Evaluation of the postoperative temporal bone can be difficult given the complex anatomy of this region and the myriad surgical approaches for management of a variety of conditions. This article provides an understanding of common postsurgical changes of the temporal bone and their typical imaging appearances. Ultimately, greater radiologist knowledge of postoperative temporal bone imaging findings will help to serve patients and referring clinicians with prompt diagnosis and recognition of expected postintervention changes compared with postoperative complications and/or disease recurrence.
Key points
- •
Postoperative temporal bone image interpretation is challenging.
- •
Careful review of the patient’s clinical and operative history is critical to identify expected postoperative appearance versus complications.
- •
Common surgical procedures involving the temporal bone include tympanostomy, mastoidectomy, temporal bone resections, internal auditory canal and cerebellopontine angle surgical approaches, superior semicircular canal dehiscence repair, sigmoid sinus wall reconstruction, ossicular reconstruction, and auditory implant placement.
- •
Common interpretive pitfalls include lack of knowledge regarding expected postsurgical anatomic alterations, appearance of otologic hardware, correct hardware positioning, as well as delayed recognition of postoperative complications.
- •
Common postoperative temporal bone complications include postoperative hemorrhage, excessive pneumocephalus, brain retraction injury, vascular injury, cerebrospinal fluid leak, hardware malposition or migration, and bone or ossicular dehiscence.
Introduction
Postsurgical changes of the temporal bone can be difficult for radiologists to interpret accurately. The combination of inherently complex native temporal bone anatomy with unique, region-specific postoperative change makes evaluation of this region challenging. Consideration of the most common types of temporal bone surgical procedures and the expected postoperative appearance is critical when reviewing these studies, because it is this fundamental understanding of the expected postoperative appearance that serves as the foundation to discern postsurgical disorder such as disease recurrence and postoperative complications. Ultimately, prompt recognition of postintervention temporal bone disorder helps improve patient care and helps to show the added value of radiological interpretation to referring clinicians.
This article covers common temporal bone procedures, including tympanostomy, mastoidectomy, temporal bone resections, cerebellopontine angle (CPA) and internal auditory canal (IAC) approaches, superior semicircular canal dehiscence repair, sigmoid sinus wall reconstruction, ossicular reconstruction, and auditory implants. Several common postoperative complications are also covered. The discussion includes the specific clinical indications, as well as the unique surgical and imaging features, which help distinguish these procedures from one another.
Tympanostomy tube
Tympanostomy is a procedure in which a myringotomy (incision through the tympanic membrane) is made and a tube is placed through the myringotomy to maintain patency of the defect. Tympanostomy tubes are most commonly placed for chronic middle ear effusions and recurrent acute otitis media, but can also be placed for less common indications such as otitic barotrauma or patulous eustachian tube. Although tympanostomy tubes come in an assortment of sizes and shapes, they are most often seen as a tubular structure on thin-section high-resolution temporal bone computed tomography (CT) ( Fig. 1 ). CT can help identify the presence of a tympanostomy tube, although it may not be obtained for that purpose. It is important to recognize tympanostomy and for radiologists not to misinterpret the tube as a foreign body, displaced ossicle, or other potential component of otologic hardware. In some cases, the tympanostomy tube can be difficult to visualize on CT, particularly if the tube is plastic and/or obscured by overlying attenuating debris or fluid. , When tympanostomy tubes are displaced, they typically fall out into the ear canal on their own, but they can become displaced medially into the middle ear ( Fig. 2 ) and possibly result in conductive hearing loss, so a comment regarding tube position should be included in the imaging report. ,


Mastoidectomy
Mastoidectomy is a commonly performed temporal bone surgical procedure that varies in extent from cortical mastoidectomy to radical mastoidectomy. Although the most common indications for mastoidectomy include chronic otitis media and cholesteatoma, there are several additional potential indications, including coalescent mastoiditis, cochlear implantation, middle ear neoplasms, facial nerve exploration, and endolymphatic sac procedures. ,
Canal Wall Up Mastoidectomy
Canal wall up (CWU) mastoidectomy ( Fig. 3 ) involves removal of the lateral cortex of the mastoid bone as well as potentially all of the mastoid air cells extending from the borders of the tegmen mastoideum superiorly, to the sigmoid sinus posteriorly, and posterior wall of the external auditory canal anteriorly. The procedure preserves or leaves up the posterior wall of the external auditory canal. The extent of CWU mastoidectomy can vary from a cortical mastoidectomy, in which the Koerner septum is not traversed, to complete removal of all the mastoid air cells. Indications for CWU mastoidectomy include acute or chronic otitis media, mastoiditis, access for cochlear implantation, and access to the second genu and descending facial nerve segments. , , Typically, the resultant mastoidectomy bowl should be aerated on CT. The presence of soft tissue attenuation in the postoperative setting may indicate benign disorder, such as fibrosis/scarring, or may represent granulation tissue or recurrent cholesteatoma in the appropriate clinical setting. Mastoidectomy cavities may also be opacified because of surgical obliteration: historically, a variety of surgical materials have been used to fill the mastoidectomy bowl, including bone, fat, cartilage, or nonautogenous material such as hydroxyapatite. , In these cases, review of the operative history is critical in determining whether this material reflects disorder or expected postoperative change.

The facial recess approach can be performed as part of CWU mastoidectomy. As part of this procedure, bone lateral to the mastoid segment of the facial nerve and medial to the chorda tympani is removed to allow access to the middle ear cavity from the mastoid posteriorly. This procedure is also known as a posterior tympanotomy. This exposure is often used for cochlear implantation or for cholesteatoma resection, because the facial recess is often a site of disease recurrence. ,
Canal Wall Down Mastoidectomy
Canal wall down (CWD) mastoidectomy ( Fig. 4 ) involves removal of all the mastoid air cells and Koerner septum. In contrast with CWU mastoidectomy, CWD mastoidectomy also removes the posterior wall of the external auditory canal. There are several indications for which CWD mastoidectomy might be performed, including cholesteatoma that has already eroded the posterior canal wall, recurrent cholesteatoma, or for exteriorization/marsupialization of cholesteatoma matrix that cannot be fully resected. Examples of marsupialization of cholesteatoma matrix might be cholesteatoma eroding into the lateral semicircular canal or other portion of the membranous labyrinth (especially in an only hearing ear), or dehiscence of the dura with thin cholesteatoma matrix that cannot be removed without dural resection.

The resultant mastoid cavity communicates with the external auditory canal and is thereby externalized. As in CWU mastoidectomy, material within the mastoidectomy bowl following CWD mastoidectomy may represent granulation tissue, postoperative material, or recurrent disease; therefore, clinical and operative correlation in these cases is critical. , Cerumen and epithelial debris may also fill the mastoid cavity, leading to an opacified appearance on imaging. Although at times this may appear concerning, if the material is lateral to the epithelial lining of the cavity, it can be addressed merely with an ear cleaning. Cholesteatoma would only be considered recurrent if it were trapped medial to the cavity’s epithelial lining. CWD mastoidectomy can also be subdivided into modified radical and radical mastoidectomies.
Canal Wall Down Modified Radical and Radical Mastoidectomy
Radical mastoidectomy ( Fig. 5 ) is a subcategory of CWD mastoidectomy in which the middle ear cavity, in addition to the mastoid, is effectively externalized. A radical mastoidectomy involves removal of the tympanic membrane and the middle ear structures, including all the ossicles, without reconstruction. The eustachian tube and middle ear cavity remain exposed to the mastoidectomy defect. , Although currently infrequently performed, this procedure is typically reserved for very extensive middle ear disease processes, including unresectable cholesteatoma. , ,

Modified radical CWD mastoidectomy ( Fig. 6 ) refers to those procedures that fall short of radical mastoidectomy. , In this case, the tympanic membrane and ossicles are either left in situ (ie, in a Bondy-type mastoidectomy, performed when there is no cholesteatoma involvement of the middle ear), or, if needed, the tympanic membrane can be reconstructed, with grafting.

Temporal bone resection
Temporal bone resection is a broad term referring to several procedures that are typically performed for resection of malignant tumors involving the temporal bone. Lateral temporal bone resection (LTBR) ( Fig. 7 ) refers to en bloc resection of the bony ear canal, ear canal skin, tympanic membrane, and lateral ossicles (malleus and incus). In this procedure, CWU mastoidectomy with opening of the facial recess is performed. Bone removal is then extended along the superior aspect of the bony canal to the zygomatic root. Inferiorly, bone between the inferior aspect of the tympanic ring and the descending facial nerve is removed. The incudostapedial joint is separated, and the incus is removed. The tensor tympani tendon is incised. In addition, with either digital pressure on the canal or with osteotomes, the bone of the anterior tympanic ring is fractured to allow removal of the bony ear canal, tympanic membrane, and malleus en bloc. The procedure may be combined with parotidectomy and/or neck dissection, depending on tumor subtype and extent. If there is significant adjacent soft tissue removal, or anticipated need for adjuvant radiation, a temporalis muscle flap or a microvascular free flap may be used for reconstruction. In contrast with LTBR, sleeve resection refers to a less extensive procedure that involves removal of the skin of the ear canal up to or including the tympanic membrane. In modern times, this type of procedure is typically reserved for tumors that only involve the cartilaginous portion of the canal, or for in situ noninvasive disease because of lack of adequate control of the deep margin of neoplasms in this region and resultant high recurrence rates. ,

More extensive temporal bone resections for malignancy include subtotal and total temporal bone resections. Subtotal temporal bone resection (STBR) involves removal of elements of the external auditory canal, middle ear, bony labyrinth, and mastoid cavity. The procedure frequently begins with an LTBR, which is used to remove tumor in the ear canal and gain potential access to the middle ear, jugular foramen, and middle and posterior fossae with overall extent of bone removal tailored to tumor extent. Total temporal bone resection (TTBR) involves complete removal of the temporal bone with further extension of the STBR dissection medially to the petrous apex. As in STBR, overall extent of resection is tailored to tumor margins. Overall morbidity is greater with TTBR, with potential postoperative complications including stroke from carotid artery sacrifice (when required) as well as multiple lower cranial nerve palsies. Balloon test occlusion with neurointerventional radiology may be considered preoperatively when tumor is adjacent to or involving the carotid to determine the risk of ischemic stroke should the artery be violated. With the availability of adjuvant therapy (radiation, chemotherapy, immunotherapy), it is uncommon to intentionally sacrifice the internal carotid because of the morbidity risk. ,
With regard to temporal bone resections, CT and magnetic resonance (MR) imaging play important and complementary roles in preoperative evaluation of tumor extent, surgical planning, and surgical guidance, as well as in the postoperative evaluation of complications and for ongoing tumor surveillance.
Internal auditory canal and cerebellopontine angle approaches
There are 3 main surgical approaches to access the IAC and CPA: translabyrinthine, retrosigmoid, and middle cranial fossa (MCF). The most common disorders addressed via these approaches are vestibular schwannoma and meningioma.
Translabyrinthine Approach
The translabyrinthine approach ( Fig. 8 ) is used when hearing preservation is not a goal. The technique involves mastoidectomy, labyrinthectomy, and removal of the bone overlying the middle and posterior fossae, as well as overlying the IAC. Reconstruction commonly involves obliteration of the mastoid cavity with fat and sealing off of the aditus ad antrum and/or eustachian tube to prevent cerebrospinal fluid (CSF) leak. Advantages of this approach include the avoidance of significant retraction on the cerebellum or temporal lobe, as occurs with other approaches, and ease of exposure of the fundus of the IAC. In addition, if the facial nerve requires grafting, it is already well exposed. Disadvantages include loss of hearing and a higher rate of CSF leak. ,

Retrosigmoid Approach
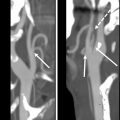
A retrosigmoid approach ( Fig. 9 ) involves a suboccipital craniotomy. Access to the IAC is afforded via drilling of the overlying bone from its posterior aspect. Because this technique does not require violation of the labyrinth, it is a hearing-preservation approach if the cochlear nerve can be preserved. Disadvantages include a more limited view of the fundus, the need for cerebellar retraction, and higher rates of postoperative headache if drilling is required, because drilling is performed intradurally (as opposed to extradurally in a translabyrinthine approach). ,


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree