Jugular foramen, albeit complex, is essentially a bony conduit transmitting nerves and vessels from the posterior cranial fossa to the nasopharyngeal carotid space. In addition to its intrinsic pathologic conditions, a variety of lesions can arise from the contiguous surrounding structures and invade the foramen. A thorough understanding of the anatomy of this region is fundamental for diagnostic evaluation and assessment of its disease extent. Vascular variants and imaging artifacts are potential pitfalls, which should be recognized and avoided.
The jugular foramen is a complex crossroad of neurovascular structures deep in the skull base. It is inaccessible to clinical examination, and safe surgical approach is often hindered by crucial surrounding structures. Radiology plays a central role in the diagnostic evaluation and management planning of jugular foramen lesions.
A jugular foramen lesion may originate from its intrinsic contents, or arise from the surrounding structures and involve the foramen secondarily. Normal variants and imaging artifacts are not infrequent in this region, simulating diseases. Although pain and lower cranial nerve palsies are expected, otologic symptoms are often the initial complaints in these patients.
Optimal assessment of jugular foramen diseases requires both MR imaging and CT with thin-section bone algorithm. MR imaging shows the exact soft tissue extent of lesions, whereas CT allows precise evaluation of the surrounding bone changes. Angiography outlines a vascular road map for surgeons, and preoperative embolization may be of value for certain hypervascular tumors.
This article presents an overview of the anatomy of the jugular foramen with its variants and anomalies, and illustrates the pathologic processes that may involve the foramen.
Applied anatomy of jugular foramen
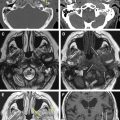
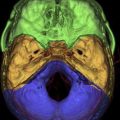
Embryologically, the jugular foramen is established from the union of the otic capsule and the basioccipital plate, forming a canal-like aperture between the petrous temporal bone and the condylar occipital bone. It has a complex oblique course running anteriorly, then laterally, and eventually inferiorly through the skull base into the carotid space. It is separated anteromedially from the carotid canal by the caroticojugular spine and inferomedially from the hypoglossal canal by the jugular tubercle ( Fig. 1 ).
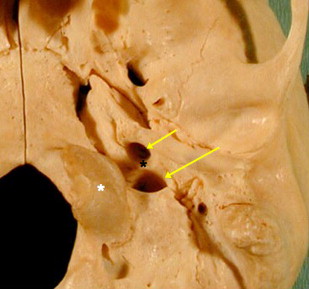
On coronal imaging, the jugular tubercle has a classic “eagle’s head” configuration, an important anatomic landmark in locating and separating the jugular foramen from the hypoglossal canal ( Fig. 2 ).

Conventionally, the jugular foramen is divided into a smaller anteromedial pars nervosa, which transmits the inferior petrosal sinus and the glossopharyngeal (IXth) nerve with its tympanic branch (Jacobsen nerve), and a larger posterolateral pars vascularis, which contains the jugular bulb, the vagus (Xth) nerve with its auricular branch (Arnold nerve), the accessory (XIth) nerve, and the posterior meningeal artery. The two compartments are separated by a fibrous septum that extends from the jugular spine of the petrous temporal bone to the condylar occipital bone ( Fig. 3 ). Complete ossification of this septum may occur, dividing the foramen into two discrete openings. Several microanatomic studies showed, however, that this conventional compartmentalization of the jugular foramen might be an oversimplification that lacked surgical significance. Division of the jugular foramen is only found at its endocranial opening, and not throughout the foramen. In addition, the Xth and XIth nerves may travel through the pars nervosa, instead of the pars vascularis.
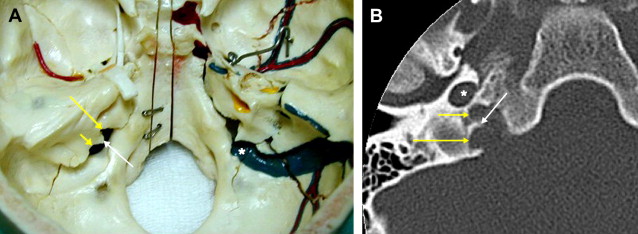
After entering the jugular foramen, the IXth nerve turns and forms a genu, which is lodged near the external opening of the cochlear aqueduct, before coursing inferiorly into the carotid space. Extreme care is essential during a translabyrinthine surgery to avoid injuring the IXth nerve genu. The IXth nerve has two ganglia within the foramen. The Jacobsen nerve arises from the inferior ganglion and runs through the inferior tympanic canaliculus of the caroticojugular spine into the hypotympanum, where it forms the tympanic plexus over the cochlear promontory.
The Xth and XIth nerves share a fibrous sheath throughout the jugular foramen. Their nerve fibers intermingle and are inseparable by microdissection. The Xth nerve expands into its superior ganglion within the foramen, from which the Arnold nerve arises and passes through the mastoid canaliculus into the facial nerve canal (mastoid segment) before exiting by the tympanomastoid fissure into the external auditory canal. The XIth nerve has no branch in the jugular foramen.
The cranial nerves within the jugular foramen cannot be visualized using the conventional MR imaging protocols. They may be seen, however, on contrast-enhanced three-dimensional fast imaging using steady-state acquisition. The steady-state sequence provides high contrast and spatial resolutions using a refocused gradient-echo sequence, whereas enhancement of the adjacent jugular vein and venous plexuses further increases the contrast between the cranial nerves and their surrounding.
The inferior petrosal sinus is the main drainage outlet of the cavernous sinus. It runs along the petroclival fissure into the pars nervosa, where it forms a multichannel confluence that empties into the jugular bulb. The posterior meningeal artery, usually a branch of the ascending pharyngeal artery, ascends through the jugular foramen adjacent to the Xth and XIth nerves to supply the posterior fossa meninges.
Jugular bulb variants and anomalies
On entering the jugular foramen, the sigmoid sinus turns laterally and expands into the jugular bulb (see Fig. 3 ). The right jugular bulb is larger than the left in 75% of individuals. There are a number of important jugular bulb variants and anomalies that should be recognized.
Jugular Bulb Pseudolesion
MR imaging flow phenomenon is frequently detected in the jugular bulb, simulating an intraluminal thrombus or tumor. It is more commonly seen on the right side when complex flow within an asymmetrically large and often high jugular bulb results in high or intermediate signal intensity, particularly on the T1-weighted images ( Fig. 4 A ). These jugular bulb pseudolesions are indeed the most common jugular foramen “lesions.”
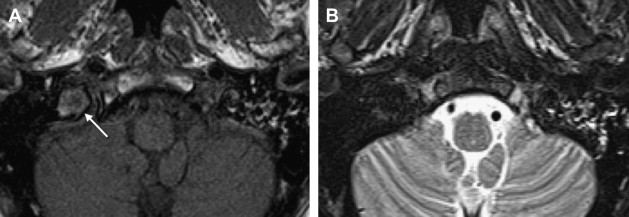
By definition, jugular bulb pseudolesions are asymptomatic and found incidentally during unrelated MR imaging. When a pseudolesion is suspected, careful scrutiny usually reveals that the flow phenomenon does not hold up on all MR imaging sequences ( Fig. 4 B). A phase-contrast MR venogram is also useful in demonstrating a patent jugular bulb with normal flow, excluding any intraluminal lesion. A high-resolution CT of the temporal bone further fortifies the confidence regarding absence of any pathologic condition by showing an intact jugular spine and cortical margin of the jugular foramen. This potential imaging pitfall should be recognized by radiologists, sparing patients from any unnecessary “interventions.”
High-riding and Dehiscent Jugular Bulb
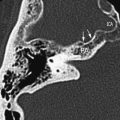
Conventionally, a high-riding jugular bulb is defined as a jugular bulb with its roof extending above the inferior tympanic annulus. Some authors used the inferior margin of the basal turn of cochlea as the criterion ( Fig. 5 ). High-riding jugular bulbs are more common on the right side, with an incidence of 4% to 24%. Although it is a normal variant, detection of a high-riding jugular bulb is nonetheless important, particularly during evaluation of cerebellopontine angle lesions. Its presence compromises the operative window during a translabyrinthine surgery and precludes adequate exposure of the inferior compartment of the inner ear and the cerebellopontine angle. Modified surgical techniques, such as transotic or retrosigmoid approaches, may be required.

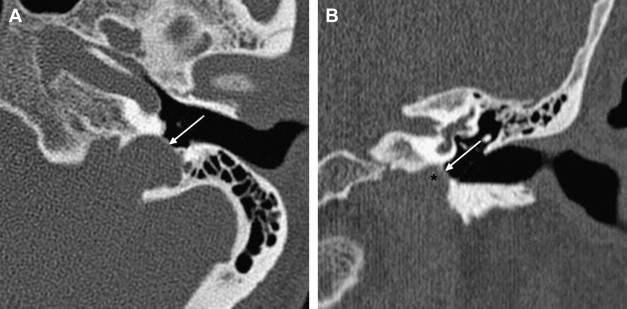
A high jugular bulb may be associated with focal dehiscence of the jugular (sigmoid) plate, allowing protrusion of the bulb superolaterally into the posterior hypotympanum ( Fig. 6 ). This dehiscent jugular bulb is seen as a bluish posteroinferior retrotympanic mass on otoscopy. Most of these patients are asymptomatic, although some may complain of low rumble pulsatile tinnitus or conductive hearing loss secondary to obliteration of the round window niche or impingement of the ossicular chain. More importantly, it is imperative that surgeons are alerted to this anatomic variant, in view of the high risk of torrential bleeding should a myringotomy or exploratory tympanotomy be performed in these patients.
Jugular Bulb Diverticulum
Jugular bulb diverticulum was once thought to be rare, with only a limited number of reported cases in the English literature. It is now believed, however, that this condition has been significantly underdiagnosed.
A jugular bulb diverticulum is an out-pouching, often but not always, from a high-riding jugular bulb. Some authors suggested that it represented a variant of high-riding jugular bulb that extended into the petrous temporal bone only to be partly hindered by the dense otic capsule, whereas others considered it a true anomaly that enlarged with time. Interestingly, they are more commonly found on the left side, despite the well-known dominance of the right-sided jugular bulbs.
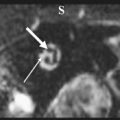
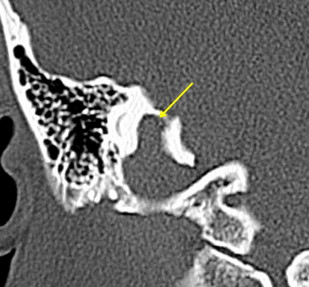
The diverticulum most commonly protrudes superomedially into the petrous temporal bone between the internal acoustic canal and the vestibular aqueduct. It is best demonstrated on high-resolution temporal bone CT as a well-corticated polypoid projection from the jugular bulb margin ( Fig. 7 ). Most are found incidentally, although some individuals may present with sensorineural hearing loss caused by erosion of the internal acoustic canal, or Meniere’s disease–like symptoms secondary to encroachment of the endolymphatic duct within the vestibular aqueduct.
Jugular bulb variants and anomalies
On entering the jugular foramen, the sigmoid sinus turns laterally and expands into the jugular bulb (see Fig. 3 ). The right jugular bulb is larger than the left in 75% of individuals. There are a number of important jugular bulb variants and anomalies that should be recognized.
Jugular Bulb Pseudolesion
MR imaging flow phenomenon is frequently detected in the jugular bulb, simulating an intraluminal thrombus or tumor. It is more commonly seen on the right side when complex flow within an asymmetrically large and often high jugular bulb results in high or intermediate signal intensity, particularly on the T1-weighted images ( Fig. 4 A ). These jugular bulb pseudolesions are indeed the most common jugular foramen “lesions.”
By definition, jugular bulb pseudolesions are asymptomatic and found incidentally during unrelated MR imaging. When a pseudolesion is suspected, careful scrutiny usually reveals that the flow phenomenon does not hold up on all MR imaging sequences ( Fig. 4 B). A phase-contrast MR venogram is also useful in demonstrating a patent jugular bulb with normal flow, excluding any intraluminal lesion. A high-resolution CT of the temporal bone further fortifies the confidence regarding absence of any pathologic condition by showing an intact jugular spine and cortical margin of the jugular foramen. This potential imaging pitfall should be recognized by radiologists, sparing patients from any unnecessary “interventions.”
High-riding and Dehiscent Jugular Bulb
Conventionally, a high-riding jugular bulb is defined as a jugular bulb with its roof extending above the inferior tympanic annulus. Some authors used the inferior margin of the basal turn of cochlea as the criterion ( Fig. 5 ). High-riding jugular bulbs are more common on the right side, with an incidence of 4% to 24%. Although it is a normal variant, detection of a high-riding jugular bulb is nonetheless important, particularly during evaluation of cerebellopontine angle lesions. Its presence compromises the operative window during a translabyrinthine surgery and precludes adequate exposure of the inferior compartment of the inner ear and the cerebellopontine angle. Modified surgical techniques, such as transotic or retrosigmoid approaches, may be required.
A high jugular bulb may be associated with focal dehiscence of the jugular (sigmoid) plate, allowing protrusion of the bulb superolaterally into the posterior hypotympanum ( Fig. 6 ). This dehiscent jugular bulb is seen as a bluish posteroinferior retrotympanic mass on otoscopy. Most of these patients are asymptomatic, although some may complain of low rumble pulsatile tinnitus or conductive hearing loss secondary to obliteration of the round window niche or impingement of the ossicular chain. More importantly, it is imperative that surgeons are alerted to this anatomic variant, in view of the high risk of torrential bleeding should a myringotomy or exploratory tympanotomy be performed in these patients.
Jugular Bulb Diverticulum
Jugular bulb diverticulum was once thought to be rare, with only a limited number of reported cases in the English literature. It is now believed, however, that this condition has been significantly underdiagnosed.
A jugular bulb diverticulum is an out-pouching, often but not always, from a high-riding jugular bulb. Some authors suggested that it represented a variant of high-riding jugular bulb that extended into the petrous temporal bone only to be partly hindered by the dense otic capsule, whereas others considered it a true anomaly that enlarged with time. Interestingly, they are more commonly found on the left side, despite the well-known dominance of the right-sided jugular bulbs.
The diverticulum most commonly protrudes superomedially into the petrous temporal bone between the internal acoustic canal and the vestibular aqueduct. It is best demonstrated on high-resolution temporal bone CT as a well-corticated polypoid projection from the jugular bulb margin ( Fig. 7 ). Most are found incidentally, although some individuals may present with sensorineural hearing loss caused by erosion of the internal acoustic canal, or Meniere’s disease–like symptoms secondary to encroachment of the endolymphatic duct within the vestibular aqueduct.