Thomas Van Thielen, Luc van den Hauwe, Johan W. Van Goethem, Paul M. Parizel
Imaging Techniques and Anatomy
Anatomy
Anatomically the spine is organised segmentally, consisting of 7 cervical, 12 thoracic, 5 lumbar, 5 (fused) sacral and 3–5 coccygeal vertebra. Each level, except C1, consists out of the following elements: a vertebral body (corpus vertebrae) anteriorly and a vertebral or neural arch (arcus posterior) posteriorly. Together these two structures enclose the spinal canal.
Functionally the spine can be divided in three so-called columns.1 The anterior column includes the anterior longitudinal ligament, the anterior annulus fibrosus and the anterior two-thirds of the vertebral body. The middle column comprises the posterior third of the vertebral body, the posterior annulus fibrosus and the posterior longitudinal ligament. The posterior column includes the posterior elements with the pedicles, facet joints, laminae and spinous processes as well as the posterior ligaments.
Osseous Elements
Vertebral Body
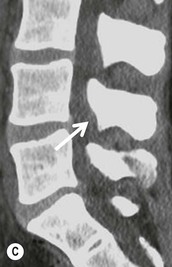
The vertebral bodies have a thin rim of cortical bone and a central framework of mostly vertically orientated trabeculae. This osseous portion contains stores of phosphate and calcium and has a structural support function. Sclerotic bands can be seen in the vertebral body at the site of fusion between two vertebral components. This is typically seen at the neurocentral junction and in the dens axis. In the dens axis there may be remnants of the subdental synchondrosis. These bony structures are optimally evaluated with computed tomography (CT) imaging and to a lesser extent with magnetic resonance imaging (MRI). On CT imaging vascular channels are often visible and in a post-traumatic setting can be mistaken for small fractures.
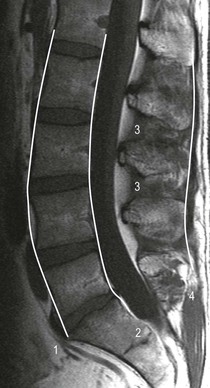
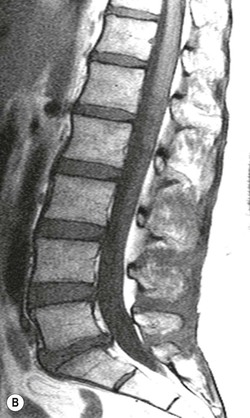
The centre of the vertebral body is composed of red bone marrow, which is haematopoietically active. Red and yellow bone marrow are not entirely homogeneous and each contain elements of the other. The vertebral marrow is dynamic, changing with age, immune state, oxygenation, coagulation and structural needs.2 The normal adult distribution of bone marrow is reached by the age of 25. With ageing, the bone marrow assumes a more variable appearance with a reduction in the red cell mass and trabecular bone and increase of the fatty content. These changes appear relatively late in comparison to the changes in the bone marrow in the peripheral skeleton. The distribution of the red bone marrow in a vertebral body is predominantly seen at the metaphyseal equivalents near the endplates and the anterior part of the vertebra.3 Evaluation of the bone marrow is best done with MRI. In the normal spinal marrow the distribution patterns of fatty and red marrow were categorised into four patterns by Ricci and colleagues4 (Fig. 54-1). Pattern 1 describes a uniform low signal on T1–weighted images with high linear signal around the basivertebral vein; this type is most commonly seen in younger patients aged 30 or less. Type 2 is a band-like high T1 signal limited to the periphery of the vertebral body. Type 3 is characterised by multiple small indistinct (difficult to visualise) high signal intensity foci on T1-weighted images throughout the vertebral body. These two patterns (types 2 and 3) are seen with increasing age and typically in persons of 40 years and older. Type 4 is a more severe form of type 3 with multiple larger high signal intensity foci (5–15 mm) on T1 images throughout the vertebral body.


Neural Arch
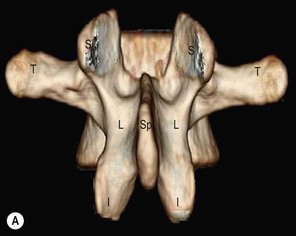
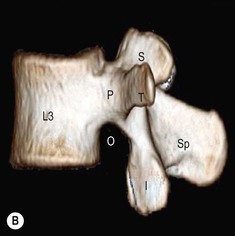
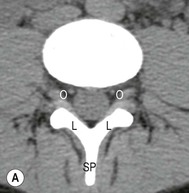
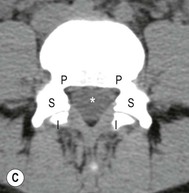
The neural arch, also known as posterior arch, forms the bony lateral and posterior border of the spinal canal (Figs. 54-2–54-4). It can be divided into different segments. Between the transverse and spinous process the neural arch is called the lamina. The pedicle is the part situated between the transverse process and the vertebral body. The pedicle of each vertebra is notched at its inferior and superior edge. Together these notches form an opening called the intervertebral foramen. Through this foramen the spinal nerves exit the spinal canal.
Spinous and Transverse Processes
The spinous process is attached to the most posterior part of the neural arch. The transverse processes arise from the lateral edge of each neural arch (Figs. 54-2–54-4). The spinous as well as the transverse process serve as an important site of attachment for the deep back muscles. As described above, they also divide the neural arch into different anatomical parts.
Joints
Facet Joints
The facet joints or the zygapophyseal joints are diarthrodial synovial joints between the inferior and superior articular processes of adjacent neural arches. These articular processes arise from the articular pillars including the bone at the junction between pedicles and the laminae. The superior articular process is located relative anterior to the inferior articular process and faces posteriorly (Figs. 54-2–54-4). In the lumbar spine the joint surface is located in an oblique way at an angle of about 45° between the sagittal and coronal plane. In the thoracic spine the facet joints are almost orientated in the coronal plan.5
The inferior facets have a convex shape while the superior articular surface has a concave aspect. In a non-degenerative spine the joint surface is covered with hyaline cartilage, being the thickest in the centre of the joint. In the normal anatomy, as most other joints, the surface of the joints should be smooth and regular with an equal spacing between the two joint surfaces. The distance between the articular processes at the facet joint should be between 2 and 4 mm on plain radiography.6
On the posterolateral side, the facet joint is covered with a strong fibrous capsule which is composed of several layers of fibrous tissue and a synovial membrane. On the anterior side of the joint, there is no fibrous capsule. Here, the only border between the spinal canal and the facet joint is formed by the ligamentum flavum and the synovial membrane.7 The capsule is composed of a superior and inferior recess containing fat pads. These fat pads act as movement-compensating mechanisms and as a lubrication mechanism for the facet joint as they are partially covered with synovial tissue.5
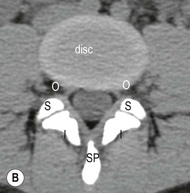
Intervertebral Disc—Symphysis
The intervertebral disc consists of the inner nucleus pulposus surrounded by an outer layer, the annulus fibrosus. Embryologically the nucleus pulposus is formed from cells originating from the notochord; in humans these notochordial cells are lost and replaced by chondrocyte-like cells. The nucleus pulposus is macroscopically composed of soft, elastic tissue with a yellow colour.8 The nucleus pulposus is primarily composed of water, proteoglycans and loose collagen fibres. With normal ageing the water content decreases.
The outer annulus fibrosus is composed of multiple concentric layers of fibrocartilage tissue. The outer layers, also called Sharpey’s fibres, continue in the longitudinal ligament and the vertebral bodies. The fibres of each layer are directed in an oblique way (30° angle), forming a meshwork. In this way a very strong flexible structure is formed.
Ligaments
Longitudinal Ligaments
A longitudinal ligament is present at the anterior and posterior part of the vertebral bodies running along the entire spine, providing stability (Fig. 54-5). The anterior longitudinal ligament (ALL) is a thick ligament which is slightly thinner at the level of the vertebral bodies and wider at the intervertebral disc.
The posterior longitudinal ligament (PLL) is situated in the vertebral canal and runs from the dens axis (tectorial membrane) to the sacrum. It is thicker in the thoracic spine and wider in the cervical region compared to the lumbar level. At the level of the vertebral bodies the PLL is separated from the concave posterior wall of the vertebral bodies by the anterior epidural space. This space contains epidural fat, basivertebral veins and the anterior internal vertebral veins.
Ligamentum Flavum
The ligamentum flavum or yellow ligament is a paired structure connecting the spinal laminae forming the posterior wall of the spinal canal (Fig. 54-6). At the lateral side these structures fuse with the capsule of the facet joints, forming a boundary of the intervertebral neuroforamina.9 The boundary between the two ligamenta flava in the centre is indistinguishable on imaging. The ligamenta flava provide a static elastic force to stimulate the return to a neutral position after flexion or extension. They also limit the flexion motion of the spine and help maintain a smooth posterior lining of the central spinal canal.10
Interconnecting Ligaments
The posterior elements are heavily reinforced with different ligaments connecting two adjacent vertebra. The supraspinous ligament connects the tips from the spinous processes while the interspinous ligaments connect the base of the adjacent spinous processes (Fig. 54-5). The transverse processes are connected by the intertransverse ligaments. As discussed earlier the laminae of the adjacent vertebra are bound together by the ligamentum flavum.
Neural Structures—Spinal Cord, Spinal Nerves, Dura Mater
The shape of the spinal canal varies from oval on the cervical and thoracic level to a triangular shape at the lower lumbar region.11
Anteriorly the dura mater is in contact with the posterior longitudinal ligament almost over the length of the whole spine. Laterally the dura mater is in close contact with the medial border of the pedicles. Above and below the pedicles the dura mater is in contact with the epidural fat in continuity with the intervertebral foramina. Posteriorly the dura mater is in contact with the posterior epidural fat separating the dura from the ligamenta flava, the posterior joints and the laminae.
In the kyphotic thoracic regions, the dura can be separated from the posterior elements by a layer of epidural fat of up to 5 mm thick. This fat should not be mistaken for epidural lipomatosis.
The spinal cord and its normal internal structure (grey and white matter) are best evaluated with MR imaging (T2). It consists of a central butterfly-shaped part which is the grey matter. The measurements of the spinal cord show a wide variation according to the patient.
The conus medullaris is the terminal end of the spinal cord and is in normal anatomy found at the level L1–L2. The spinal cord tapers out into a cone at this level and the nerve roots descend, forming the cauda equina.
The spinal nerves exit the spinal canal through the intervertebral neuroforamina. At the cervical and thoracic level the nerve roots leave the spinal canal horizontally. At the lumbar level the nerve roots first descend in the lateral canal recess before exiting through the neuroforamen.
Vascular Structures
The spinal cord is supplied by three main arteries parallel to the spinal cord: one anterior and two posterior. The blood supply can be divided into three anatomical regions. In the cervicothoracic region the blood is supplied segmentally from arteries originating from the vertebral arteries and the great vessels of the neck (i.e. aorta, carotid and subclavian arteries). The midthoracic region receives most of its blood supply from collateral circulation from superior and inferior arteries and acts as a watershed area. The segmental blood supply is received from small perforants originating from the aorta. The thoracolumbar region is supplied by segmental arteries from the aorta and the iliac arteries. Variably originating from levels Th9 to L2 and in most cases from the left side of the vertebral column, the largest vessel originates from the aorta: the artery of Adamkiewicz.
The venous plexus in the spine is called the Batson plexus. This plexus is unique compared to other plexuses in the body as this venous plexus does not have valves, allowing retrograde flow in the venous network.
Craniocervical Junction
The craniocervical junction (CCJ) is the region connecting a spherical (head) and a tubular structure (spine). To stabilise this connection the craniocervical junction is composed of bones, ligaments and muscles.
The bony parts are formed by the occipital bone with a basilar part, squamous part (scale) and the lateral (condylar) part. At the cervical part of the connection, the atlas (C1) consists of an anterior and posterior arch, and two bulky lateral masses. The axis (C2) is formed by a vertebral body, pedicles, foramina transversaria, laminae, spinous process and the dens axis articulating anteriorly with the arcus anterior of the atlas.
The complex organisation of ligaments at the CCJ provides stability but allows a complex range of motion. These ligaments can be divided into the external and internal ligaments. The anterior external ligaments are formed by the ALL running along the anterior side of the vertebral bodies from C2 downward and the anterior atlanto-axial ligament connecting the ALL and the arcus anterior of the atlas. The ligament running between the arcus anterior of the atlas and the os occipitale is the atlanto-occipital ligament. Posteriorly the external ligaments consist of the extension of the ligamenta flava, the posterior atlanto-occipital and the posterior atlanto-axial ligament. The ligamentum nuchae runs from the external occipital protuberance to the spinous process of C7.
The internal ligaments of the CCJ consist anteriorly of a thin apical ligament and thick alar ligaments. The alar ligaments attach the axis to the skull base and run from the lateral aspect of the odontoid process to the anterior part of the foramen magnum. The middle internal ligament (cruciform ligament) is formed by the transverse ligament of C1, the accessory ligaments and the superior and inferior fibres. The transverse ligament is the largest, strongest and thickest craniocervical ligament and maintains stability by locking the anterior part of the odontoid process against the posterior side of the anterior arch of the atlas.12 It runs posterior to the odontoid process of the dens and attaches bilaterally on the lateral tubercle of C1. The posterior internal ligament is the tectorial membrane. Superiorly this ligament continues as the dura mater; inferiorly the ligament forms the posterior longitudinal ligament.
The function of the muscles in the CCJ is to initiate and maintain movement, and not to limit the movements of this joint. They can be grouped into flexion, extension, abduction, adduction and rotation.
Imaging Techniques
Multiple imaging techniques are available to evaluate the spine. The choice of imaging technique depends on the indication (e.g. traumatic or non-traumatic) and on the age of the patient. As MRI has become widely available in most countries it has become the first examination to perform in a non-traumatic setting. Especially in young patients it has the advantage not to use X-rays. In older patients computed tomography can be indicated to evaluate bony degenerative changes. If a contraindication for MRI is present, other imaging techniques (e.g. CT) are indicated.
In post-traumatic imaging CT is the preferred initial imaging technique in blunt spinal trauma patients. CT is also indicated in acute trauma patients when there is no optimal visualisation of the spine on plain film and in patients with unexplained focal pain or neurological deficit with a negative plain film, if unexplained soft-tissue swelling is present or when plain film is abnormal. Plain radiography can be performed in minor injuries. CT offers outstanding information about the bony lesions of the spine and reconstruction in virtually every anatomical plane. A group at the Harborview Medical Center in Seattle, Washington, defined a series of high-risk criteria to decide whether to perform plain radiography or CT imaging as the primary technique when imaging cervical spinal trauma (Table 54-1).13
TABLE 54-1
Harborview High-Risk Criteria
| If yes to any criteria, high risk for c-spine injury and indication for CT • Presence of significant head injury • Presence of focal neurological deficit(s) • Presence of pelvic or multiple extremity fractures • Combined impact of accident >50 km/h (>35 mph) • Death at the scene of the motor vehicle accident • Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|