Posttreatment imaging evaluation of sinuses encompasses a wide gamut of procedures, ranging from endoscopic procedures for sinonasal inflammatory diseases to markedly radical surgeries for malignant neoplasms (with or without reconstructions), as well as providing access for surgeries involving the anterior and central skull base. Advances in both techniques and devices have expanded the use of endoscopic approaches in managing both benign and malignant lesions, in addition to being the primary surgical method for treating all medically refractive sinonasal inflammatory disorders. Familiarity with the complex anatomy in the sinonasal region and knowledge of the various procedures is indispensable in interpreting these imaging studies.
Key points
- •
Functional endoscopic sinonasal surgery (FESS) is the preferred method for treating medically refractive sinusitis.
- •
Advances in FESS techniques have expanded the role of FESS surgery in managing benign and malignant masses, as well as becoming the preferred approach in providing access for skull base and pituitary surgeries.
- •
Familiarity with the various procedures, knowledge of the various causes of surgical failures and complications, and understanding of the complex anatomy in this region, is essential for accurate interpretation.
Introduction
Modern sinonasal surgery is heavily dependent on endoscopic techniques both for treating mucosal inflammatory conditions and for accessing various benign and malignant sinonasal, skull base, and periorbital lesions. Over the last 2 decades, endoscopic approaches for various sinonasal surgeries have become ubiquitous and have significantly reduced patient morbidity with faster recovery times.
Most sinonasal surgeries come under the umbrella term functional endoscopic sinus surgery (FESS) ( Box 1 ), which is a minimally invasive surgical technique, most often performed for the treatment of chronic sinusitis or sinonasal polyposis. The overall aim is to create or restore patency of the normal anatomic drainage pathways to allow for the clearance of secretions and normal sinus ventilation. Multiple different surgical techniques can be used during a single surgery based on the individual anatomy and specific locations of disease. Advances in technology and increasing familiarity with endoscopic techniques have led to the increasing use of endoscopic approaches for both benign and malignant sinonasal tumors. Open surgeries are still used for more extensive disease or in instances whereby achieving adequate tumor resection is not amenable to endoscopic technique.
External nose and septum
- •
Rhinectomy (partial or total, with prosthesis or reconstruction)
- •
Septoplasty (either primary or for access/approach)
- •
Directed toward anterior osteomeatal unit
- •
Maxillary or middle meatus antrostomy and uncinectomy
- •
Middle and inferior turbinectomy
- •
Ethmoidectomy (total or partial)
- •
Directed toward posterior osteomeatal unit
- •
Sphenoidotomy
- •
Posterior ethmoidectomy
- •
Frontal sinus procedures
- •
Endoscopic frontal sinusotomy (Draf type I, II, and III [modified Lothrop])
- •
Caldwell–Luc surgery
Approach for orbital procedures
Approach for skull base and pituitary surgeries
Approach for the resection of benign and malignant mass lesions
Surgery for malignant masses
- •
Maxillectomy (partial/lateral/total), palatectomy (partial), turbinectomy
- •
Craniofacial resection
- •
Osteoplastic flap frontal sinus obliteration and frontal sinus cranialization
Imaging is a critical tool for preoperative planning, diagnostic workup of causes of treatment failure, and for the evaluation of postsurgical complications ( Box 2 ). Imaging for sinonasal malignant and benign tumors is performed for preoperative staging, surgical planning, and postoperative tumor surveillance. Expected imaging findings following endoscopic surgery for both benign and malignant indications are largely site-specific.
Minor complications
- •
Recurrent sinusitis and polyposis
- •
Residual frontal sinus disease
- •
Lateralized middle turbinates/scarring stenosis or middle meatus
- •
Adhesions and septations
- •
Mucus recirculation
- •
Neo-osteogenesis
- •
Nasal septal perforations
- •
Empty nose syndrome
- •
Major complications
Vascular injury
- •
Hemorrhage
- •
Pseudoaneurysm
- •
Orbital complications
- •
Hematoma
- •
Abscess
- •
Penetration
- •
Motility disorder
- •
Blindness
- •
Intracranial injury
- •
CSF leak, meningocele, and encephalocele
- •
Subarachnoid and parenchyma injury with edema and/or hemorrhage
- •
Infection – abscess/cerebritis
- •
Imaging technique
Imaging following sinonasal surgery for chronic sinusitis has historically relied on direct imaging in the coronal plane. Multidetector CT now allows for imaging in the axial plane with isotropic voxels and multiplanar reconstruction in the coronal, sagittal, or oblique planes. Thin section axial imaging and multiplanar reconstruction also allow for a reduction in dental amalgam artifacts and the use of imaging data with intraoperative stereotactic guidance systems. Administration of intravenous contrast is usually not necessary for imaging after FESS unless there is a concern for infection. Magnetic resonance imaging (MRI) is usually reserved for cases of suspected intracranial complications or in situations whereby there is diagnostic uncertainty not amenable to direct visual or endoscopic evaluation. Angiography may be used in select cases when there is concern for vascular complication. Computed tomography angiography (CTA), magnetic resonance angiography (MRA), or catheter-based angiography may be used.
Although MRI or CT with intravenous contrast is most commonly used following surgery for the resection of sinonasal tumors, PET/CT is a very useful tool for the evaluation of residual/recurrent disease and nodal involvement. The timing of imaging following surgery for sinonasal malignancy is an important factor to consider. A baseline postoperative MRI or CT is typically performed between 1 and 4 months following surgery to allow the expected postoperative inflammatory changes in subside. Most clinicians then follow the National Comprehensive Cancer Center (NCCN) guidelines for the timing of additional surveillance imaging.
Surgical techniques and imaging findings
Septoplasty
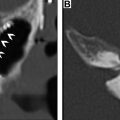
Most often, the initial step in endoscopic sinus surgery is septoplasty to provide better surgical access for subsequent surgical techniques. Septoplasty may also be performed to relieve any associated nasal cavity obstruction secondary to a deviated nasal septum and/or any associated bony septal spur. Severe nasal septal deviation or a large spur can also contribute to sinusitis secondary to mass effect on associated osteomeatal unit structures. Imaging findings following septoplasty include a straightened nasal septum, thinned septal mucosa, irregular septal mucosal contour, and absence of any bony spurs. , In the early postoperative period following septoplasty, nasal stents or packing material may be identified , Imaging findings of septoplasty are best depicted in the coronal or axial planes( Fig. 1 ).

To help facilitate endonasal approaches to the anterior skull base or sellar region, the posterior nasal septum may be resected. Often, this is conducted in concert with the removal of other structures such as ethmoid septations, one or both middle turbinates, or the superior turbinates. If not resected, the turbinates may be lateralized. These actions are performed to help improve accessibility to the site of interest, improve the manipulation of surgical instruments in the posterior nasal cavity, and to improve visibility. Postsurgical changes from septectomy are best seen in the axial plane.
Rhinectomy
Most malignancies involving the external nose only require limited local surgical excision or radiotherapy. For advanced cases, partial or total rhinectomy may be performed. Reconstruction may be performed with autologous regional or free tissue flaps, although this is a technically difficult procedure and outcomes are often unsatisfactory. Nasal prostheses are currently the reconstruction technique of choice following rhinectomy. , ( Fig. 2 ).

Maxillary sinus surgery
Maxillary Antrostomy and Uncinectomy
Following septoplasty, removal of the uncinate process (uncinectomy) may be performed. Uncinectomy allows for greater surgical access to the maxillary ostium, frontal recess, and anterior ethmoid complex, for treating obstruction involving the anterior osteomeatal complex. Next, widening of the maxillary sinus ostium and infundibulum (maxillary antrostomy or middle meatus antrostomy) may be performed ( Fig. 3 ). If present, maxillary polyps, mucosal hypertrophy, or tumors amenable to endoscopic treatment may then be resected ( Fig. 4 ). Imaging findings of uncinectomy and maxillary antrostomy include the absence or partial absence of the uncinate process and widening of the maxillary ostium and infundibulum. These findings are typically best depicted in the coronal plane.


Caldwell–Luc Procedure
Several procedures which are no longer commonly performed or performed less frequently than previously for certain indications may sometimes be seen on imaging, particularly in older patients. The Caldwell–Luc procedure involves the external access of the maxillary sinus through a surgically created defect in the buccal mucosal surface of the maxillary bone and passage through the anterior wall of the maxillary sinus. This is usually followed by a middle meatal antrostomy or an inferior nasoantral window or inferior meatal antrostomy, a surgically created defect in the medial wall of the maxillary sinus below the inferior turbinate attachment. The canine fossa puncture has a similar approach to the Caldwell–Luc procedure and is sometimes performed for specific indications related to maxillary sinus disease. Postprocedural changes from Caldwell–Luc procedure are best seen in the axial plane as a defect in the anterior wall of the maxillary sinus ( Fig. 5 ). Postsurgical changes from inferior nasalantral window creation or inferior meatus puncture are best seen in the coronal plane as a defect in the medial maxillary wall inferior to the inferior turbinate attachment.

Maxillectomy
Maxillectomy can be partial or total. For tumors centered along the medial maxillary wall or the lateral nasal wall, a medial maxillectomy may be performed. In a medial maxillectomy, the medial maxillary sinus wall/lateral nasal wall is removed, traditionally along with the inferior turbinate and the nasolacrimal duct although the preservation of the inferior turbinate or nasolacrimal duct may be attempted. Depending on tumor extent and/or ability to access the necessary areas, other structures may be resected or manipulated including the middle turbinate or portions of the ethmoid cavity. Depending on tumor extent, partial maxillectomy can involve the lateral wall, or can be extended to include portions of the palate, orbital floor, or other structures ( Fig. 6 ). If the palate or orbital floor is resected, one may see palatal prostheses, palatal reconstruction flaps, orbital floor mesh reconstruction hardware, or orbital floor reconstruction flaps on postoperative imaging. Partial maxillectomy may be performed endoscopically or via an open approach.

Total maxillectomy involves the resection of all of the maxillary sinus walls. Removal of the orbital contents or orbital exenteration may also sometimes be necessary. Because this involves the resection of several tissues and significant alterations in anatomy, flaps, or prosthesis are used to reconstruct the midface for both functional and cosmetic reasons. Free flaps are most commonly used but local pedicled flaps may also be seen.
Nasal turbinate surgery
Middle Turbinectomy
Middle turbinectomy is commonly performed during FESS and may be performed to allow for greater access during approaches to sinonasal or sellar tumors. The middle turbinate vertical insertion at the skull base is an important surgical landmark during endoscopic sinus surgery. Surgeons generally attempt to stay lateral to the middle turbinate in an effort to avoid inadvertently causing a cerebrospinal fluid (CSF) leak. For this reason, middle turbinectomy is most often partial with a portion of the vertical insertion at the skull base usually intentionally left intact (see Fig. 3 ). The presence or absence of a residual middle turbinate following endoscopic sinus surgery with middle turbinectomy should be noted. To prevent recurrent osteomeatal complex obstruction, following partial middle turbinectomy, the residual middle turbinate may be purposefully fixated to the lateral wall of the nasal septum. (see Fig. 3 ). This is beneficial anatomically and should be noted in the radiology report. Likewise, a lateralized middle turbinate on postsurgical imaging is an important finding to identify and communicate as this could be a potential cause for recurrent osteomeatal complex obstruction and sinusitis. Findings of middle turbinectomy are generally easiest to appreciate in the coronal plane.
Inferior Turbinectomy
Inferior turbinate reduction or inferior turbinoplasty may be performed for cases of nasal cavity obstruction secondary to the mucosal inflammation of these structures. Resection can be total or partial. Resection can involve submucosa or bone. Lateralization of the inferior turbinates via out-fracture may be performed. Additionally, various types of ablation (radiofrequency, ultrasound, cryoablation) can be used to produce scarring and subsequent reduction in mucosal volume. On imaging, finding of inferior turbinate reduction or turbinoplasty includes the partial or complete absence of the inferior turbinate, lateralization of the inferior turbinate, or thinning of the inferior turbinate mucosal structures. These findings are best depicted in the coronal plane.
Ethmoid sinus surgery
Ethmoidectomy
Depending on the extent of disease and patient anatomy, total or partial ethmoidectomy may be performed ( Fig. 7 ). If the posterior ethmoid air cells are entered, a portion of the vertical basal lamella of the middle turbinate must be removed. This structure demarcates the anterior from the posterior ethmoid air cells. The presence of residual ethmoid air cells should be noted, especially if disease is present. Residual cells are usually located superiorly near the skull base or posteriorly near the sphenoid sinuses and may be intentionally left intact to avoid CSF leak or optic nerve injury. A deep olfactory fossa, an asymmetrically low olfactory fossa on one side, or dehiscence of the cribriform plate or ethmoid roof may predispose to iatrogenic injury. Findings of ethmoidectomy are best seen in the axial and coronal planes.