This article discusses the 4 main imaging modalities used to evaluate reproductive-aged women: ultrasound, magnetic resonance imaging, computed tomography, and fluoroscopy. For each modality, major clinical indications are described, along with important technical considerations unique to imaging reproductive-aged women. Finally, key safety issues are discussed, particularly with regard to imaging pregnant patients.
Key points
- •
Ultrasound (US), magnetic resonance imaging (MR imaging), computed tomography (CT), and fluoroscopy (hysterosalpingography) are all important imaging tools for evaluating reproductive-aged women.
- •
US typically is the initial study of choice, followed by MR imaging for problem solving.
- •
CT is useful for nonlocalized symptoms or in situations, such as trauma, where rapid, comprehensive evaluation of the abdomen and pelvis is required.
- •
Fluoroscopy, in the form of hysterosalpingography, has important specialized applications.
- •
Because MR imaging and US do not use ionizing radiation, they generally are considered safer than CT. Important safety considerations remain, however, particularly when imaging pregnant patients.
Introduction
Imaging women who are reproductive age is challenging. The uterus and ovaries are deep within the pelvis; their positions and orientations are highly variable. In addition, the appearance of these organs may vary depending on several factors, including patient age and stage of menstrual cycle. Relatively rare pathologic entities must be distinguished from common benign findings and normal variants. It also is necessary to minimize the use of ionizing radiation. Finally, there are unique safety considerations when imaging pregnant patients.
The most common tools that are used to image reproductive-aged women are ultrasound (US) and magnetic resonance imaging (MR imaging). Both of these tools offer excellent anatomic detail and soft tissue contrast without exposure to ionizing radiation. US generally is used for initial evaluation whereas MR imaging typically is used for problem solving when US is either indeterminant or discordant with the overall clinical picture. Computed tomography (CT) is used principally in the setting of acute pain or other situation where full abdominal and pelvic coverage is required (cancer staging, for example). The use of CT is limited, however, because it involves ionizing radiation and also because it has relatively poor soft tissue contrast in the ovaries and uterus. Finally, fluoroscopy—in the form of hysterosalpingography (HSG)—has a specialized role in evaluating the patency of the fallopian tubes.
This article describes the general approach to using each of these modalities, along with important technical considerations as well as safety issues unique to imaging women who are reproductive age. Specific diseases as well as specialized techniques are described in later articles. This article focuses on general approaches that can be used to improve image quality and maximize diagnostic information.
Ultrasound
US typically is the initial study of choice when imaging women who are reproductive age. , It is relatively inexpensive with excellent spatial resolution and soft tissue contrast. In many cases, blood flow detected on Doppler imaging is helpful for diagnosis, including vascular tumors, polyps, retained products of conception, vascular anomalies, and ovarian torsion. Because US avoids the use of ionizing radiation, it generally is safe and lends itself to performing serial follow-ups and surveillance.
Ultrasound Imaging Approach
The detailed US scanning protocol is based on the exact clinical indication. Typically, both transabdominal and transvaginal images are obtained. Transabdominal images are obtained using a full urinary bladder as the acoustic window, whereas transvaginal images are obtained with the bladder empty. Although transvaginal images may have higher resolution for structures close to the US probe, transabdominal images are key for detecting extrauterine abnormalities, abdominal fluid, and hydronephrosis. When the uterus is enlarged or ovaries are superior in position, they are seen better transabdominally than transvaginally.
Measurements
Measurements of anatomic structures and masses are made along 3 axes—longitudinal, transverse, and anteroposterior—relative to the structure being imaged. Imaging relative to these axes can be challenging if the uterus has an oblique orientation or is retroverted. Color and spectral Doppler imaging is essential to detect and characterize blood flow. For example, a central vascular stalk is a helpful feature for diagnosing endometrial polyps. It is important that proper Doppler technique is used, adjusting scale, gain, and angle.
Three-dimensional reconstructions
Three-dimensional (3-D) reconstructions can be useful for many applications, including assessing the uterine contour in suspected uterine anomalies and establishing the location of intrauterine devices.
Stage of menstrual cycle
With pelvic US, patient age and phase in menstrual cycle are crucial, because the endometrium and ovaries can appear different throughout a patient’s life. For detecting endometrial abnormalities, the early proliferative phase (immediately after menses) is the best timeframe; the endometrium is thinnest during this phase. Ovaries in a reproductive-aged woman also can undergo changes related to ovulation.
Ultrasound Safety
Heating
Because US relies on sound waves and avoids ionizing radiation, it generally is considered safe compared with alternative techniques, such as CT. No harmful effects from US have been described in humans. Based primarily on animal studies, however, there are theoretic risks from tissue heating, particularly in early gestation. With this in mind, a prudent approach is to (1) perform US only when it is medically indicated and (2) minimize the use of techniques associated with high-power deposition, such as power Doppler, early in pregnancy.
Infection
Because US probes come in close contact with skin and mucosal surfaces, there is a risk of spreading infection between patients. When probe covers are used together with disinfectant wipes (low-level disinfection), persistent microbial DNA can be found on transvaginal probes. Therefore, a meticulous cleaning program is recommended, including the use of transducer covers and high-level disinfection of transvaginal transducers and handles. ,
Computed tomography
CT provides reliable and comprehensive evaluation of the abdomen and pelvis in a short scan time and is used frequently for the assessment of acute symptoms. Because CT requires radiation exposure and lacks the soft tissue contrast of MR imaging and US, it often is not the initial study of choice in evaluating reproductive-aged women. CT is useful in the evaluation of abdominal pain when initial US is negative or equivocal. It also is useful in situations, such as cancer staging, where comprehensive evaluation of the entire abdomen and pelvis is necessary. Finally, CT is used in situations, such as major abdominal trauma, where rapid evaluation is critical and techniques, such as US, are less sensitive, particularly for parenchymal injury.
Computed Tomography Technique
CT in reproductive-aged women is performed using an approach similar to that used for other patients. Intravenous contrast generally is useful unless contraindicated. As with any patient, radiation exposure should be minimized by eliminating unnecessary contrast phases, restricting the anatomic scan coverage, and using dose-reduction techniques, such as tube current modulation and iterative reconstructions.
Computed Tomography Safety
CT has two major risks. First, there is risk from contrast administration, which in younger patients is predominantly allergy or allergy-like reactions. There also is a risk from ionizing radiation exposure. Although the exact radiation risk from radiation in medical procedures is complex, younger patients likely are more sensitive to the effects of radiation. Therefore, nonradiation alternatives, such as US and MR imaging, are preferentially used in younger patients when possible, particularly when serial examinations are needed. That said, concerns of radiation exposure should not prevent a patient from undergoing a CT examination when medically necessary.
Because of potential risks to the developing embryo or fetus, special considerations are required for using CT in pregnant patients. First, before using techniques that require x-ray exposure to the pelvis, pregnancy status should be confirmed, either through history or urine/blood testing. Radiation doses less than 50 mGy convey a negligible risk for miscarriage, malignancy, or major malformation. Most radiological examinations, including single-phase CT examinations, are within this level. Caution should still be exercised, however, especially when multiple CT scans are required, including consultation with a medical physicist to verify dose. Informed consent in these cases should be considered.
Magnetic resonance imaging
MR imaging of the female pelvis is central to the clinical evaluation of both benign and malignant diseases. , In patients with endometrial and cervical cancers, the superior soft tissue contrast achieved by MR imaging allows for highly accurate assessment of local tumor extension as well as metastatic disease. In terms of benign disease, MR imaging is a key tool in preoperative planning for treatment of leiomyomas and assessing müllerian duct anomalies. , Chemical sensitivity inherent in the MR imaging scan permits the identification of fat-containing masses, such as teratomas. Increasingly, functional techniques, such as diffusion-weighted imaging (DWI) , and dynamic contrast imaging, are permitting new insights into tumor biology. ,
Pelvis Magnetic Resonance Imaging Pulse Sequences and Imaging Approach
Broadly speaking, at the authors’ institution, MR imaging of the female pelvis contains 3 types of pulse sequences that are tailored to the application at hand. Pelvic MR imaging is performed using both 1.5T and 3.0T scanners. In all cases, a dedicated phased array coil is placed directly over the anatomy of interest in order to maximize sensitivity. In addition to general imaging sequences, described in this article, specialized pulses sequences and image planes may be obtained for certain applications (for example, in suspected pelvic malignancies, uterine anomalies, or abnormally invasive placenta). Those specialized approaches are discussed in other articles within this issue.
High-resolution T2-weighted imaging
The most important imaging sequence for evaluating the female pelvis is the T2-weighted fast spin-echo (FSE) without fat saturation. Images have excellent tissue contrast and spatial resolution. Ovaries and uterus are well seen, along with clear delineation of important fascial planes.
Diffusion-weighted imaging
In DWI, strong magnetic field gradients are used to generate image contrast that is proportional to the amount of freedom water molecules have to move within tissues. In general, pelvic malignancies tend to be more cellular and, therefore, have higher DWI signal (and lower apparent diffusion coefficient). Low apparent diffusion coefficient can be seen, however, in both benign tumors and non-neoplastic processes, such as hemorrhage and infection. DWI can aid in the detection of lymph nodes and peritoneal metastases.
Chemical shift imaging
T1-weighted images are obtained with fat and water in-phase and opposed-phase. Signal dropout on opposed-phase images establishes the presence of fat that is smaller than the image voxel (eg microscopic fat). Black lines, or india ink, at the interface between structures establishes the presence of bulk fat.
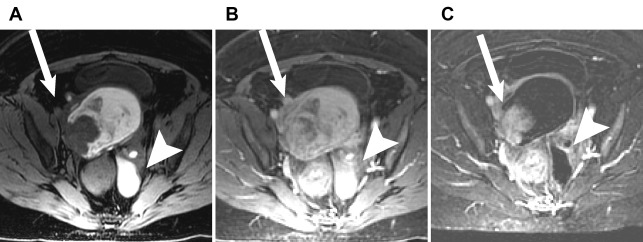
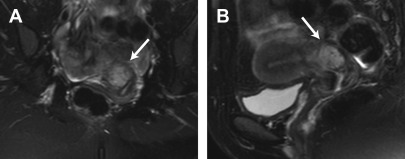
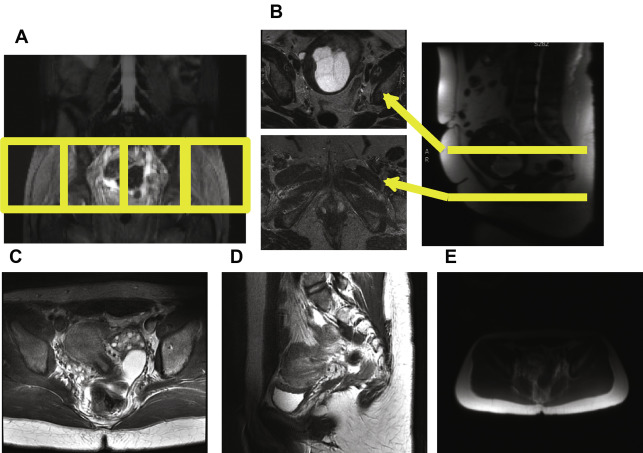
Contrast enhancement
T1-spoiled gradient-echo sequences with fat saturation are obtained before and after administration of a gadolinium-based contrast agent (GBCA). Lesion enhancement may establish the presence of suspicious solid nodules. High T1 signal in a cystic lesion before the administration of intravenous contrast can indicate the presence of blood products in either an endometrioma or hemorrhagic cyst. Because these lesions have high T1 signal prior to administration of contrast, subtraction images may be useful in detecting enhancing nodules against an already bright background ( Fig. 1 ).
Magnetic Resonance Imaging Technique
This section addresses several common technical challenges that are encountered when performing MR imaging of the female pelvis.
T2-weighted images and fat suppression
When imaging the female pelvis with MR imaging, T2-weighted images performed without fat suppression are crucial. Fat within the pelvis allows clear delineation of fascial planes and anatomic boundaries, which are important for judging (among other things) the local extent of tumors. When fat suppression is used, high signal intensity within pelvic vessels as well as fluid in the pelvis can obscure these anatomic planes ( Fig. 2 ).
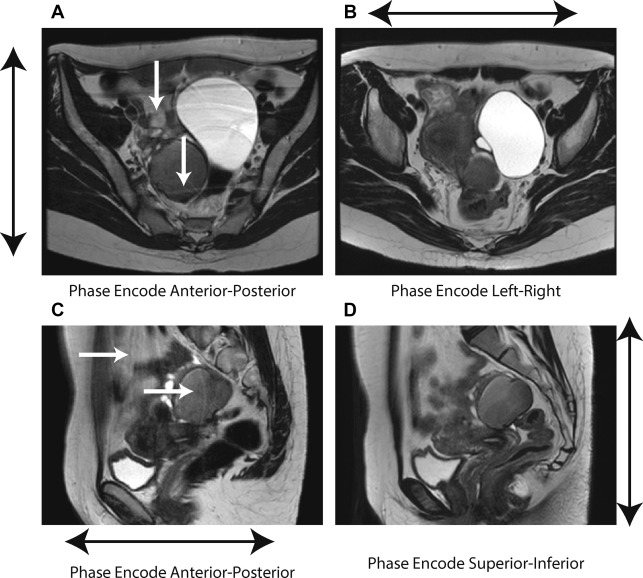
Phase encoding direction
Unlike imaging in the abdomen, MR imaging of the female pelvis typically is performed while the patient breathes freely. This is possible because the deep pelvic organs, such as the uterus and ovary, tend to be fairly static. Considerable artifact may be generated, however, from motion of the anterior abdominal wall. When the phase encoding direction is chosen anterior-posterior (which is the direction used in the pelvis), these motion artifacts potentially obscure anatomic details within the uterus. Changing the phase encoding direction to left-right, however, these artifacts are pushed to the side in a more benign pattern ( Fig. 3 ).
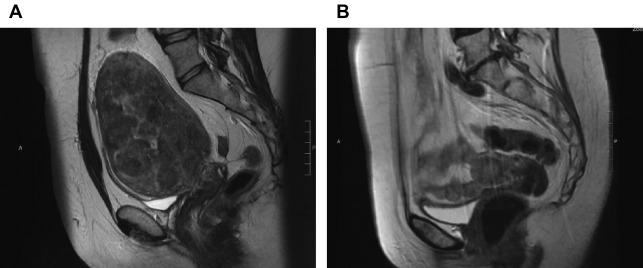
Choosing the field of view
The imaging field of view (FOV) must be chosen to match the anatomy being imaged. Many times, the FOV is made overly large in order to avoid missing things, but a large FOV leads to larger pixel sizes and coarser spatial resolution, which may make important structures, such as the uterus, difficult to evaluate. Because the uterus in particular can vary in size from one woman to another, depending on age, pregnancy, and the presence of masses, it is difficult to use a one-size-fits-all approach. Instead, the FOV can be adjusted at the time of the scan ( Fig. 4 ).
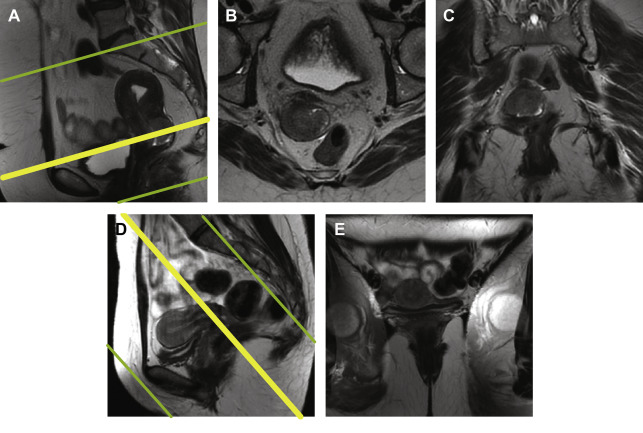
Tailored image planes
MR imaging acquisitions in the female pelvis usually are tailored to answer specific questions, for example, assessing the depth of invasion of an endometrial mass or parametrial extension of a cervical tumor ( Fig. 5 ). Making these choices correctly requires careful communication between radiologists and technologists and requires both parties to speak a common language and understand the physical principles involved.
Coil array positioning
Most pelvic MR imagings are acquired using an array of radiofrequency (RF) surface coils. These coil arrays are composed of 8 to 32 detector coils placed over the part of the body that is being imaged ( Fig. 6 A). Coil arrays have increased sensitivity for objects close to the coil elements, and they experience decreased noise from regions that are not being imaged. In addition, coil arrays permit the use of parallel imaging techniques that can speed up the acquisition.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree