There is a plethora of surgical procedures that are performed in the eye and orbit. The consequences of these procedures can often be observed on diagnostic imaging through the presence of various implants and altered anatomy. The expected postoperative changes in the eye and orbit, the impact of implants on image quality and safety, and potential associated complications are reviewed in this article. Conventional computed tomography and MR imaging scans are useful for the postoperative assessment of the eye and orbit. The computed tomography and MR imaging findings related to the postoperative eye and orbit are reviewed in this article.
Key points
- •
There is a wide array of eye and orbit surgeries, ranging from eyelid, refractive, retinal, nasolacrimal drainage, and oncologic procedures.
- •
The effects of many of these surgeries can be observed on CT and MRI through the presence of various implants and altered anatomy.
- •
Imaging can be useful for assessing surgical complications, such as device malposition or migration.
Introduction
There is a plethora of surgical procedures that are performed in the eye and orbit. Although ultrasound and optical coherence tomography are often performed for ophthalmic imaging, conventional computed tomography (CT) and MR imaging scans are useful for the postoperative assessment of the eye and orbit. The consequences of these procedures can often be observed on diagnostic imaging through the presence of various implants and altered anatomy. The expected postoperative changes in the eye and orbit, the impact of implants on image quality and safety, and potential associated complications are reviewed in this article.
Imaging protocols
Computed Tomography
A suggested orbit CT protocol consists of 3-mm slice thickness soft tissue and 1-mm slice thickness bone window images with multiplanar reformats. Intravenous contrast is generally not necessary for assessing implant positioning or evaluating the altered bony anatomy, but is useful for cases of suspected tumor or infection. Implementation of metal artifact reduction software is useful for patients with implants that tend to produce streak artifact, as indicated in subsequent sections of this article.
MR Imaging
A typical MR imaging obit protocol consists of multiplanar T1-weighted and T2-weighted sequences with up to 3-mm slice thickness. As for CT, intravenous contrast can be administered with MR imaging scans particularly when tumor or infection is suspected and there are no contraindications. The use of fat-suppressed sequences is particularly useful for postcontrast T1-weighted sequences. Degradation of the fat-suppressed images by artifacts from some implants is mitigated using the Dixon method. For example, although surgically implanted metal devices are generally safe and compatible with MR imaging, selecting lower field strength scanners can also help minimize susceptibility artifacts.
Imaging findings
Eyelid Weight and Spring
Palpebral weights and springs are used to reanimate the eyelid to prevent corneal injury in patients with facial nerve paralysis. These devices are MR imaging safe and are encountered incidentally as part of the imaging work-up for recurrent tumors. The eyelid weights appear as slightly curved plates with holes for securing the implant and can produce substantial beam hardening artifact on CT ( Fig. 1 ). The eyelid springs do not produce substantial beam hardening on CT and consists of a prong secured to the superior orbital rim and another prong positioned in the upper eyelid ( Fig. 2 ).
Keratoprosthesis
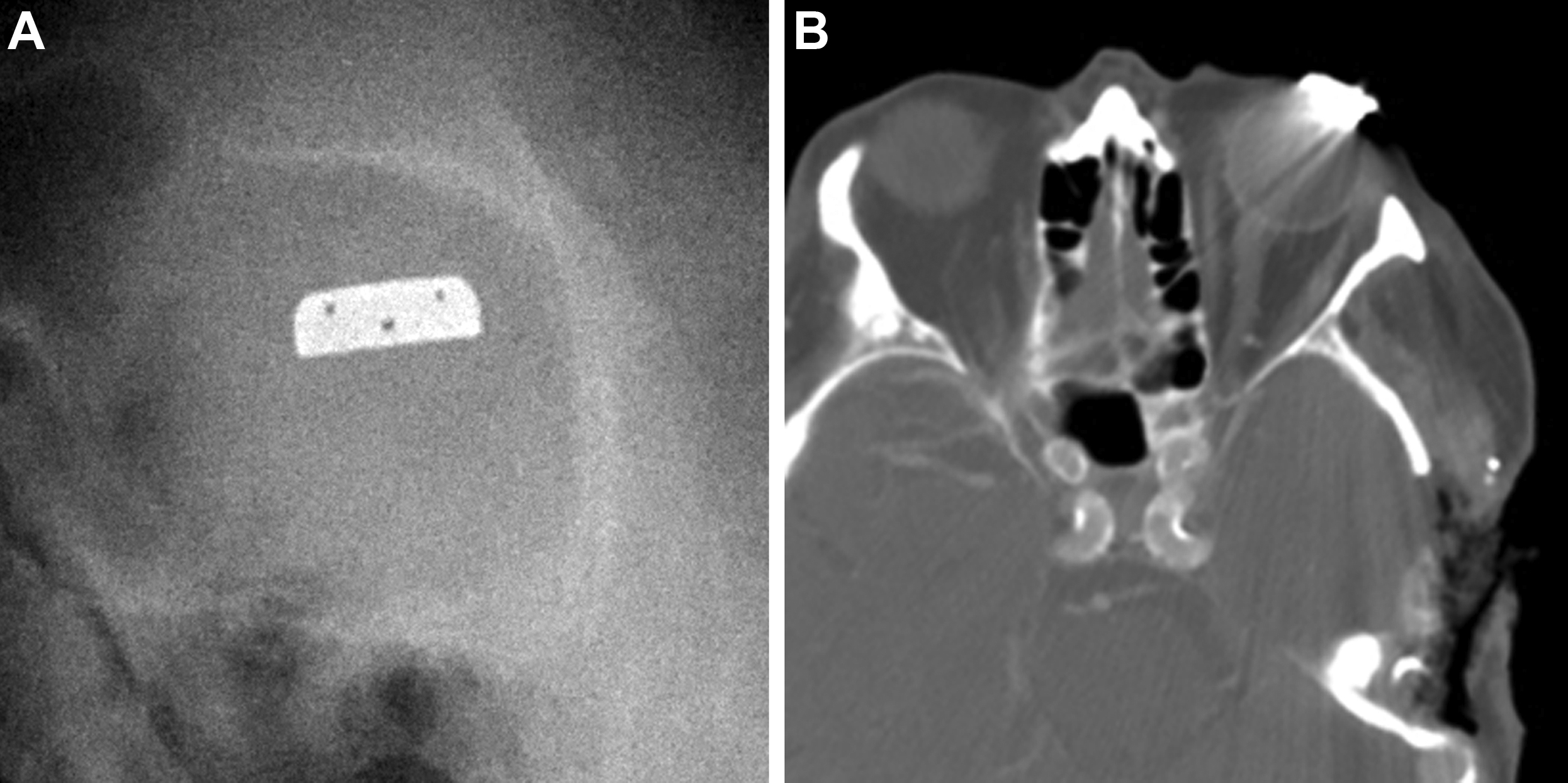
Alloplastic implants are used to treat cases of complicated corneal blindness. For example, Boston keratoprostheses are used in conjunction with corneal donor grafts. On CT, the keratoprosthesis plastic front plate that functions as a lens appears as soft tissue attenuation alongside the higher attenuation titanium locking back plate and locking ring ( Fig. 3 ). These prostheses are MR imaging compatible and do not produce any significant artifacts. An alternative option for corneal reconstruction is the osteo-odonto-keratoprosthesis, which comprises a portion of the tooth.
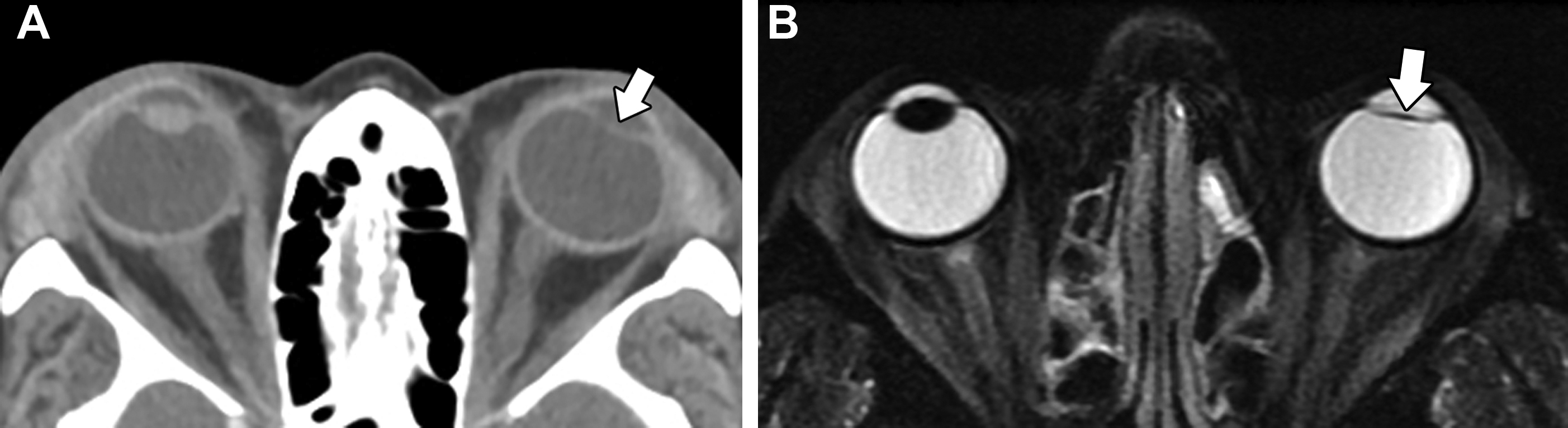
Intraocular Lens Implant
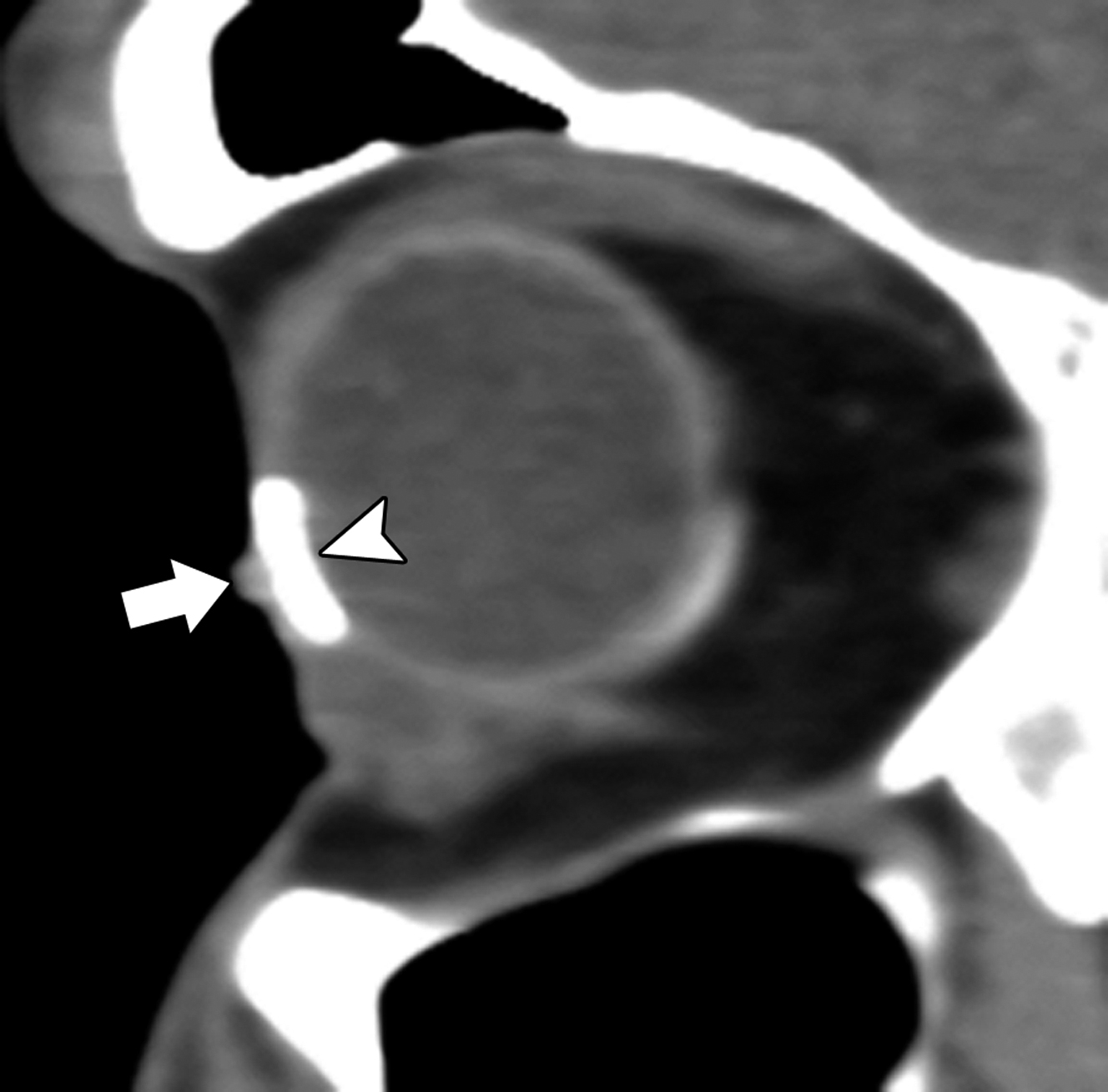
Artificial intraocular lens implants are used to substitute a diseased lens, most commonly from cataracts. The lens implants are comprised of a refractive optic component and haptics that secure the implant to the capsular bag. The optic portions of intraocular lens implants are generally visible on routine clinical CT and MR imaging scans, whereas the haptic portions are not discernible on clinical images. In particular, the implants appear as thin hyperattenuating structures on CT and low signal on T2-weighted MR imaging sequences ( Fig. 4 ). The implants are MR imaging compatible and do not produce any significant artifacts.
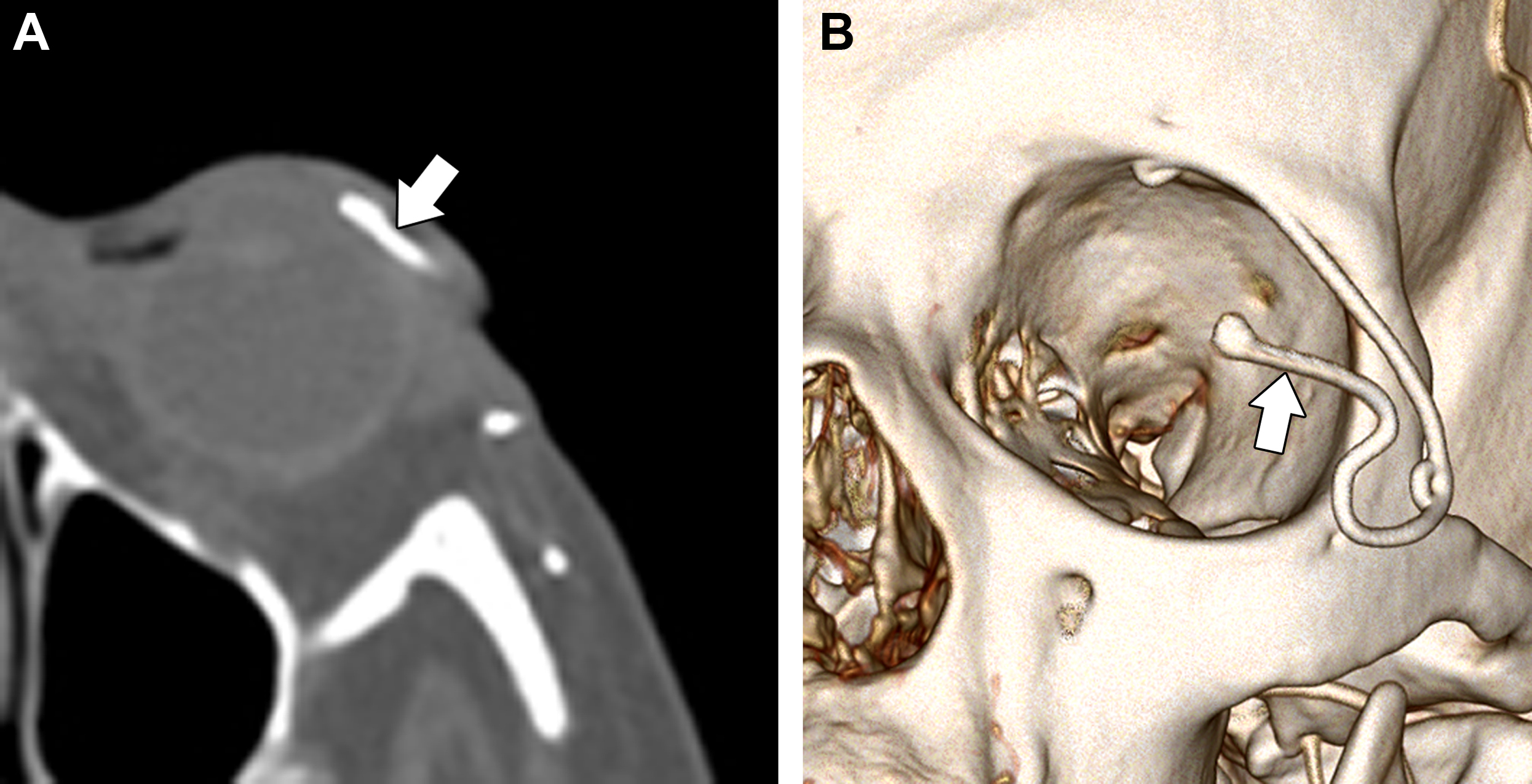
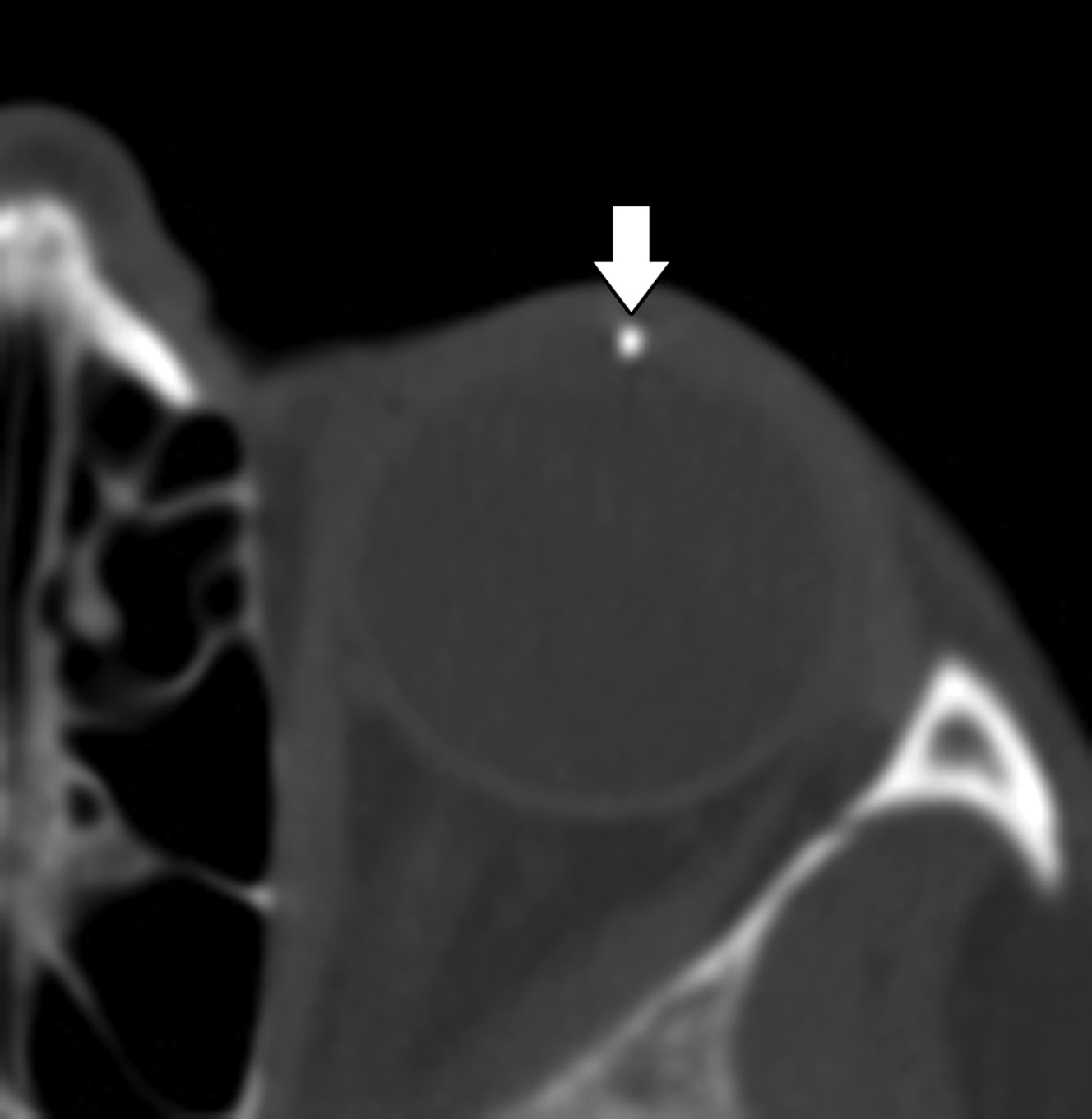
Glaucoma Drainage Implants
The excess intraocular pressure is reduced in patients with glaucoma using aqueous drainage devices, such as the Ahmed and Baerveldt shunts, among others. These devices are usually positioned along the superotemporal aspect of the globe and can accumulate variable amounts of fluid in the reservoirs, forming filtration blebs. The blebs are visible on imaging along the periphery of the implants ( Fig. 5 ). The size of the bleb correlates with the preoperative intraocular pressure and there is associated compression of the lacrimal gland. Alternatively, the stainless steel Ex-PRESS mini glaucoma filtration device is used to drain the aqueous humor. The device is positioned in the anterior chamber of the globe and is MR imaging compatible with negligible artifact on CT or MR imaging ( Fig. 6 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree