Presentation and Presenting Images
( ▶ Fig. 22.1, ▶ Fig. 22.2, ▶ Fig. 22.3, ▶ Fig. 22.4, ▶ Fig. 22.5, ▶ Fig. 22.6, ▶ Fig. 22.7, ▶ Fig. 22.8)
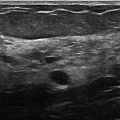
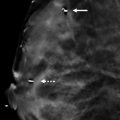
A 37-year-old female who is breast-feeding presents for her high-risk asymptomatic screening mammogram.
22.1.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
22.1.2 Imaging Findings
The breast tissue on the patient’s current mammogram has increased in density and there also appears to be more of it. The tissue in the upper outer quadrants appears more confluent and there is new tissue present in the left axillary region. Compare the current mammograms ( ▶ Fig. 22.1, ▶ Fig. 22.2, ▶ Fig. 22.3, and ▶ Fig. 22.4) with those of a year ago ( ▶ Fig. 22.5, ▶ Fig. 22.6, ▶ Fig. 22.7, and ▶ Fig. 22.8, respectively). All the breast tissue on the current mammograms has the same imaging appearance. No definite masses, architectural distortion, or calcifications are noted. The patient has two biopsy marking clips in the right breast from past magnetic resonance-guided (MR) and ultrasound-guided benign biopsies.
22.2 BI-RADS Classification and Action
Category 2: Benign
22.2.1 Differential Diagnosis
Breast tissue changes due to lactation: The breast tissue proliferates during lactation. Typically screening is not performed during lactation because of the decrease in sensitivity that the increased breast density introduces. In this case, the patient is high risk and will be breast feeding for several more months.
Incorrect comparative patient mammograms: When there is a marked contrast between sequential years of mammograms, it is always helpful to ensure that the correct patient’s images were placed in the file. In this case, it is the same patient. The biopsy clips aid in identifying that these are indeed of the same patient.
Weight loss: Weight loss will cause some increase in breast tissue density, but it will not result in proliferation of breast tissue as is seen in this case.
22.3 Essential Facts
It would appear the mammography procedure will cause the development of the cancer.
There is diminished sensitivity of mammography during lactation and pregnancy likely secondary to increased parenchymal density in the breast due to hormonal changes.
If imaging is necessary while a patient is lactating, it is advised that she breast-feed or pump prior to imaging to reduce the overall density of the breast tissue due to retained milk products.
Pregnancy-associated breast cancer accounts for 0.2 to 3.8% of all newly diagnosed cases of breast cancer.
Pregnancy-associated breast cancer is the most common malignancy of pregnancy, occurring in 1 in 3000 to 1 in 10,000 pregnancies.
22.4 Management and Digital Breast Tomosynthesis Principles
Screening mammography is generally not indicated for normal risk patients while pregnant or lactating.
Ultrasound is typically the first-line imaging modality that is used for symptomatic patients that are pregnant or lactating. The ultrasound findings may determine the need for mammographic imaging.
DBT imaging has been reported to improve sensitivity and specificity across all breast tissue densities. However, it is unclear if these results can be extrapolated to the breast tissue changes seen in pregnancy and during lactation.
22.5 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Vashi R, Hooley R, Butler R, Geisel J, Philpotts L. Breast imaging of the pregnant and lactating patient: imaging modalities and pregnancy-associated breast cancer. AJR Am J Roentgenol. 2013; 200(2): 321‐328 PubMed

Fig. 22.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree