ppropriate use of imaging techniques is essential for diagnosis, treatment planning, and follow-up of orthopaedic procedures. Basic techniques will be discussed in this chapter to avoid redundancy in anatomic chapters.
ppropriate use of imaging techniques is essential for diagnosis, treatment planning, and follow-up of orthopaedic procedures. Basic techniques will be discussed in this chapter to avoid redundancy in anatomic chapters.
 Routine Radiographs
Routine Radiographs
Routine radiographs remain the primary screening examination for musculoskeletal disorders. Appropriate evaluation of radio-graphs may provide the diagnosis or allow selection of the next imaging procedure to completely evaluate the clinical problem. Specifically, radiographs are essential for proper interpretation of magnetic resonance (MR) images.
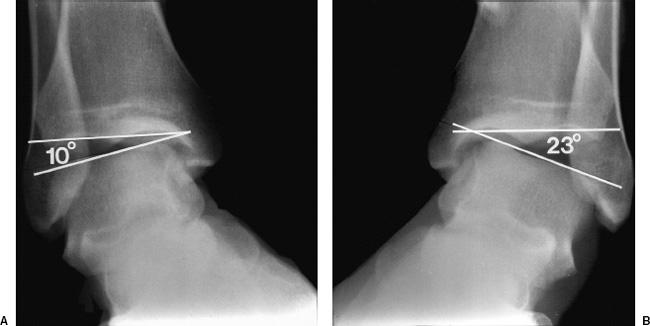
Currently, screen-film radiography is being replaced with computed radiography (CR) at many institutions. Regardless of the system used, it is essential to ensure proper patient positioning and accurate chronologic labeling of images. Multiple views (two to four) are required to evaluate osseous and articular anatomy. Specific views will be discussed in subsequent anatomic chapters. In certain cases, fluoroscopically positioned images are useful to optimize positioning and reduce bony overlap. This approach is useful in the foot and wrist. The technique is also appropriate to evaluate interfaces of arthroplasty components, fixation devices, and evaluate pin tracts when infection is suspected clinically. Fluoroscopic positioning is also useful when performing stress tests to assure that the joint is properly positioned. Stress studies are most often performed on the ankle, elbow, knee, and wrist (see Fig. 1-1).
 SUGGESTED READING
SUGGESTED READING
Bender CE, Berquist TH, Stears JG, et al. Diagnostic techniques. In: Berquist TH, ed. Imaging of orthopaedic trauma, 2nd ed. New York: Raven Press; 1992:1–37.
Bontrager KL. Textbook of radiographic positioning and related anatomy, 5th ed. Mosby: St. Louis; 2001.
 Computed Tomography
Computed Tomography
Computed tomography (CT) is a fast and efficacious technique for evaluating musculoskeletal disorders. New systems are even faster which allows more flexibility for reconstruction in multiple image planes. There are also improved techniques for evaluating patients with orthopaedic fixation devices or joint replacements. The basic components of a CT scanner include a gantry that houses the detectors and a movable patient table. Common CT terminology is summarized as follows:
Multislice: Number of images generated
Multidetector: Number of detector rows to register data
Multichannel: Ability to register data during gantry rotation using a data acquisition system, typically 16 channels
Detector array: Multichannel CT systems have a slip-ring design system that allows electronic manipulation of the x-ray beam into multiple channels of data
Beam collimation: Metal collimators near the x-ray source are adjusted to control the width of the beam directed to the patient
Section collimation: Smallest section thickness that can be reconstructed from the acquired data and is based on how detectors are configured to channel the data
Effective section thickness: Related to beam collimation for single channel CT or width of the detector row for multichannel CT
Pitch: Table translation in millimeters per gantry rotation divided by beam collimation
CT is particularly suited for evaluating complex skeletal anatomy in the spine, shoulder, pelvis, foot, ankle, hand, and wrist. Thin-section images allow reformatting in multiple image planes and three-dimensional reconstruction. Pre- and postcontrast images (intravenous iodinated contrast) are useful for evaluation of soft tissue lesions. Imaging of patients with orthopaedic implants requires special attention to detail to minimize metal artifacts.
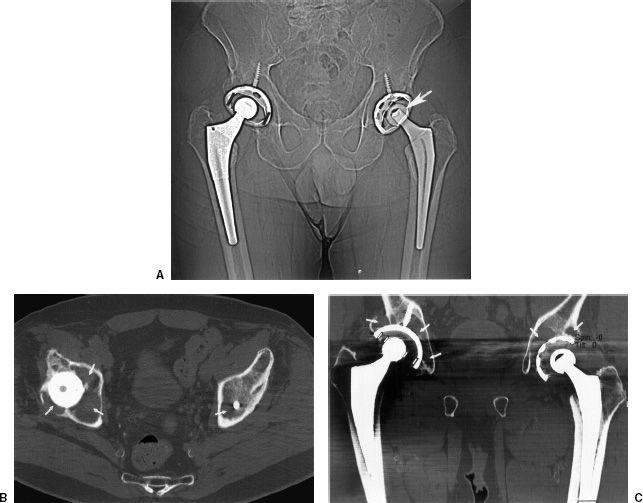
Metal-related artifacts can cause significant image degradation in patients with orthopaedic implants. Certain metals are more problematic. Implants with lower beam attenuation coefficients such as titanium produce fewer artifacts than stainless steel and cobalt-chromium implants. Artifact reduction can be accomplished by modifying parameters such as milliampere-seconds, kilovolt peak (kVp), and reconstruction algorithms. Higher kilovolt peak increases metal penetration. Several authors recommend using 140 kVp. Increasing the tube current may also reduce metal artifacts. Multichannel scanners can collect redundant data by using a lower pitch setting. This also reduces metal artifact (see Fig. 1-2).
 Fig. 1-1 Stress views of the ankle done with valgus positioning of the normal (A) and involved ankle (B) for comparison. The tibiotalar angle on the abnormal side (B) opens 13 degrees more than the normal side indicating tears of the anterior talofibular and calcaneofibular ligaments (>5 degrees indicates one ligament is disrupted and >10 degrees indicates both ligaments are disrupted).
Fig. 1-1 Stress views of the ankle done with valgus positioning of the normal (A) and involved ankle (B) for comparison. The tibiotalar angle on the abnormal side (B) opens 13 degrees more than the normal side indicating tears of the anterior talofibular and calcaneofibular ligaments (>5 degrees indicates one ligament is disrupted and >10 degrees indicates both ligaments are disrupted).
SUGGESTED READING
Berland LL, Smith KL. Multidetector array CT. Once again technology creates new opportunities. Radiology. 1998;209: 327–329.
Douglas-Akinwande AC, Buckwalter KA, Rydberg J, et al. Multichannel CT: Evaluating the spine in postoperative patients with orthopaedic hardware. Radiographics. 2006;26: S97–S110.
Memarsadeghi M, Breitenseher MJ, Schaefer-Prokop C, et al. Occult scaphoid fractures: Comparison of multidetector CT and MR imaging-initial experience. Radiology. 2006;240: 169–176.
Ohashi K, El-Khoury GY, Bennett DL, et al. Orthopaedic hardware complications diagnosed with multidetector row CT. Radiology. 2005;237:570–577.
 Magnetic Resonance Imaging
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is a proven technique with expanding musculoskeletal applications. Most imaging is performed at 1.5 Tesla (T). However, 3 T units are being used with increasing frequency. There are also multiple open bore and extremity configurations at lower field strengths for musculoskeletal imaging.
Before considering MRI as an imaging option one must consider certain patient screening and safety issues. A written questionnaire is preferred with specific, easy to answer questions to improve detection of patients who may be at risk during MRI examinations. Information regarding obvious risk factors such as cardiac pacemakers, certain cerebral aneurysm clips, metallic foreign bodies, and electrical devices can be obtained from the questionnaire and/or by verbal clarification with the patient. When metallic foreign bodies are suspected, radiographs or CT should be obtained for confirmation.
Metallic implants may create artifacts that significantly degrade image quality, especially if they contain ferromagnetic impurities. Fortunately, most orthopaedic implants are made of alloys that do not contain ferromagnetic material. The size of the implant and its configuration may still cause problems. Image quality can be improved in several ways. Increasing the bandwidth and number of acquisitions decreases metal artifact. One can also set the frequency encoding direction along the axis of the metal. Unfortunately, this is not always possible. T1-weighted, fast spin-echo (SE) and fast short T1 inversion recovery (STIR) sequences may be useful to improve image quality (see Fig. 1-3). Gradient echo sequences should be avoided. Metal artifact is also less of an issue at lower field strengths. Cast material and methyl methacrylate do not cause artifacts.
 Fig. 1-2 A: Computed tomographic (CT) scout image demonstrating bilateral hip arthroplasties with metal and polyethylene components on the right and a modular ceramic head (arrow) on the left. There is slight asymmetry of the femoral heads noted by black lines on the right. Axial (B) and coronal (C) CT images with artifact reduction techniques clearly demonstrate the bilateral osteolysis (arrows) and femoral head asymmetry (lines).
Fig. 1-2 A: Computed tomographic (CT) scout image demonstrating bilateral hip arthroplasties with metal and polyethylene components on the right and a modular ceramic head (arrow) on the left. There is slight asymmetry of the femoral heads noted by black lines on the right. Axial (B) and coronal (C) CT images with artifact reduction techniques clearly demonstrate the bilateral osteolysis (arrows) and femoral head asymmetry (lines).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree