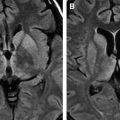
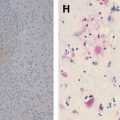
Acute disseminated encephalomyelitis (ADEM) is a monophasic demyelinating disease of the central nervous system typically affecting the gray and the white matter of the brain and spinal cord in multiple locations. In the acute stages, ADEM is characterized histologically by perivenous edema, demyelination, and infiltration with macrophages and lymphocytes, with relative axonal sparing, whereas the late course of the disease is characterized by perivascular gliosis.
Acute disseminated encephalomyelitis (ADEM) is a monophasic demyelinating disease of the central nervous system typically affecting the gray and the white matter of the brain and spinal cord in multiple locations. In the acute stages, ADEM is characterized histologically by perivenous edema, demyelination, and infiltration with macrophages and lymphocytes, with relative axonal sparing, whereas the late course of the disease is characterized by perivascular gliosis .
ADEM has a typical temporal relationship with a prior infectious episode or vaccination, which functions as a trigger to the inflammatory response. It occurs in the majority (50%–75%) of cases in the aftermath of a viral or bacterial infection, mostly involving an upper respiratory tract infection that occurs 1 to 3 weeks before the onset of the illness. Vaccination, especially against measles, mumps, or rubella (ie, postimmunization encephalomyelitis) is another predisposing factor. The clinical history may be blurred, however, with no recognizable preceding event or causal factor. When the implicated episode is not recent, a causal correlation becomes less evident, or even impossible to advocate; on the contrary, because of the high frequency of viral episodes in children, medical history often is positive regardless of whether or not an established causal correlation exists. This is the reason why, unless the latency period is shorter than 30 days, a causal link between a febrile episode and ADEM may not be established conclusively . In exceptional cases, ADEM may complicate the course of autoimmune diseases (ie, systemic lupus erythematosus) and neoplasm (ie, small cell lung carcinoma) .
Pathogenesis
The pathogenesis of ADEM is debated despite the large number of theories proposed, even though there is general consensus that ADEM is an immune-mediated disorder resulting from an autoimmune reaction to myelin. The most compelling evidence perhaps is represented by the similarities of ADEM to experimental allergic encephalomyelitis, in which damaged myelin exposes segregated antigens that in turn induce an immune response. Two basic mechanisms currently are under consideration :
- 1.
Inflammatory cascade theory: viral infection results in nervous tissue damage, which causes segregated antigens to leak into the systemic circulation through a damaged blood-brain barrier; these antigens are processed in the lymphatic organs and elicit a T-cell response, which in turn damages the central nervous system (CNS) and perpetuates inflammation.
- 2.
Molecular mimicry theory: there is a structural similarity between the pathogen and the myelin proteins of the host; B- and T-cells that are activated during the immune response to infection enter the CNS and react against the presumed foreign antigen represented by the homolog myelin protein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree