Implementing Ultrasound in the Prehospital Setting
Nicole Danielle Hurst
INTRODUCTION
Rapid growth of new ultrasound applications is underway outside the traditional hospital setting. Disaster relief workers, medical personnel in austere settings, military personnel, prehospital providers, and patient transport teams are utilizing ultrasound with increasing frequency because it provides rapid and accurate patient assessment so paramount to timely and effective patient care. Regardless of the clinical setting, real-time diagnostic information provided by ultrasound can aid decision making. This is perhaps most true in the initial care of the undifferentiated patient frequently encountered in the prehospital setting, allowing early-care decisions and interventions to be made with increased certainty. Space restrictions, extreme environmental conditions, equipment limitations, or occasionally an overwhelming number of patients in need of care create extraordinary challenges. Ultrasound offers a highly versatile point-of-care resource ideal for these challenging settings.
Different out-of-hospital environments present unique technological challenges. For example, a military medic in the middle of a desert firefight using handheld ultrasound to diagnose and treat a pneumothorax may have different equipment requirements than a helicopter transport team monitoring a patient with a high-risk pregnancy. Recent developments in ultrasound technology have improved machine portability, performance under extreme environmental conditions, image quality, and software functioning. Research and development is meeting the challenges of the out-of-hospital setting, adapting to the unique demands of the prehospital environment and expanding the realm of ultrasound use.
EXISTING LITERATURE
Multiple Casualty Incidents
Unique characteristics of the multiple casualty incident (MCI) setting highlight the versatility of ultrasound for disaster response. Several descriptive reports of earthquake, tsunami, tropical storm, and mudslide disaster response describe an important role for ultrasound in relief efforts (1, 2, 3, 4, 5, 6). Hospital diagnostic imaging capabilities, if available, are uniformly overwhelmed by patient volume during an MCI, and ultrasound becomes the preferred imaging modality based on its efficiency, accessibility, and portability (5). The benefit of ultrasound portability is magnified when access to imaging equipment is limited due to destruction or concerns of structural damage to hospital facilities hampering access to diagnostic imaging (1). In such settings, sonographic evaluation is frequently performed outside or in makeshift care areas (1). MCIs frequently occur in developing countries or remote areas where ultrasound may be the only diagnostic imaging modality locally available (7). Local ultrasound machines and provider skills may be a vital resource during the immediate response phase, which relies solely on local resources (7).
Several applications have been described during the immediate response phase of an MCI. Ultrasound is primarily utilized to triage for surgery or evacuation, differentiate hemodynamically unstable patients, evaluate acute injury, and guide immediate interventions and procedures (1,5).
Ultrasound is potentially of greatest use when large numbers of casualties create high demand for rapid assessment and triage. Ultrasound was used during initial response by earthquake response teams in China, Armenia, Haiti, and Turkey as well
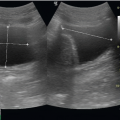
as during an MCI in the Second Lebanon Wa (1,4, 5, 6, 7, 8). After the Wenchuan earthquake in China, the Focused Assessment with Sonography for Trauma exam (FAST) was the primary imaging tool for trauma during the first 72 hours of the incident, and was used to evaluate 1386 of 3307 patients presenting to one response team (1). During the early response phase of the 1988 Armenian earthquake, 400 out of 750 injured patients were evaluated using ultrasound, deteing traumatic injuries of the abdomen in 12.8% of patients (5). Response teams for these two major earthquakes used ultrasound to triage patients for surgery by prioritizing sonographic evaluation of patients with unstable hemodynamics, limb or trunk injury with suspected visceral injury, and altered mental status (1,5). Major sonographic findings reported after earthquakes in the acute phase included hemoperitoneum, hemothorax, solid organ injury, renal injury, and musculoskeletal injury (1,5,6). In many cases, decisions for surgical intervention were based solely on physical exam and sonographic findings (5). In an MCI during the Second Lebanon War, 849 civilian and military casualties presented simultaneously to a level 1 trauma referral center for evaluation (8). Over 100 patients with suspected abdominal injury were initially triaged with a FAST exam to determine who required immediate surgery, further study with computed tomography (CT), or observation alone (8).
as during an MCI in the Second Lebanon Wa (1,4, 5, 6, 7, 8). After the Wenchuan earthquake in China, the Focused Assessment with Sonography for Trauma exam (FAST) was the primary imaging tool for trauma during the first 72 hours of the incident, and was used to evaluate 1386 of 3307 patients presenting to one response team (1). During the early response phase of the 1988 Armenian earthquake, 400 out of 750 injured patients were evaluated using ultrasound, deteing traumatic injuries of the abdomen in 12.8% of patients (5). Response teams for these two major earthquakes used ultrasound to triage patients for surgery by prioritizing sonographic evaluation of patients with unstable hemodynamics, limb or trunk injury with suspected visceral injury, and altered mental status (1,5). Major sonographic findings reported after earthquakes in the acute phase included hemoperitoneum, hemothorax, solid organ injury, renal injury, and musculoskeletal injury (1,5,6). In many cases, decisions for surgical intervention were based solely on physical exam and sonographic findings (5). In an MCI during the Second Lebanon War, 849 civilian and military casualties presented simultaneously to a level 1 trauma referral center for evaluation (8). Over 100 patients with suspected abdominal injury were initially triaged with a FAST exam to determine who required immediate surgery, further study with computed tomography (CT), or observation alone (8).
The best way to incorporate ultrasound into triage protocols is still being developed (9,10). Protocols that integrate ultrasound as a secondary triage tool have been suggested, including the CAVEAT protocol, which proposes comprehensive sonographic examination in the evaluation of the chest, abdomen, vena cava, and extremities in acute triage (11). Although the benefit of the CAVEAT protocol is yet to be tested in an MCI, there is extensive literature in support of its component parts (11).
In the acute response phase, sonographic evaluation can also be used at local receiving hospitals to evaluate crush injuries, assess shock states, and guide resuscitation (6). Anesthesiologists have described using ultrasound preoperatively for evaluation of systolic function and volume status (6). Inferior vena cava (IVC) and cardiac evaluation may be used to guide resuscitative efforts and volume replacement. Ultrasound can also be used to guide invasive resuscitative procedures such as central line placement.
Ultrasound is also useful for evaluating subacute complications that present remote to disaster incidents, either in location or by time (>72 hours) (2,3). For example, a problem-specific application of ultrasound has been used in the setting of decreased urine output to differentiate renal failure from rhabdomyolysis, dehydration, or renal parenchymal injury (5). One team applied a protocol that evaluated for urinary retention, disruption in kidney architecture, perinephric hematomas, free fluid in the abdomen, and determination of bladder size to estimate the likelihood of bladder rupture (5). Another team used Doppler to detect elevated renal resistive index to recognize and guide treatment of renal vasoconstriction found in acute crush-related renal injury (12). Ultrasound may also be useful for detecting (and sometimes treating) other commonly described delayed complications such as intra-abdominal abscess, deep venous thrombosis, cellulitis, abscess, and ileus (1,5,6).
Weeks after an MCI, indications for ultrasound become more routine, as patients utilize medical response units to replace nonfunctional local clinics or capitalize on the presence of medical care not usually available (2). When a hurricane caused a devastating mudslide in Guatemala in 2005, loss of potable water, food, sanitation, clothing, shelter, and lack of routine healthcare contributed to the bulk of medical cases that presented to a disaster relief team arriving 2 weeks after the mudslide (2). While ultrasound was used to evaluate a small number of thoracic trauma cases, it was primarily used for pregnancy-related conditions that were not directly caused by the mudslide (2). In this setting, cardiac and IVC measurements to estimate volume depletion from gastroenteritis may help direct rehydration therapy in areas with compromised sanitation and outbreaks of infectious gastroenteritis.
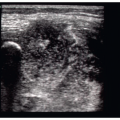
Depending on the type of MCI, unique injury patterns emerge that can be evaluated with ultrasound. The South Asia tsunami relief effort in 2004 described unique patterns of injuries suitable for ultrasound evaluation (3). Tidal waves caused high impact injuries with a predominance of musculoskeletal findings, including embedded foreign bodies, fractures, and dislocations. Victims were likely to sustain penetrating injuries from organic debris and material that was not visualized well by routine radiographic evaluation. Small or medium-sized openings in the skin frequently revealed surprisingly large amounts of foreign bodies such as sand, soil, and wood splinters. Contamination of wounds with seawater increased the rate of infection and abscess formation, which were also evaluated and treated using ultrasound. Lastly, seawater aspiration and near drowning were prevalent, resulting in noncardiac pulmonary edema, pleural effusion, pulmonary contusion, pneumothorax, aspiration pneumonia, acute respiratory distress syndrome (ARDS), and tsunami sinusitis. Thoracic ultrasound was additionally utilized to evaluate many of these pulmonary injuries. Lastly, limited X-ray resources can be rationed by using ultrasound for long-bone fracture detection and confirmation of alignment after reduction (13).
In addition to using ultrasound for diagnosis, ultrasound can be of benefit in improving the quality of care. Pain control in disaster settings is notoriously poor. A survey of 848 victims who survived the Wenchuan earthquake revealed that only 1.6% received pain control at rescue, 3.9% during transport to the hospital, 19% in the emergency department (ED), and 29% during debridement of wounds (14). Anesthesiologists report good outcomes for ultrasound-guided regional anesthesia both for pre- and post-operative pain control during MCI relief efforts (6). Ultrasound guidance is especially helpful for nerve blocks when a language barrier is present, because providers cannot rely on verbal communication regarding paresthesias to guide placement of anesthetic (6). Motor stimulation guidance for nerve blocks in traumatized patients can produce severe pain, but ultrasound guidance provides a good alternative for guidance (6). Additionally, ultrasound aids in precise delivery of anesthetic placement when normal anatomic landmarks are obscured by trauma. A review of epidemiology of injury patterns from recent disasters suggests that response personnel trained in four nerve blocks could provide relief for most extremity injuries: (a) femoral, (b) popliteal, (c) forearm, and (d) interscalene (15).
Military
Although the austerity of the battlefield environment limits the availability of many diagnostic and therapeutic modalities, ultrasound is currently being used at all levels of care. In fact, it is commonly the most advanced radiologic diagnostic
equipment available. A medic might carry a handheld ultrasound unit in his pack to help him diagnose, treat, and triage acute battlefield injuries. Medical air evacuation teams can reliably operate an ultrasound within a noisy helicopter without interfering with flight avionics (16). Highly mobile surgical teams that directly support combatant units are issued portable ultrasound machines as part of their routine equipment inventory. Combat support hospitals and regional hospitals use ultrasound in addition to more permanent radiologic equipment that is found in standard hospitals.
equipment available. A medic might carry a handheld ultrasound unit in his pack to help him diagnose, treat, and triage acute battlefield injuries. Medical air evacuation teams can reliably operate an ultrasound within a noisy helicopter without interfering with flight avionics (16). Highly mobile surgical teams that directly support combatant units are issued portable ultrasound machines as part of their routine equipment inventory. Combat support hospitals and regional hospitals use ultrasound in addition to more permanent radiologic equipment that is found in standard hospitals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree