A wide variety of abnormalities may be encountered in the paravertebral mediastinum, ranging from congenital lesions to malignant neoplasms. A combination of localizing mediastinal masses to the paravertebral compartment, characterizing them with cross-sectional imaging techniques, and correlating the imaging findings with demographics and other clinical history typically enables the development of a focused differential diagnosis. Radiologists must be familiar with these concepts in order to help guide subsequent imaging and/or intervention and, when appropriate, treatment planning for neoplasms and other abnormalities.
Key points
- •
A wide variety of neoplastic and non-neoplastic entities may originate from the paravertebral mediastinum.
- •
Neurogenic neoplasms are the most common paravertebral compartment masses and typically represent peripheral nerve sheath tumors, which manifest as smooth, round or oval masses in the paravertebral region on computed tomography.
- •
Non-neurogenic primary and secondary neoplasms are much less common than neurogenic tumors in the paravertebral mediastinum and may arise from osseous structures or soft tissues.
- •
Spinal infections typically are due to bacterial infections and result in ill-defined soft tissue, unorganized fluid, and/or loculated collections.
- •
Intrathoracic meningoceles are associated with neurofibromatosis type 1 and manifest as a unilocular mass of fluid attenuation, often associated with vertebral anomalies, such as hemivertebrae, butterfly vertebra, or spina bifida.
Introduction
The paravertebral mediastinal compartment contains several vascular and nonvascular organs and anatomic structures from which a wide variety of anatomic variants and abnormalities may arise. It has been well established that a combination of lesion localization, characterization with cross-sectional imaging modalities, and correlation with demographics and other clinical information typically enable the development of a focused differential diagnosis. The first step in this process is identifying the compartment from which a mediastinal mass originates, which can be accomplished by employing the mediastinal compartment classification scheme created by the International Thymic Malignancy Interest Group (ITMIG), which has been accepted as a standard.
The following boundaries have been defined for the paravertebral mediastinal compartment : superiorly, the thoracic inlet ; inferiorly, the diaphragm ; anteriorly, the posterior boundaries of the visceral compartment; and posterolaterally, a vertical line along the posterior margin of the chest wall at the lateral aspect of the transverse processes. With these anatomic landmarks in mind, the most significant organs and anatomic structures contained in the paravertebral compartment include the thoracic spine and paravertebral soft tissues. The most common masses and other abnormalities originating from the paravertebral compartment are neurogenic neoplasms, non-neurogenic tumors, infections (discitis/osteomyelitis), and those related to trauma (hematoma), although a wide variety of miscellaneous lesions related to other underlying conditions (such as extramedullary hematopoiesis) are possible.
Imaging of paravertebral abnormalities
General Considerations
Lesions in the paravertebral mediastinum typically originate from the thoracic spine and paravertebral soft tissues, the most common of which are neurogenic neoplasms. Primary lymphoma and bone tumors as well as metastatic disease are less common but may be seen. Non-neoplastic abnormalities include etiologies such as infections of the spine of the spine; cystic lesions, such as intrathoracic meningocele and neurenteric cyst; and extramedullary hematopoiesis. Although the composition, morphology, and other imaging features may be sufficient to make a specific diagnosis, in other cases, correlation with clinical information is necessary.
Neurogenic Neoplasms
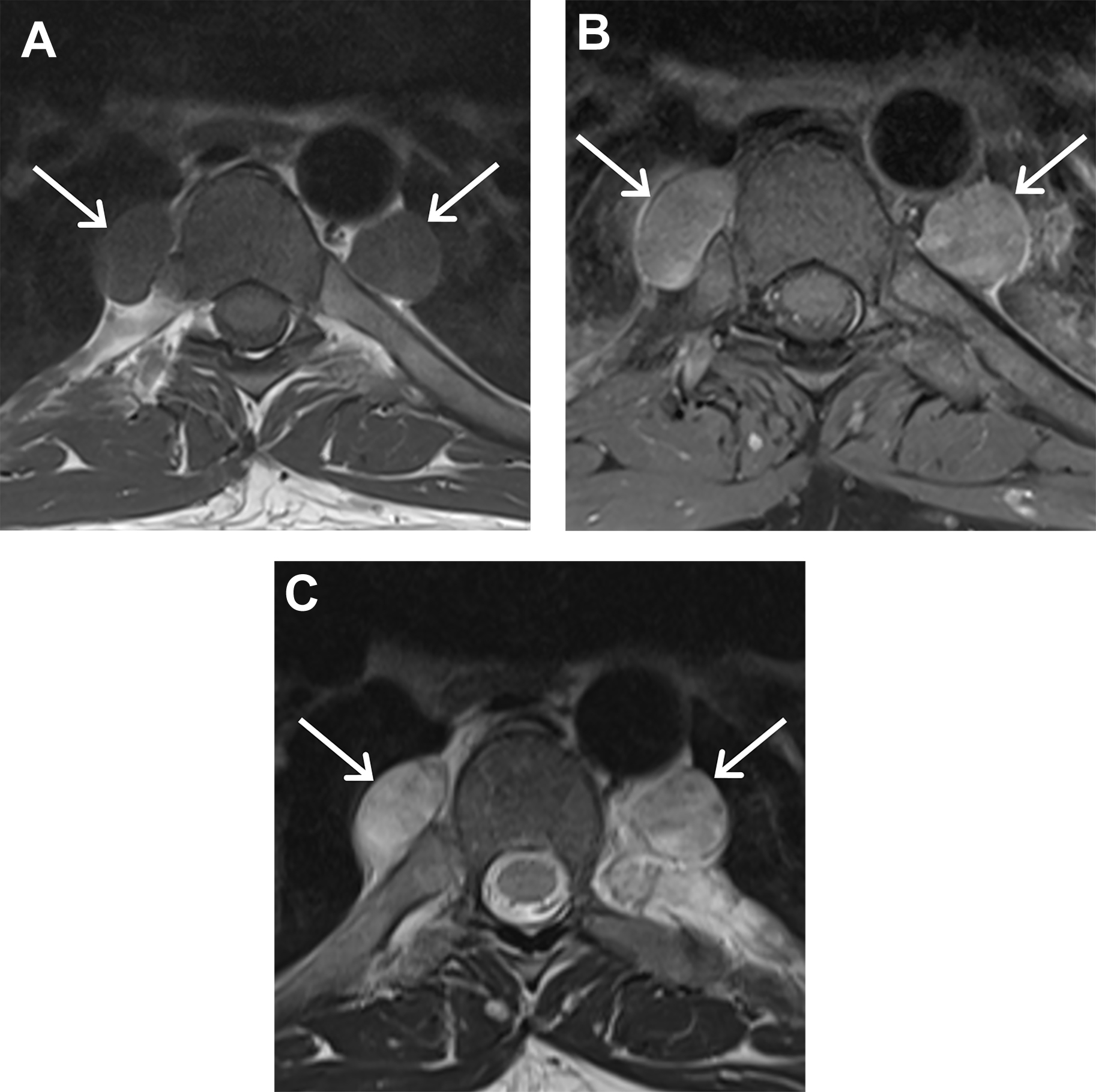
Neurogenic neoplasms are the most common paravertebral compartment masses and represent 20% and 35% of all adult and pediatric mediastinal neoplasms, respectively. Most of these lesions (70%–80%) are benign. Peripheral nerve sheath tumors originate from spinal or proximal intercostal nerves, less commonly from the vagus, recurrent laryngeal, or phrenic nerves, and represent 70% of mediastinal neurogenic neoplasms. Multiple neurofibromas may be encountered in patients with neurofibromatosis type 1. On computed tomography (CT), peripheral nerve sheath neoplasms, such as neurofibroma or schwannomas, manifest as smooth, round or oval masses in the paravertebral region that may exhibit a dumbbell shape and communicate with the spinal canal ( Fig. 1 ). Cystic changes or hemorrhage may result in regions of internal heterogeneity and are more common in schwannomas than in neurofibromas. Although pressure erosion of adjacent ribs or vertebrae and enlargement of the neural foramina may be seen, these are benign findings and should be differentiated from bone invasion and destruction, which are typical of malignancies. MR imaging offers the advantage of showing the extent of intraspinal/extradural extension and may be used in some instances to distinguish between the types of peripheral nerve sheath tumors based on unique signs ( Figs. 2 and 3 ). For example, multiple small, ringlike structures of low signal intensity representing fascicular bundles is known as the fascicular sign and typically is seen with schwannomas. On the other hand, the combination of central low signal intensity and surrounding peripheral high signal intensity is termed the target sign, and is seen more commonly with neurofibromas than with schwannomas.
For patients with neurofibromatosis type 1, there is a 10% lifetime risk of developing a malignant peripheral nerve sheath tumor. If a neurofibroma demonstrates imaging findings such as sudden increase in size, development of internal heterogeneity, and/or invasion of adjacent tissues, malignant transformation to a malignant peripheral nerve sheath neoplasm should be suspected. Differentiation between a malignant peripheral nerve sheath tumor and a benign neurofibroma may be accomplished with fluorodeoxyglucose PET/CT, with 1 study demonstrating sensitivity of 95% and specificity of 72%. Warbey and colleagues found sensitivity of 97% and specificity of 87% for the detection of malignant peripheral nerve sheath neoplasms. Additionally, the investigators suggested the following management based on maximum standardized uptake value (SUVmax): (1) lesions with SUVmax less than 2.5 should be considered benign; (2) masses with SUVmax greater than 3.5 should be considered malignant; and (3) lesions with SUVmax of 2.5 to 3.5 should undergo surveillance imaging.
Sympathetic ganglion neoplasms, such as ganglioneuromas, ganglioneuroblastomas, and neuroblastomas, and neuroendocrine neoplasms, such as paragangliomas, are other neurogenic tumors that may arise in the paravertebral mediastinum; however, these are much less common than peripheral nerve sheath tumors and many of the imaging features of these tumors are nonspecific, necessitating histologic assessment for diagnosis. Paragangliomas arise from clusters of neuroendocrine cells called paraganglia and are classified by location and secretory function. On contrast-enhanced CT, paragangliomas demonstrate intense enhancement. On MR imaging, lesions exhibit a salt-and-pepper appearance from enhancing tumor and signal flow voids of blood vessels on T1-weighted imaging and high signal intensity (light bulb appearance) on T2-weighted imaging.
Other Neoplasms
Non-neurogenic primary and secondary neoplasms also may be encountered in the paravertebral mediastinal compartment but are much less common than neurogenic tumors. The most common primary tumors to occur in this region may be classified as either osseous or soft tissue in origin, with chordoma and chondrosarcoma included in the former and lymphoma in the latter.
Although chordomas of the vertebral bodies are rare, they are the second most common primary malignancy in the spine following lymphoproliferative neoplasms.
The thoracic spine is the most infrequent portion of the spine involved, following the cervical and lumbar spine. On CT, chordomas typically manifest as well circumscribed destructive lytic lesions that may be heterogeneous due to the presence of necrosis and/or hemorrhage. The associated expansile soft tissue mass is often much larger than the osseous abnormality.
Internal foci of high attenuation appearing as intratumoral calcifications may be present, which are thought to represent sequestra of normal bone. On MR imaging, chordomas demonstrate intermediate to low signal intensity on T1-weighted imaging, high signal intensity on T2-weighted imaging, and heterogeneous enhancement with a honeycomb appearance following the administration of intravenous gadolinium contrast material. Chordomas tend to involve more than 1 vertebral body via extension across the intervertebral disc space and may spread to the epidural space, compressing the spinal cord or along the nerve roots, resulting in neural foraminal expansion.
Chondrosarcomas are malignant tumors of cartilaginous origin that represent approximately 25% of all primary malignant neoplasms of bone, although involvement of the spine accounts for only approximately 7% of cases. The thoracic spine is the most frequent portion of the spine affected. The posterior elements and vertebral body are involved in 45% of cases whereas location within the posterior elements only (40%) or the vertebral body only (15%) is less common. On CT, tumors are lytic approximately 50% of the time and contain internal calcifications that may be in a rings and arcs pattern or popcorn morphology. Endosteal scalloping may be present and affects greater than two-thirds of the cortical thickness of the bone affected. Higher-grade tumors may demonstrate a permeative pattern of bone destruction. On MR imaging, lesions demonstrate low to intermediate signal on T1-weighted imaging, high signal intensity in the regions without mineralization on T2-weighted imaging, and heterogeneous enhancement following the administration of intravenous gadolinium contrast material.
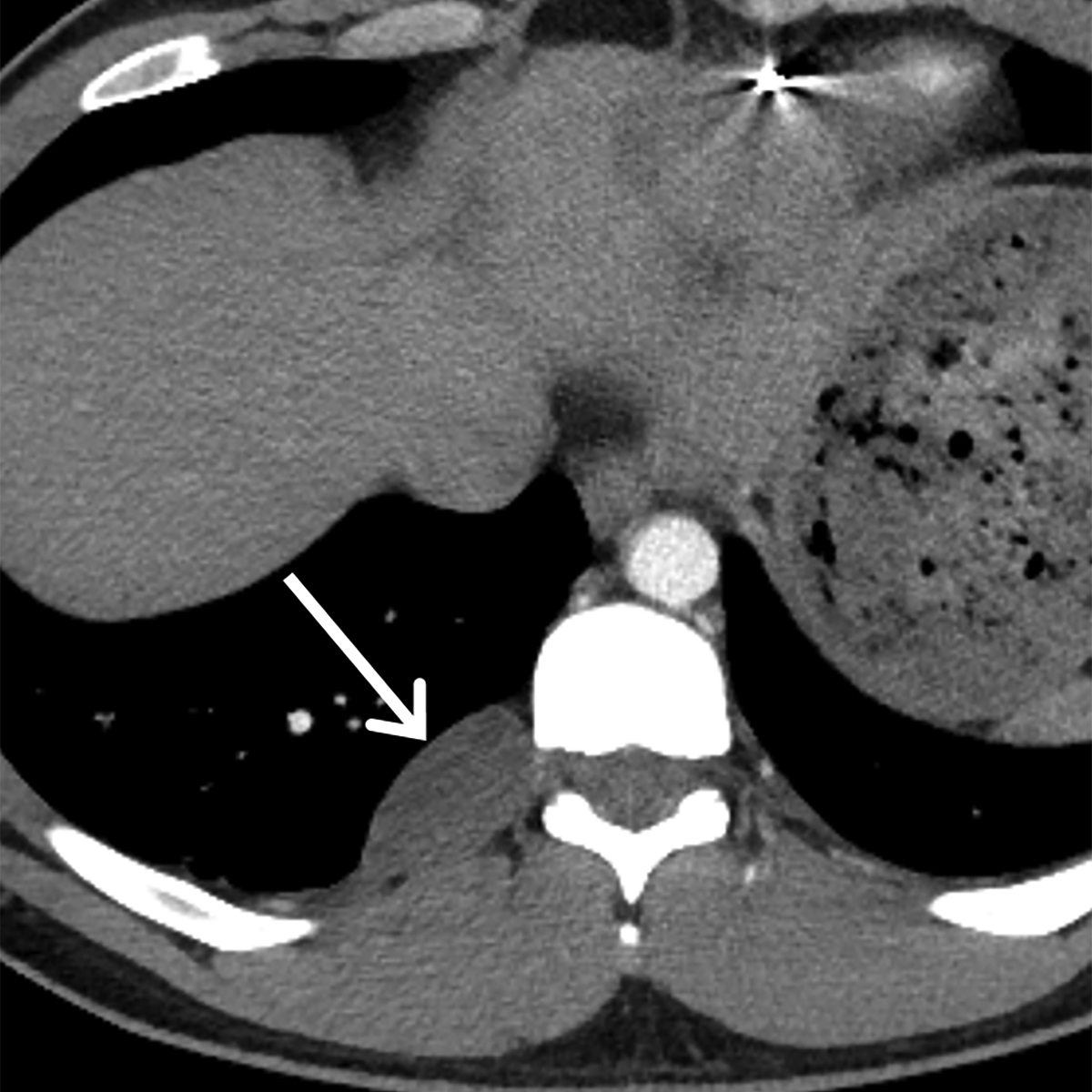
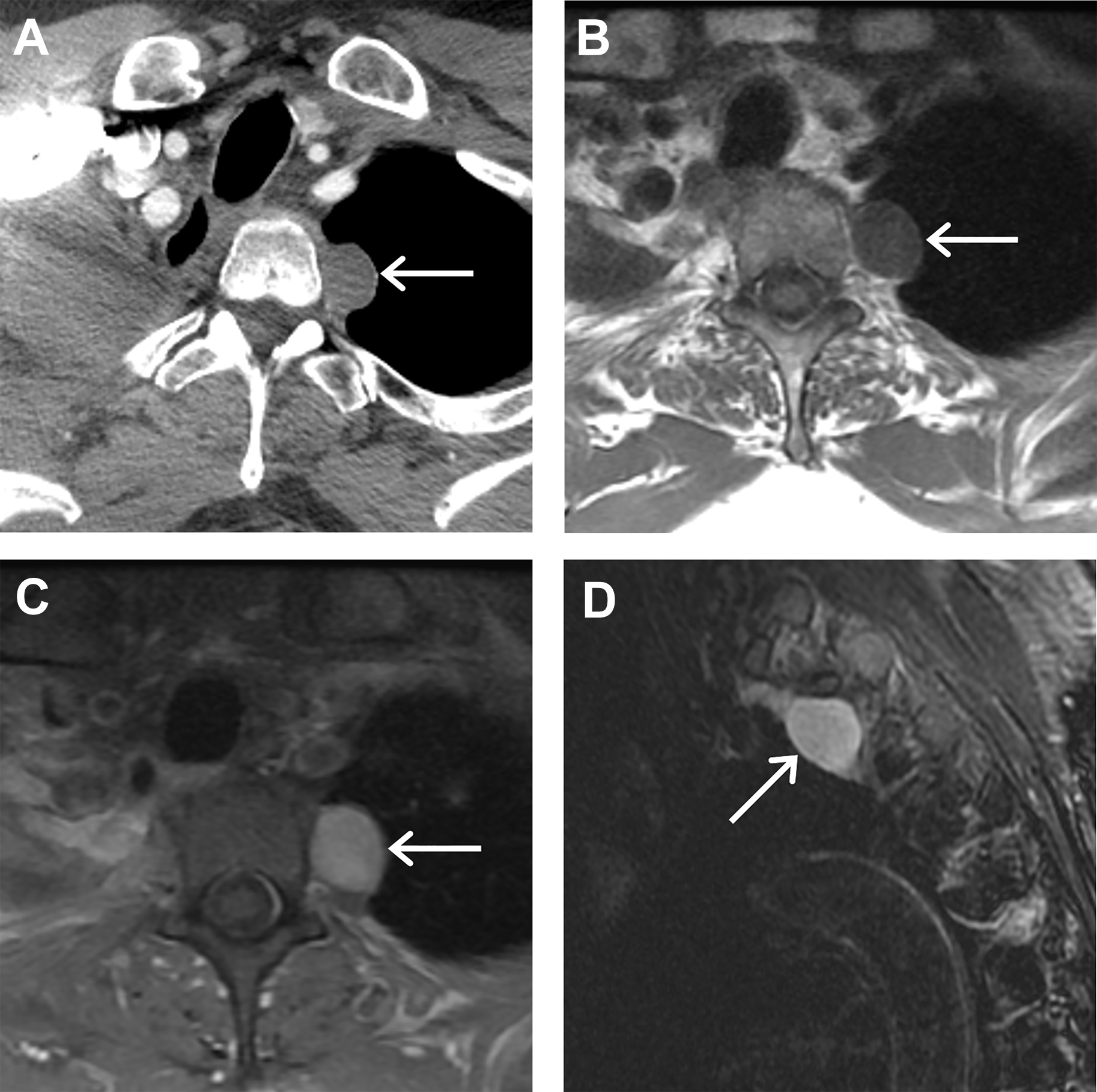
Non-neurogenic soft tissue tumors affecting the paravertebral mediastinum are uncommon and tend to represent lymphoma, metastatic disease, or a variety of unusual neoplasms. When lymphoma arises from the mediastinum as a primary malignant neoplasm, the paravertebral compartment is the least common site of involvement ( Fig. 4 ). A wide variety of neoplasms may metastasize to the paravertebral mediastinum and typically demonstrate the imaging characteristics of the primary tumor and metastases elsewhere in the body ( Fig. 5 ).