This article reviews the embryology, anatomy, congenital anomaly, acquired disorders, degenerative diseases, neoplasms, and inflammatory and infectious disorders in the craniovertebral junction. The imaging characteristics and differential diagnoses of these lesions are provided. This review also focuses on the complimentary roles of different imaging modalities.
The craniovertebral junction (CVJ) consists of the occipital bone, foramen magnum, clivus, atlas (C1), axis (C2), and ligaments of the atlanto-occipital and atlantoaxial articulations. The CVJ provides the support needed for movement of the head. The atlantoaxial joints enable head rotation about the dens axis, whereas the atlanto-occipital joints primarily allow flexion, extension, and lateral bending.
Anatomy and embryology
The occipital bone is composed of the basiocciput, supraocciput, exocciput, and occipital squamosa. They are separated by cartilaginous plates called synchondroses. The basiocciput forms the superior half of the clivus; the squamosa forms the interparietal and supraoccipital calvaria; and the exocciput forms the lateral margins of the foramen magnum, occipital condyles, and hypoglossal canals. The embryology and development of the CVJ are summarized in Table 1 .
| Sclerotomes | Divisions | Subdivisions | Formations |
|---|---|---|---|
| First occipital | — | — | Basiocciput |
| Second occipital | — | — | Exoccipital centers |
| Third occipital | — | — | (Jugular tubercles) |
| Fourth proatlas | Hypocentrum | — | Anterior tubercle clivus |
| — | Centrum | — |
|
| — | Neural arch | Ventral rostral |
|
| — | — | Dorsal caudal |
|
| — | Hypocentrum | — | Anterior arch of C1 |
| First spinal | Centrum | — | Dens of C2 |
| — | Neural arch | — | Posterior inferior arch of C1 |
| Second spinal | Hypocentrum | Disappears | — |
| — | Centrum | — | Body of C2 |
| — | Neural arch | — | Facets, posterior arch of axis |
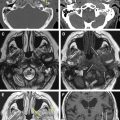
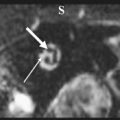
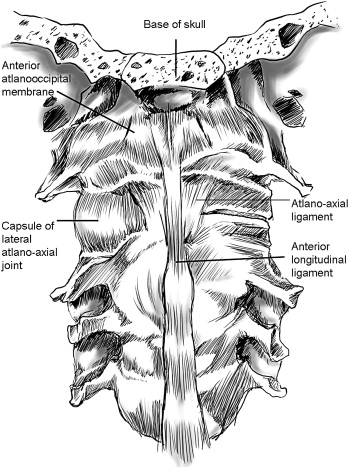
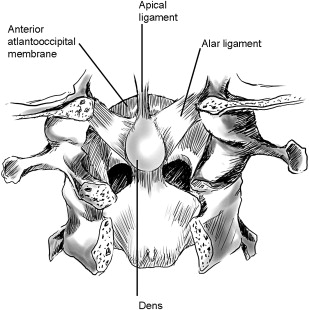
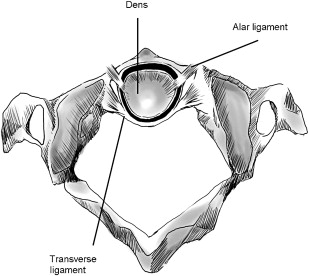
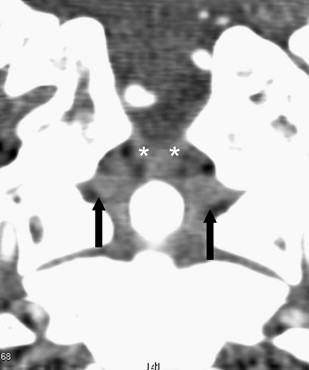
Laterally, the C1 articulates with the occipital condyles superiorly, the atlanto-occipital joint, the lateral masses of C2, and the atlantoaxial joints ( Fig. 1 ). These lateral atlantoaxial joints are enclosed by a joint capsule and the accessory atlantoaxial ligament. The dens (odontoid process) of C2 articulates with the anterior arch of C1 and is held in place by the transverse part (transverse ligament) of the cruciform ligament ( Fig. 2 ), which attaches laterally to tubercles on the inner surface of C1. It is also held in place by the alar and apical ligaments (see Fig. 2; Fig. 3 ) attached to the occipital bone. The superior tip of the odontoid process (ossiculum terminale) develops from the fourth occipital sclerotome. Apical, alar, and transverse ligaments (see Figs. 2 and 3 ; Figs. 4–6 ) are lacking or nonfunctional if there is no ossiculum terminale. A transverse line of low signal with a brighter signal above and below on sagittal or coronal T1-weighted MR imaging is usually evident at the junction of the odontoid process and body of C2 ( Fig. 6 A) in individuals younger than 50 years of age.
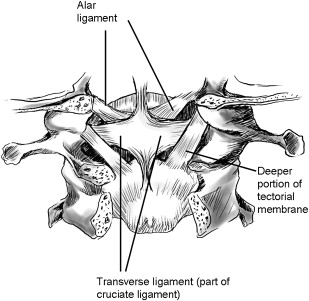
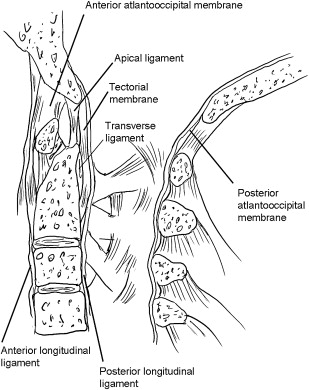
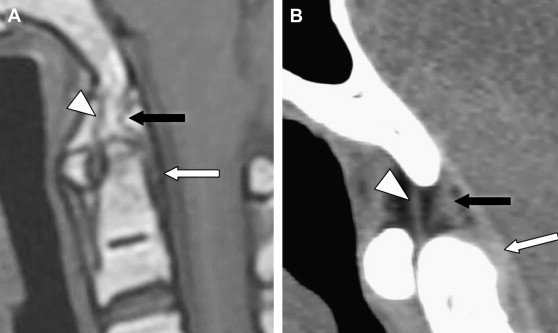
The transverse ligament appears as an oval area of signal void, posterior to the upper dens, on sagittal MR imaging (see Fig. 6 ) and can be visualized on axial T1-weighted MR imaging and axial CT. Posterior to the dens, the dura, tectorial membrane, and vertical part of the cruciform ligament are imaged as a single vertical band of low signal intensity on sagittal T1-weighted MR imaging (see Figs. 5 and 6 ).
Because the anterior longitudinal ligament (see Fig. 1 ) is cord-like and adjacent to the anterior atlanto-occipital membrane above C1 (see Figs. 5 and 6 ), differentiation may be difficult, especially in sagittal MR imaging; however, the anterior longitudinal ligament is distinct between the body of C2 and the anterior arch of C1. The posterior atlanto-occipital membrane and posterior atlantoaxial membrane are adjacent to the dura and appear as a single line of low signal on MR imaging (see Figs. 5 and 6 ).
Apical and alar ligaments between the superior margin of the dens and the condyles and basion of the occipital bone, which are best identified on CT, pass through the supraodontoid space (see Fig. 6; Fig. 7 ). The supraodontoid space lies between the alar ligaments and foramen magnum and between the tectorial and atlanto-occipital membranes and is divided into a pair of symmetric halves by the apical ligament and a thin fatty membrane. The contents, dorsally to ventrally, lie deep in relation to a thin subtectorial membrane.
The clinical features of lesions at the CVJ are diverse and depend completely on the type and degree of deformity of the regional structures. The vital structures, including the brain stem, upper cervical spinal cord, cervical nerve roots, vertebral arteries, and anterior spinal artery, can become compressed. Suboccipital and neck pain (encountered in 82% of patients with CVJ lesions) is the most common sign. Brain stem, lower cranial nerve, and spinal cord compression may cause sleep apnea, dysphagia, nystagmus, dysphasia, nasal regurgitation, tongue atrophy, motor deficits, and bladder dysfunction. Occasionally, vascular symptoms, such as intermittent loss of consciousness, loss of visual fields, vertigo provoked by extension or rotation of the head, and basilar migraine, have been reported. The classification of disorders of the CVJ is summarized in Box 1 .
Congenital malformations
- I
Malformations of occipital bone
- A.
Platybasia
- B.
Basioccipital hypoplasia (basilar invagination)
- C.
Condylar hypoplasia
- D.
Condylar dysplasia (condylus tertius, paracondyloid process, and basilar process)
- A.
- II
Malformations of the atlas
- A.
Atlas assimilation
- B.
Aplasia and hypoplasia of the atlas
- C.
Atlas arch anomaly
- A.
- III
Malformations of the axis and odontoid process
- A.
Aplasia or hypoplasia of the dens
- B.
Persistent ossiculum terminale
- C.
Os odontoideum
- D.
Klippel-Feil anomaly
- A.
- I
Developmental and acquired
- I
Traumatic
- A.
Clival fractures
- B.
Occipital condyle fractures
- C.
Atlanto-occipital dislocations
- D.
Atlas fractures, including Jefferson’s fractures
- E.
Axial fractures, including odontoid fracture
- F.
Hangman’s fractures
- A.
- II
Inflammation and degenerative arthritis
- A.
Rheumatoid arthritis
- B.
Seronegative spondyloarthropathy (ankylosing spondylitis, psoriasis, and scleroderma)
- C.
Others arthritidis (gout, crystal pyrophosphate deposition disease, amyloidosis, pseudotumor, and pigmented villonodular synovitis)
- D.
Degenerative arthritis
- E.
Ossification of the posterior longitudinal ligament and diffuse idiopathic skeletal hyperostosis
- A.
- III
Infectious
- A.
Pyogenic (eg, Grisel’s syndrome)
- B.
Granulomatous (tuberculosis and others)
- C.
Epidural abscess
- A.
- IV
Neoplastic
- A.
Benign (fibrous dysplasia, aneurysmal bone cyst, osteoblastoma, osteochondroma, and chondroma)
- B.
Malignant
- 1.
Primary (chordoma, chondrosarcoma, and plasmacytoma)
- 2.
Secondary (multiple myeloma, metastatic disease, and nasopharyngeal malignancy)
- 1.
- A.
- I
Metabolic and genetic disorders
- A.
Metabolic (Morquio’s syndrome, Conradi’s syndrome, fetal warfarin syndrome, and renal rickets)
- B.
Genetic transformations (Down’s syndrome, osteogenesis imperfect, achondroplasia, Paget’s disease, and neurofibromatosis)
- A.
Occipital anomaly
Platybasia
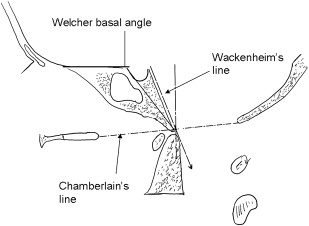
Platybasia refers to an increase in the Welcher basal angle ( Figs. 8 and 9 ). Platybasia alone does not usually cause symptoms unless it is associated with basilar invagination.
Basioccipital Hypoplasia
The basiocciput is derived from the fourth occipital sclerotome and forms the lowermost part of the clivus. Hypoplasia of the basiocciput may be mild or severe, depending on the number of occipital vertebrae affected. Plain radiographs allow detection of basilar invagination near the tip of the odontoid process located above Chamberlain’s line (see Fig. 8 ). The position of the Wackenheim clivus baseline is usually normal. Sagittal midline MR imaging can demonstrate shortening of the clivus ( Fig. 10 ) and the degree of cervicomedullary compression.
Basilar invagination (basilar impression) refers to upward herniation of the margins of the foramen magnum into the posterior fossa. Most patients with basilar invagination actually have a normal basal angle, and thus do not have associated platybasia. Basilar invagination is attributable to different underlying disorders of the CVJ. Clinically, basilar invagination can be primary or secondary. In primary basilar invagination, herniation is associated with other congenital CVJ anomalies, such as atlanto-occipital fusion, hypoplasia of C1 ( Fig. 11 ), spina bifida of the posterior arch of C1, Klippel-Feil syndrome, Chiari malformation, and skeletal dysplasias (eg, achondroplasia). In secondary basilar invagination, the change is attributable to softening or traumatic changes of bone, such as severe osteoporosis, hyperparathyroidism, osteomalacia, rickets, renal osteodystrophy, Paget’s syndrome, Hurler’s syndrome, and rheumatoid arthritis (RA). The most common associations with basilar invagination are Chiari malformation, occipitalization of C1, and fused upper vertebrae.
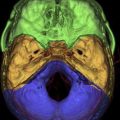
Occipital Condylar Hypoplasia
When occipital condyles are normally developed, the skull base descends medially. In condylar hypoplasia, the occipital condyles are underdeveloped and flat; as a result, the skull base is flattened or even ascends medially. Such change causes basilar invagination and widening of the atlanto-occipital joint axis angle. The lateral masses of C1 may be fused to the hypoplastic condyles ( Fig. 12 ), further accentuating the basilar invagination. Clinically, condylar hypoplasia limits, or may even abolish, movements at the atlanto-occipital joint and may occasionally lead to compression of the vertebral artery secondary to excessive posterior gliding of the occiput in relation to the atlas (C1).
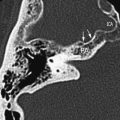
Condylus Tertius (Third Occipital Condyle)
When the hypochordal bow of the fourth occipital sclerotome (proatlas) persists or when the proatlas fails to integrate, an ossified remnant may be present at the distal end of the clivus, called the condylus tertius or third occipital condyle. Although typically single, multiple supranumerary ossicles may be present. It is usually directly above and anterior to the arch of C1 ( Fig. 13 ). This third condyle may form a joint or pseudojoint with the clivus, odontoid process, or anterior arch of C1. Although mostly asymptomatic, a condylus tertius (if large enough) may lead to limitation in the range of motion of the CVJ. An increased prevalence of os odontoideum is associated with this abnormality.
Occipital anomaly
Platybasia
Platybasia refers to an increase in the Welcher basal angle ( Figs. 8 and 9 ). Platybasia alone does not usually cause symptoms unless it is associated with basilar invagination.
Basioccipital Hypoplasia
The basiocciput is derived from the fourth occipital sclerotome and forms the lowermost part of the clivus. Hypoplasia of the basiocciput may be mild or severe, depending on the number of occipital vertebrae affected. Plain radiographs allow detection of basilar invagination near the tip of the odontoid process located above Chamberlain’s line (see Fig. 8 ). The position of the Wackenheim clivus baseline is usually normal. Sagittal midline MR imaging can demonstrate shortening of the clivus ( Fig. 10 ) and the degree of cervicomedullary compression.
Basilar invagination (basilar impression) refers to upward herniation of the margins of the foramen magnum into the posterior fossa. Most patients with basilar invagination actually have a normal basal angle, and thus do not have associated platybasia. Basilar invagination is attributable to different underlying disorders of the CVJ. Clinically, basilar invagination can be primary or secondary. In primary basilar invagination, herniation is associated with other congenital CVJ anomalies, such as atlanto-occipital fusion, hypoplasia of C1 ( Fig. 11 ), spina bifida of the posterior arch of C1, Klippel-Feil syndrome, Chiari malformation, and skeletal dysplasias (eg, achondroplasia). In secondary basilar invagination, the change is attributable to softening or traumatic changes of bone, such as severe osteoporosis, hyperparathyroidism, osteomalacia, rickets, renal osteodystrophy, Paget’s syndrome, Hurler’s syndrome, and rheumatoid arthritis (RA). The most common associations with basilar invagination are Chiari malformation, occipitalization of C1, and fused upper vertebrae.
Occipital Condylar Hypoplasia
When occipital condyles are normally developed, the skull base descends medially. In condylar hypoplasia, the occipital condyles are underdeveloped and flat; as a result, the skull base is flattened or even ascends medially. Such change causes basilar invagination and widening of the atlanto-occipital joint axis angle. The lateral masses of C1 may be fused to the hypoplastic condyles ( Fig. 12 ), further accentuating the basilar invagination. Clinically, condylar hypoplasia limits, or may even abolish, movements at the atlanto-occipital joint and may occasionally lead to compression of the vertebral artery secondary to excessive posterior gliding of the occiput in relation to the atlas (C1).
Condylus Tertius (Third Occipital Condyle)
When the hypochordal bow of the fourth occipital sclerotome (proatlas) persists or when the proatlas fails to integrate, an ossified remnant may be present at the distal end of the clivus, called the condylus tertius or third occipital condyle. Although typically single, multiple supranumerary ossicles may be present. It is usually directly above and anterior to the arch of C1 ( Fig. 13 ). This third condyle may form a joint or pseudojoint with the clivus, odontoid process, or anterior arch of C1. Although mostly asymptomatic, a condylus tertius (if large enough) may lead to limitation in the range of motion of the CVJ. An increased prevalence of os odontoideum is associated with this abnormality.
Atlas anomaly
Occipital Assimilation of the Atlas (Occipitalization of the Atlas)
Occipital assimilation of the atlas refers to congenital fusion of C1 with the occiput. It results from failure of segmentation between the fourth occipital sclerotome and first spinal sclerotome and failure of the hypochordal bow to separate from the fourth occipital sclerotome. It can be found in 0.14% to 0.25% of the population. The assimilation may be complete ( Fig. 14 A ) or partial ( Fig. 14 B; Table 2 ). The most common type is assimilation of the anterior arch of C1 with the anterior rim of the foramen magnum (see Fig. 14 A). On lateral plain radiographs, the C1 arches appear too high when incompletely assimilated and are not visible at all when completely assimilated. It invariably results in basilar invagination (see Fig. 12; Fig. 15 ). There is an increased prevalence of associated Klippel-Feil anomaly in C1 and C2. When this is present, gradual loosening of the atlantodental joint with progressive atlantoaxial subluxation or dislocation may occur. This condition is attributable to chronic excessive movement at the atlantoaxial joint, with consequent greater stress on ligaments connecting C1 and C2, especially the transverse ligament. In some instances, occipital assimilation of C1 may be associated with sudden death.
| Type I | Partial assimilation |
| Type II | Type 1 + Klippel-Feil anomaly of C2 and C3 |
| Type III | Complete assimilation, basilar invagination, and maldevelopment of transverse ligament causing atlantoaxial dislocation |
| Type IV | Complete assimilation associated with multiple malformations, including C2-to-C3 fusion, hemivertebrae, dens aplasia, tertiary condyle, and C2-to-C3 spondylolisthesis |
Arch Anomaly
Aplasia and hypoplasia are rare. The most common arch anomaly in C1 is posterior arch rachischisis ( Fig. 16 ), which is present in 4% of adult autopsy specimens. In 97% of cases, this defect is located midline, and in 3%, the cleft is located in the lateral aspect of C1 and through the sulcus of the vertebral artery. Anterior arch rachischisis is rare, occurring in only 0.1% of autopsy specimens. When it occurs in association with posterior arch rachischisis, the term split atlas is applied.