CHAPTER 34 Indications and Patient Selection in Obstructive Coronary Disease
Since the advent of ECG-synchronized cardiac CT, this modality has become a rapidly evolving tool for noninvasive imaging of the coronary arteries.1,2 Advances in technology with fast data acquisition, improvements in temporal resolution, and high spatial resolution have contributed to the widespread acceptance of this test in a number of clinical scenarios. On the other hand, because of the rapid succession of technologic innovations, several scanner generations are currently in simultaneous clinical use.3 During the last decade, research has mainly been restricted to feasibility testing in tune with the rapid, roughly triennial, introduction of new multidetector-row CT (MDCT) scanner generations. Only recently do we see more emerging data of the greater impact of this potentially disruptive technology on the general field of health care. Albeit scarce, we see increasing evidence illustrating the cost-effectiveness of this test in the management of coronary heart disease.4 After years during which technologic development was focused almost exclusively on improved image quality and increased spatial resolution, particular attention is now being paid to mechanisms of radiation protection.5 Evidence-based guidelines have recently been implemented2,4 to steer the appropriate use and to avoid overuse of this test. This contribution aims to summarize the current indications for the use of coronary CT angiography (CTA) for assessment of obstructive native coronary artery disease (CAD).
OVERVIEW OF EVIDENCE AND TRENDS
Significant obstructive CAD is defined as a diameter stenosis of 70% or more in at least one major epicardial artery and as a 50% reduction in the case of the left main coronary artery. At coronary CTA, the assessment for hemodynamically significant coronary artery stenosis is roughly analogous to that of conventional invasive coronary angiography, which in clinical reality is ordinarily based on visual assessment and subjective estimation of stenosis severity. More objective assessment with quantitative catheter angiography is typically not routinely performed and is reserved for equivocal cases or research applications. Similarly, routine clinical coronary CTA evaluation of stenosis severity is ordinarily performed visually and subjectively, although virtually every currently available image display and analysis software platform provides semiautomated measurement tools for stenosis grading. These allow quantification of stenosis severity based on the ratio of stenosed arterial lumen relative to adjacent prestenotic and poststenotic segments with normal luminal diameters, similar to the standards as established, for instance, for intravascular ultrasound.6
A number of meta-analyses present an overview of the diagnostic performance of ECG-gated coronary CTA,7,8 and the number of studies is rapidly growing. One large analysis performed a systematic review of studies based on different scanner generations,3 illustrating the continuously improving image quality but also the growing experience of observers, as demonstrated by the high percentage of segments considered assessable with more recent scanner generations. Most important, however, a consistent performance with regard to the well-established high negative predictive value of this test, and thus the reliable exclusion of significant stenosis, is observed across scanner generations.
At present, the use of 16-slice MDCT with a gantry rotation speed of less than 500 ms is considered to meet the minimal requirements for successful ECG-gated imaging of the coronary arteries.2
False-negative findings, however rare, do occur. With regard to the clinically relevant per-patient analyses, many studies report between one and three patients who are missed by coronary CTA who have stenosis of more than 50%, a number that is fairly consistent across scanner generations, including the recently introduced dual-source CT (DSCT) technology.10 However the majority of missed stenoses were located in distal segments that are not amenable to revascularization.2
Noninvasive coronary CTA tends to overestimate disease. Main causes of false-positive findings are calcifications of the vessel wall and limited visualization of small-vessel lumens due to partial volume effects.9 The average positive predictive value is therefore moderate. Although average positive predictive values are reported to be higher with 64-slice CT,7 reports are ambiguous even with regard to the latest scanner types.10 Thus, coronary CTA should still be mainly regarded as a reliable tool to rule out significant obstructive disease rather than a means to estimate the severity of detected lesions.
Early evidence with use of 16-slice MDCT was characterized by excluding small vessels (<1.5 mm or <2 mm) or vessel segments with heavy calcifications or motion artifact from analysis, an approach that is not clinically feasible. More recently, in the majority of studies using 64-slice scanners, the entire coronary tree is considered for assessment. The number of nonassessable segments in the available literature has dropped from a mean 12% with 16-slice CT to 4% with 64-slice CT.7,8
SEGMENT-BASED AND PATIENT-BASED ANALYSIS
Indications
Throughout the available literature and for all scanner generations, it has been consistently found that ECG-synchronized coronary CTA has the ability to reliably rule out significant stenosis on the basis of the exceedingly high negative predictive value of this test. Selection of patients who most likely would benefit from noninvasive imaging of the coronary arteries is based on existing evidence on coronary CTA, known performance of conventional diagnostic procedures, and potential impact on patient management and risk estimation.4 Supported by broad consensus among experts, coronary CTA is recommended in symptomatic patients for the initial evaluation of chest pain in the setting of low to intermediate probability of CAD.3,5 In this context, coronary CTA is considered to have incremental value in patient management to inform the indication for invasive coronary angiography (Fig. 34-1). Of note, this target group (i.e., symptomatic patients with low to intermediate probability of CAD) is still different from the study populations on which most of the currently accepted clinical evidence is based. Invasive coronary angiography is typically not performed in patients with low probability of CAD.11 A few studies have closed this knowledge gap. Mejboom and colleagues10 investigated symptomatic patients at different levels of pretest likelihood and demonstrated that the performance of coronary CTA is inversely related to the probability of CAD. Coronary CTA was more accurate in patients with low to intermediate likelihood (Figs. 34-2 and 34-3) than in groups with high probability. The limited value in the latter group was explained by the high prevalence of advanced disease with heavy calcifications.
Therefore, symptomatic patients with high pretest probability are not appropriate candidates for noninvasive coronary CTA because this test is unlikely to add incremental value in their diagnostic work-up. Rather, invasive coronary angiography with the option of direct intervention and revascularization is the more appropriate initial procedure in the management of such patients (Fig. 34-4).9
Asymptomatic Patients
Cardiac CT is insufficiently validated for the application in asymptomatic individuals and is not currently recommended for this group.2,4 The characteristics of this test involving relatively high radiation doses and unclear cost/benefit currently do not support the use of coronary CTA as a screening modality.2,9 Whether coronary CTA may in the future have a role for better risk stratification in asymptomatic individuals at high Framingham risk12 or to detect silent CAD (e.g., in diabetic patients)13 remains to be established.
Estimation of Cardiovascular Risk and Pretest Probability for Coronary Artery Disease
An asymptomatic individual’s risk for future cardiovascular events is usually estimated on the basis of the traditional Framingham risk score, determining absolute and relative risk (compared with an age- and sex-adjusted low-risk group) of coronary heart disease.14 Risk is stratified to determine the appropriate level of aggressiveness in risk modification for disease prevention.
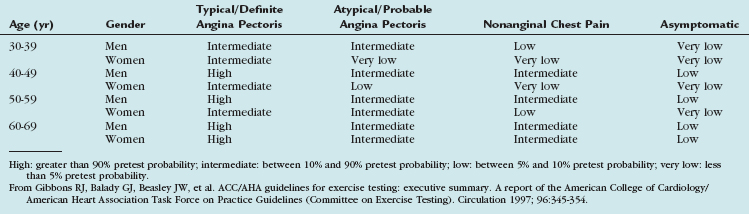
Pretest probability, on the other hand, is estimated in symptomatic patients, based on the quality of the chest pain (typical, atypical, and noncardiac quality; Table 34-1). Beyond symptoms, probability depends on age and gender (Table 34-2) and, as in the Duke score, may also include risk factors.12
TABLE 34-1 Clinical Classification of Chest Pain
| Typical angina (definite) |
| (1) Substernal chest discomfort with a characteristic quality and duration that is (2) provoked by exertion or emotional stress and (3) relieved by rest or nitroglycerin |
| Atypical angina (probable) |
| Meets 2 of the above characteristics |
| Noncardiac chest pain |
| Meets ≤1 of the typical angina characteristics |
From Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: executive summary and recommendations. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Chronic Stable Angina). Circulation 1999; 99:2829-2848.
Role of Coronary CT Angiography in the Context of Other Noninvasive Tests
Exercise testing and stress echocardiography are firmly established in the diagnostic algorithm of CAD, supported by extensive population-based evidence. Noninvasive stress testing provides functional and clinical information about the significance of myocardial hypoperfusion. Treadmill testing is a readily available low-cost procedure and is the primary tool in the diagnostic work-up of patients with suspected CAD. Similar to noninvasive angiography, exercise testing performs most accurately in patients with intermediate likelihood for CAD.13
Stress echocardiography is indicated as a second-line tool for patients who are unable to exercise.15 With recent developments in tissue Doppler imaging, improvements in the diagnostic performance of stress echocardiography have been reported. However, the modality is more sophisticated, and the diagnostic value depends on acoustic window and operator expertise. A considerable range of sensitivities and specificities is reported for both exercise testing and stress echocardiography to describe the accuracy of these tests for detection of significant CAD.15 Of note, the diagnostic accuracy of stress testing is recognized to be decreased in women, resulting in a higher rate of post-test referrals to invasive coronary angiography for women.16
Given the variable performance of noninvasive stress testing, particularly in women, a group of symptomatic and asymptomatic individuals is left in whom the probability after stress testing remains indeterminate. According to the National Cardiovascular Data Registry, a considerable part of invasive angiography is indicated by false-positive results of stress tests.17 Thus, most experts agree on the usefulness of coronary CTA in patients with inconclusive or uninterpretable stress test results.2,4
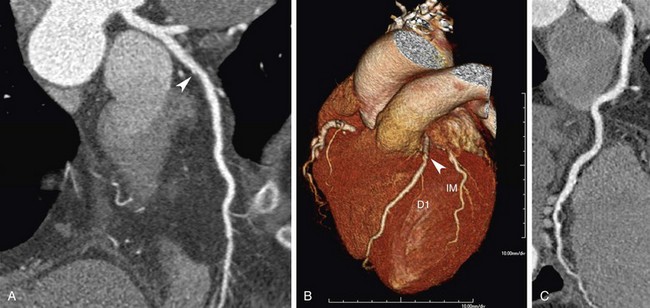
 FIGURE 34-1
FIGURE 34-1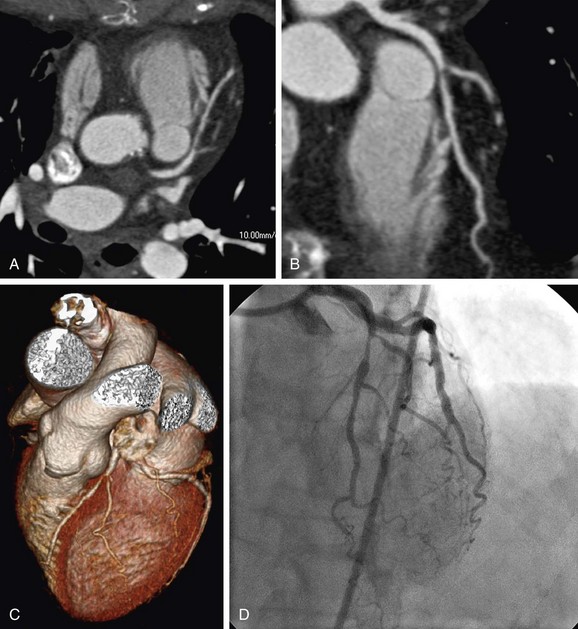
 FIGURE 34-2
FIGURE 34-2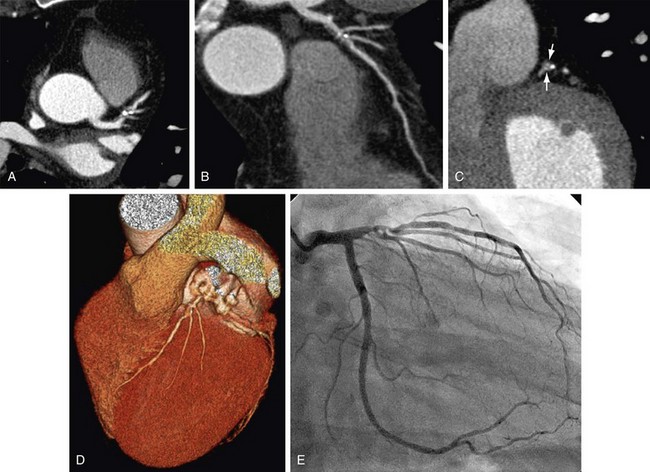
 FIGURE 34-3
FIGURE 34-3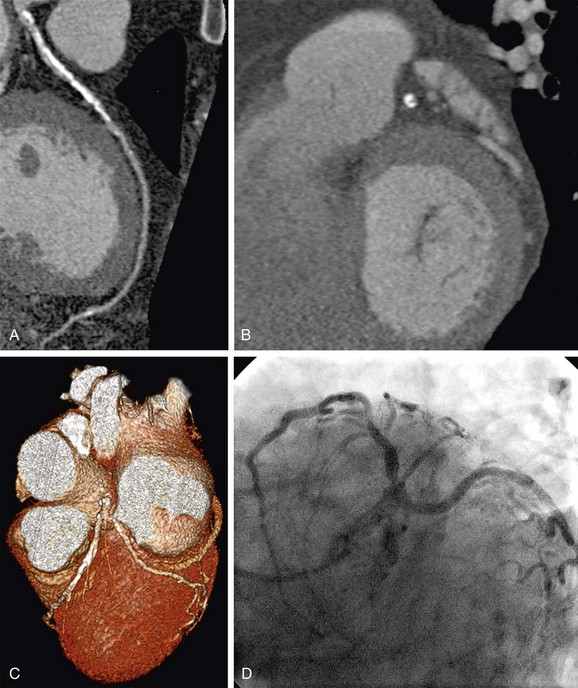
 FIGURE 34-4
FIGURE 34-4