This article reviews normal embryologic development of the spine and spinal cord and the imaging features of congenital abnormalities of the spine and spinal cord, with particular focus on magnetic resonance imaging. The authors discuss spinal dysraphisms, a heterogeneous group of congenital abnormalities of the spine and spinal cord, and provide information to expand understanding of these complex entities.
Spinal cord development
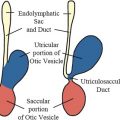
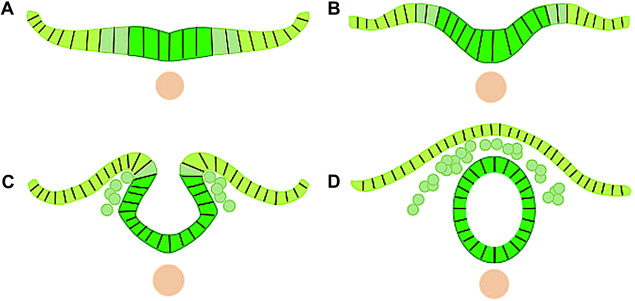
There are 3 basic embryologic stages to spinal development. The first stage occurs during the second or third week of embryonic development and is referred to as gastrulation. During gastrulation, the embryonic disk converts from a bilaminar disk to a trilaminar disk composed of ectoderm, mesoderm, and endoderm. Primary neurulation is the second stage in spinal development and occurs during weeks 3 to 4. During primary neurulation, the notochord and overlying ectoderm interact to form the neural plate, which then bends and folds to form the neural tube. The neural tube then closes bidirectionally in a zipperlike manner ( Fig. 1 ). Secondary neurulation is the final stage of spinal development and occurs during weeks 5 and 6. During secondary neurulation, the secondary neural tube is formed by the caudal cell mass. The secondary neural tube is initially solid, subsequently cavitates, and eventually forms the tip of conus medullaris and filum terminale via a process called retrogressive differentiation. Abnormalities in any of these developmental stages can lead to spine or spinal cord malformations.
Categorization of spinal dysraphisms
Spinal dysraphisms can be broadly divided into open and closed types. Open spinal dysraphisms describe entities that have an overlying skin defect with neural tissue exposed to the environment. Closed spinal dysraphisms describe entities in which the overlying skin remains intact. Closed spinal dysraphisms can be further subcategorized based on whether a subcutaneous mass is present or absent. The key features of open and closed spinal dysraphisms are summarized in Table 1 .
| Open Spinal Dysraphisms -Not covered by intact skin | |
| Myelocele | Neural placode flush with skin surface |
| Myelomeningocele | Neural placode protrudes above skin surface |
| Hemimyelocelee | Myelocele associated with diastematomyelia |
| Hemimyelomeningocele | Myelomeningocele associated with diastematomyelia |
| Closed Spinal Dysraphisms -Covered by intact skin With a Subcutaneous Mass: | |
| Lipomyelocele | Placode-lipoma interface within the spinal canal |
| Lipomyelomeningocele | Placode-lipoma interface outside of the spinal canal |
| Meningocele | Herniation of CSF filled sac lined by dura |
| Terminal myelocystocele | Terminal syrinx herniating into posterior meningocele |
| Myelocystocele | Dilated central canal herniating through posterior spina bifida |
| Without a Subcutaneous Mass: Simple Dysraphic States | |
| Intradural lipoma | Lipoma within the dural sac |
| Filar lipoma | Fibrolipomatous thickening of filum |
| Tight filum terminale | Hypertrophy and shortening of filum |
| Persistent terminal ventricle | Persistent cavity within conus medullaris |
| Dermal sinus | Epithelial lined fistula between neural tissue and skin surface |
| Complex Dysraphic States | |
| Dorsal enteric fistula | Connection between bowel and skin surface |
| Neurenteric cyst | More localized form of dorsal enteric fistula |
| Diastematomyelia | Separation of cord into two hemicords |
| Caudal agenesis | Total or partial agenesis of spinal column |
| Segmental spinal dysgenesis | Various segmentation anomalies |
Categorization of spinal dysraphisms
Spinal dysraphisms can be broadly divided into open and closed types. Open spinal dysraphisms describe entities that have an overlying skin defect with neural tissue exposed to the environment. Closed spinal dysraphisms describe entities in which the overlying skin remains intact. Closed spinal dysraphisms can be further subcategorized based on whether a subcutaneous mass is present or absent. The key features of open and closed spinal dysraphisms are summarized in Table 1 .
| Open Spinal Dysraphisms -Not covered by intact skin | |
| Myelocele | Neural placode flush with skin surface |
| Myelomeningocele | Neural placode protrudes above skin surface |
| Hemimyelocelee | Myelocele associated with diastematomyelia |
| Hemimyelomeningocele | Myelomeningocele associated with diastematomyelia |
| Closed Spinal Dysraphisms -Covered by intact skin With a Subcutaneous Mass: | |
| Lipomyelocele | Placode-lipoma interface within the spinal canal |
| Lipomyelomeningocele | Placode-lipoma interface outside of the spinal canal |
| Meningocele | Herniation of CSF filled sac lined by dura |
| Terminal myelocystocele | Terminal syrinx herniating into posterior meningocele |
| Myelocystocele | Dilated central canal herniating through posterior spina bifida |
| Without a Subcutaneous Mass: Simple Dysraphic States | |
| Intradural lipoma | Lipoma within the dural sac |
| Filar lipoma | Fibrolipomatous thickening of filum |
| Tight filum terminale | Hypertrophy and shortening of filum |
| Persistent terminal ventricle | Persistent cavity within conus medullaris |
| Dermal sinus | Epithelial lined fistula between neural tissue and skin surface |
| Complex Dysraphic States | |
| Dorsal enteric fistula | Connection between bowel and skin surface |
| Neurenteric cyst | More localized form of dorsal enteric fistula |
| Diastematomyelia | Separation of cord into two hemicords |
| Caudal agenesis | Total or partial agenesis of spinal column |
| Segmental spinal dysgenesis | Various segmentation anomalies |
Open spinal dysraphisms
Myelomeningocele and Myelocele
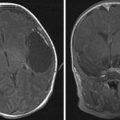
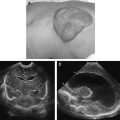
Myelomeningocele and myelocele result from defective closure of the primary neural tube and are characterized clinically by neural placode exposure through a midline skin defect on the back. Myelomeningoceles account for greater than 98% of open spinal dysraphisms. Myeloceles are rare. Because open spinal dysraphisms are often diagnosed clinically (often antenatally), imaging of these entities is not always performed. When imaging is performed, the main differentiating feature between a myelomeningocele and myelocele is neural placode position relative to the skin surface. With a myelomeningocele, the neural placode protrudes above the skin surface ( Fig. 2 ). With a myelocele, the neural placode is flush with the skin surface ( Fig. 3 ).
Hemimyelomeningocele and Hemimyelocele
Hemimyelomeningocele and hemimyelocele have been described but are rare. These entities occur when a myelomeningocele or myelocele is associated with diastematomyelia (cord splitting) and one hemicord fails to neurulate.
Closed spinal dysraphisms with a subcutaneous mass
Lipomas with a Dural Defect
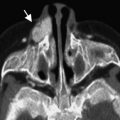
Lipomas with a dural defect can be characterized as lipomyelocele or lipomyelomeningocele and occur as a result of defective primary neurulation whereby mesenchymal tissue enters the neural tube and forms lipomatous tissue. Clinically, lipomyeloceles and lipomyelomeningoceles are characterized by the presence of a subcutaneous fatty mass above the intergluteal crease. The position of the placode-lipoma interface is the main differentiating feature between a lipomyelocele and lipomyelomeningocele. If the placode-lipoma interface lies within the spinal canal, it is characterized as a lipomyelocele ( Fig. 4 ). If the placode-lipoma interface lies outside of the spinal canal because of expansion of the subarachnoid space, it is characterized as a lipomyelomeningocele, ( Fig. 5 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree