve (“Superman”) in 1995, resulting in a complete C2-level SCI, heightened public awareness of the risks associated with horseback riding.
Up to 80–90 % of horseback riding accident victims are female (Hessler et al. 2014; Siebenga et al. 2006). Most spinal injuries are caused by falling of the horse (65–80 %), followed by being kicked by a horse. Around 80 % of the injuries occur at the thoracolumbar junction, either at Th12, L1, or L2 (Siebenga et al. 2006). Lumbar injuries being the most frequent (70 %), thoracic injuries second most frequent (30 %), while cervical injuries are more rare (Hessler et al. 2014). Other studies found relatively more thoracic injuries (Roe et al. 2003). The majority of fractures (85 %) are vertebral compression lesions (Hessler et al. 2014). Spinal cord injury from horseback riding affects an equal proportion of women and men, has a wide age range, and most commonly results in incomplete tetraplegia followed by complete paraplegia (Lin et al. 2011). Overall figures from the USA show that between 1973 and 1985, a total of 9,647 new admissions with spinal cord injury, 14.2 % were due to sport, of which 2 % represented horseback riding injuries (Stover and Fine 1987). A fall from a horse would appear to be most likely to cause a spinal cord injury. A kick, while it may cause a fracture of a transverse process, usually does not cause spinal cord injury (Silver 2002).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree