Acute pyelonephritis is a bacterial infection of the renal parenchyma and collecting system. Diagnosis is based on clinical findings of fever, flank pain, and urinary tract infection. Computed tomography findings include renal enlargement with wedge-shaped heterogeneous areas of decreased enhancement, known as a “striated nephrogram.” Imaging is primarily used to diagnose complications such as emphysematous pyelonephritis, renal abscess, and pyonephrosis. Chronic pyelonephritis can have varying appearances on imaging ranging from xanthogranulomatous pyelonephritis or, in extreme cases, renal replacement lipomatosis.
Key points
- •
Pyelonephritis commonly occurs as a complication of ascending urinary tract infection manifesting as a unilateral or bilateral striated nephrogram on imaging.
- •
Complications of pyelonephritis include emphysematous pyelonephritis appearing as gas within the renal parenchyma on imaging and renal abscess signified by a rim-enhancing cystic renal mass.
- •
Pyonephrosis is one of the few urologic emergencies requiring urgent drainage. A peripherally enhancing, thickened, and dilated renal pelvis is concerning for pyonephrosis.
- •
Chronic pyelonephritis is a spectrum of long-standing renal infection including xanthogranulomatous pyelonephritis and renal replacement lipomatosis.
Introduction
Urinary tract infection (UTI) is the most common urologic disease in the United States, accounting for more than 10 million office and 2 to 3 million emergency department visits every year. Typically, in adults the diagnosis of a UTI is established with patient history, physical examination, and urinalysis. Per American College of Radiology appropriateness criteria, diagnostic imaging is reserved for complex patients with either treatment failure or when there is concern for complications such as pyelonephritis or an abscess, especially in the setting of diabetes mellitus, immunosuppression, or stones.
Etiology
Ascending Infection
The urinary tract is a tubular system that opens at the body’s surface as the urethra, which makes it susceptible to colonization by infectious organisms that include both gram-negative and gram-positive bacteria, as well as certain fungi. The most common causative agent is Escherichia coli . UTIs are more common in women than men because of the shorter length of the urethra. In most cases, the infection is confined to the urinary bladder. An ascending migration of the pathogens through the ureters into the kidneys can lead to a complicated UTI, which includes a spectrum of acute and chronic renal infectious pathology, discussed as follows.
Descending Infection
In patients with bacteremia, sepsis, or infective endocarditis, the bloodborne pathogens can seed into the kidneys by crossing the tubular epithelium barrier followed by parenchymal colonization and infection.
Renal Stones
The presence of renal stones increases the risk of complicated UTI. The obstruction of the urinary tract by renal stones leads to urinary stasis with entrapment and proliferation of bacteria. The major types of renal stones include calcium oxalate (most common), calcium phosphate, struvite, uric acid, cysteine, xanthine, and protein matrix stones. The struvite stones are composed of magnesium ammonium phosphate and calcium carbonate-apatite and can cause chronic upper UTI with urease-producing organisms such as Proteus and Klebsiella . Overall, renal stones are more common in men with a prevalence of 10.6%, compared with 7.1% among women. However, struvite stones are more common in women, with a frequency of 10% to 15% and can grow rapidly into a large calculus involving and conforming to the shape of the entire renal collecting system that resembles a staghorn or coral ( Fig. 1 ). If left untreated, the complication rate can reach up to 75%, including renal failure and life-threatening urosepsis.

Pathology
Acute Pyelonephritis
Acute pyelonephritis denotes an infection of the renal pelvis, calyces, and parenchyma and presents predominantly in adult women. Almost always, the infection ascends from the urinary bladder or spreads to the kidneys hematogenously. Clinically, the patient presents with fever, dysuria, flank pain, and costovertebral angle tenderness. The diagnosis is confirmed with bacterial growth in the urine culture.
Imaging features
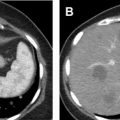
The diagnosis of acute pyelonephritis is clinical, and imaging is generally used to assess for complications. Ultrasound is frequently used as the initial imaging modality, but the most common finding is a normal examination. When present, sonographic features of acute pyelonephritis include loss of corticomedullary differentiation, increased renal size, loss of renal sinus fat due to edema, dilated renal pelvis, and urothelial thickening. The change in renal echogenicity commonly occurs in a linear or wedge-shaped pattern that could be increased due to hemorrhage, or decreased due to edema. The alternating pattern of increased renal echogenicity with normal renal parenchyma is termed as echogenic “striation.” Focal pyelonephritis can appear as a masslike area of abnormal echogenicity, especially in patients with diabetes mellitus or immunosuppression. On Doppler interrogation, areas of hypoperfusion are identified that correspond to the changes in echogenicity ( Fig. 2 A).

Computed tomography (CT) is preferred in the evaluation of acute pyelonephritis because of its excellent ability to detect complications such as gas, hemorrhage, obstruction, or stones. The “striated nephrogram” is the classic appearance that occurs as inflammation selectively increases parenchymal pressure leading to intratubular edema and obstruction, which is then manifested as alternating bands of high and low parenchymal attenuation on CT oriented to the axis of the renal tubules and collecting ducts ( Fig. 2 B). This can be unilateral or bilateral, and the affected kidney is often enlarged and edematous with or without perinephric fat stranding. In addition, smooth urothelial thickening and enhancement also may be seen.
Differential diagnosis and pitfalls
The “striated nephrogram” is not specific for acute pyelonephritis ( Table 1 ). Any process that increases the pressure within the renal parenchyma can lead to this pattern of enhancement. Unilateral etiologies include renal vein thrombosis, renal contusion, or ureteric obstruction. , Differentiation between focal pyelonephritis and segmental renal infarction can be challenging ( Table 2 ). In such cases, the “cortical rim sign” can be very helpful, which is seen due to preserved outer rim of renal cortex being perfused by perforating collateral vessels in the presence of occlusion of main or smaller renal arteries in the affected kidney ( Fig. 3 A). Bilateral striated nephrograms are associated with contrast-associated acute kidney injury, hypotension, renal infarcts, and autosomal recessive polycystic kidney disease ( Fig. 3 B). Another potential pitfall is infiltrating transitional cell carcinoma that invades the renal parenchyma, thus causing a delayed cortical nephrogram that can mimic a “striated nephrogram” appearance ( Fig. 3 C).
| Unilateral | Bilateral |
|---|---|
|
|
| Focal Pyelonephritis | Segmental Renal Infarction |
|---|---|
|
|

Emphysematous Pyelonephritis
Emphysematous pyelonephritis is a life-threatening necrotizing infection of the renal parenchyma with gas-forming organisms. Patients with emphysematous pyelonephritis are extremely ill with fever and flank pain. When gas is confined to the collecting system, the term emphysematous pyelitis, an important differentiator from parenchymal gas, is implied, which can be managed conservatively with antibiotic treatment. The most common gas-forming organism is E coli (68%) followed by Klebsiella pneumoniae (10%). Emphysematous pyelonephritis almost exclusively occurs in patients with poorly controlled diabetes mellitus, where the elevated levels of glucose inhibit the normal function of leukocytes, impairing the body’s defense against infection. ,
Imaging features
Conventional radiography has a sensitivity of 66% to 70% for detection of gas in the kidneys. The gas is commonly present in a radial pattern along the renal pyramids ( Fig. 4 A). On gray scale ultrasound, highly echogenic areas within the renal sinuses and parenchyma are identified with associated ring down artifact representing gas, commonly referred to as “dirty shadowing” ( Fig. 4 B). When present in the perinephric space, gas can obscure the visualization of the kidney. On CT, the characteristic finding is intraparenchymal, intracaliceal, or intrapelvic gas, often extending into the subcapsular space or even across the Gerota fascia, indicative of a more advanced stage of renal necrosis ( Fig. 4 C).

Wan and colleagues identified 2 types of emphysematous pyelonephritis depending on presence of fluid and their gas pattern. The mortality rate in the 2 subtypes correlates with degree of parenchymal destruction. Type 1 emphysematous pyelonephritis is more fulminant and occurs in approximately 33% of cases. There is destruction of more than one-third of the renal parenchyma, however, without any fluid collection ( Fig. 5 A). Gas may be intraparenchymal, or present with in a crescentic pattern in the subcapsular or perinephric region. The associated mortality rate is as high as 69%. Treatment is nephrectomy ( Fig. 5 B). Type 2 emphysematous pyelonephritis is associated with destruction of less than one-third of the renal parenchyma, with gas associated with renal or perirenal abscesses ( Fig. 5 C). The gas is typically confined to the abscess or may be seen within the renal pelvis and has a lower mortality at 18%. Treatment is percutaneous drainage or in severe cases, nephrectomy.

Renal Abscess
Renal abscess is defined as necrosis of the renal parenchyma that commonly develops as a complication of focal pyelonephritis. These are usually solitary and unilateral. The complications include rupture of the abscess into surrounding spaces leading to perinephric, subdiaphragmatic, or pelvic spread. A renal abscess should be suspected if appropriate treatment for pyelonephritis does not demonstrate any significant clinical improvement. Approximately 15% to 20% of patients with a renal abscess will have negative urine cultures.
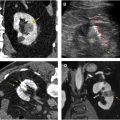
Imaging features
On grayscale ultrasound, an abscess presents as a hypoechoic well-circumscribed mass with poor through transmission, but without internal vascular flow on Doppler ( Fig. 6 A). Low-level internal echoes representing hemorrhage or debris are often identified. Gas within the abscess will cause dirty shadowing. Internal complexity is indicated by the presence of septations. On CT, an abscess presents as a cystic mass with thick peripheral enhancement called the “rim sign,” with perinephric fat stranding indicating an inflammatory process , ( Fig. 6 B).