Chapter 10
Infectious diseases of the liver
Ersan Altun1, Mohamed El-Azzazi1,2,3,4, and Richard C. Semelka1
1The University of North Carolina at Chapel Hill, Department of Radiology, Chapel Hill, NC, USA
2University of Dammam, Department of Radiology, Dammam, Saudi Arabia
3King Fahd Hospital of the University, Department of Radiology, Khobar, Saudi Arabia
4University of Al Azhar, Department of Radiology, Cairo, Egypt
Abscess
- Hepatic abscesses can be classified as pyogenic, amebic, and fungal.
- They may occur as single or multiple lesions.
- Infectious agents reach the liver through the hepatic artery, portal vein, biliary tract, and direct extension from contiguous organs.
- Pathology:
- Early stages: Liver abscesses are ill-defined with intense acute inflammation.
- Later stages: Liver abscesses become well-circumscribed and surrounded by a shell of granulation tissue.
- End stages: Liver abscesses show complete fibrous encapsulation.
- They may occur as single or multiple lesions.
- Pyogenic Abscesses
- Commonly occur as complications of ascending cholangitis and portal phlebitis.
- Common causative organisms include Escherichia coli, Clostridia species, Staphylococcus aureus, and Bacteriodes species.
- Presents with fever, right upper quadrant pain, tender hepatomegaly, and high white blood cell counts.
- Portal vein thrombosis may be associated with abscess.
- Pyogenic abscesses may be composed of small abscesses coalescing into and forming a multiloculated larger abscess cavity. This characteristic finding is known as the cluster of grapes sign (Figure 10.1).
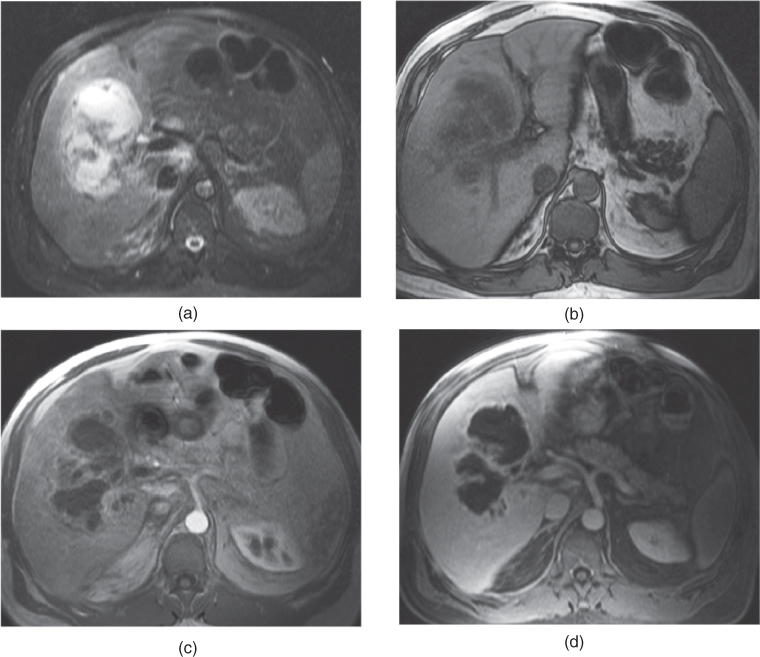
- Localized edema may surround the abscess cavity. When peripheral edema is present surrounding the enhancing pseudocapsule of abscess cavity, the appearance is called double target appearance on CT and MRI, which is described as the presence of the following from internal to external: hypodense/hypointense central area (abscess cavity); hyperdense/hyperintense enhancing pseudocapsule; and external hypodense/hypointense surrounding localized edema (Figures 10.2 and 10.3).
- Gas may be present in pyogenic abscesses.
- On CT:
- Pyogenic abscesses are seen as round or irregularly shaped hypoattenuating lesions on pre- and postcontrast examinations. Surrounding transient peripheral parenchymal enhancement on the hepatic arterial dominant phase is usually present, indicating the presence of hyperemia and inflammatory response in the surrounding liver parenchyma. Progressively intense rim enhancement of the pseudocapsule and enhancement of internal septations are seen on hepatic venous and interstitial phases of postcontrast examinations (Figure 10.3).
- On MRI:
- Pyogenic abscesses usually have high signal intensity on T2-WI, but mixed signal is a common feature among a population of lesions (Figure 10.4).
- Pyogenic abscesses usually have low signal intensity on T1- WI (Figure 10.4).
- Depending on their protein content, abscesses may have variable signal intensities on T2-WI and T1-WI. If an abscess has high protein content, it usually shows low signal on T2-WI and high signal on T1-WI. The feature of mixed T2 signal is helpful, if present, to distinguish from cysts/biliary hamartomas which generally do not contain protein/blood in the liver.
- Pyogenic abscesses are usually associated with moderate perilesional parenchymal transient enhancement with indistinct outer margins on the hepatic arterial dominant phase, which rapidly fade to isointensity with the remaining liver parenchyma on later phases on postgadolinium sequences (Figures 10.1, 10.2, 10.4, 10.5, 10.6). Moderate perilesional parenchymal transient enhancement reflects hyperemic inflammatory response in the adjacent liver parenchyma.
- Progressive moderate to intense enhancement of the wall and internal septations of abscesses are seen on all phases of postgadolinium sequences (Figures 10.1, 10.2, 10.4, 10.5, 10.6).
- Double target or cluster of grapes signs may be present (Figure 10.1).
- Layering of gas (signal void on both T2- and T1-WIs) (Figure 10.6) and debris (variable signal on T1-WI or T2-WI, most often low signal on T2- and high signal on T1-WI) due to high protein within the abscess cavity may be seen.
- Small abscesses may also show moderate enhancement due to enhancement of internal septations and prominent inflammatory response (Figure 10.7).
- Some pyogenic abscesses may also have very thick walls (Figure 10.5).
- Peripheral subcapsular abscesses especially develop secondary to operations and interventions (Figure 10.8)
- If the portal vein or its branches is thrombosed, the most important imaging finding is the absence of contrast enhancement of the portal vein on examination of all postgadolinium series. The infected bland thrombus may show high signal intensity on T2-WI and low to intermediate signal on T1-WI. Additionally, the portal vein wall may also show a moderate to intense enhancement, best seen on hepatic venous and interstitial phases of enhancement, which is the clue to its infected nature.
- Progressive moderate to intense enhancement of the wall and internal septations of abscesses are seen on all phases of postgadolinium sequences (Figures 10.1, 10.2, 10.4, 10.5, 10.6).
- Commonly occur as complications of ascending cholangitis and portal phlebitis.
- Amebic Abscesses
- Caused by Entameba histolytica.
- Presents with right upper quadrant pain, tender hepatomegaly, and diarrhea.
- Associated with a history of travel to an endemic area and positive serology.
- Lesions are usually solitary and affect the right lobe more often than the left lobe.
- Due to right lobe involvement and large size of the abscess, the diaphragm may be involved and pulmonary consolidation and empyema may be present.
- The radiologic features of amebic abscesses usually overlap with pyogenic abscesses. Lesions are encapsulated, thick-walled (5 to 10-mm), and demonstrate progressive substantial enhancement of the capsule on postcontrast images on MRI and CT. Amebic walls have thicker walls compared to the majority of pyogenic abscesses.
- Gas is usually not present within amebic abscesses.
- The differentiation of amebic abscesses from pyogenic abscesses is based on the clinical, radiologic, and serologic data, and is critical to determine as the treatment strategies are different for pyogenic abscesses compared to amebic abscesses. Amebic abscesses generally do not require drainage, whereas pyogenic abscesses may require intervention.
- Gas is usually not present within amebic abscesses.
- Caused by Entameba histolytica.
- Fungal Abscesses
- Are generally caused by Candida species, especially Candida Albicans, and seen in immune-compromised patients including AIDS patients, patients on chemotherapy especially for leukemia, patients undergoing bone marrow transplantation, and prolonged duration of neutropenia (Figure 10.9).
- Spleen is usually involved in combination with the liver (Figure 10.10).
- The kidneys may also be occasionally involved (Figure 10.10).
- Histoplasmosis, cryptococcus, mucormycosis, or aspergillus may also sometimes involve the liver.
- Imaging features of various fungal organism infections are similar.
- Candidiasis or other fungal infections may produce either little or no inflammatory/suppurative response, or occasionally granulomas in the liver. It is critical to be aware of this in immunocompromised patients, as, unlike pyogenic abscesses, little indication of the infective nature of the lesions is apparent, reflecting the inability of the host to mount an immune response.
- Hepatic candidiasis is typically characterized by the presence of microabscesses which contain the fungi in the center of the lesion, surrounded by necrosis and polymorphonuclear infiltrate.
- In the healing stage, microabscesses decrease in size and the amount of surrounding peripheral fibrous tissue increases (Figures 10.10 and 10.11)
- On CT:
- Abscesses are frequently smaller than 1-cm and are generally between 2 and 20 mm in size.
- Multiple small hypoattenuating lesions involving the liver and spleen are usually seen on contrast-enhanced CT examinations (Figure 10.10).
- They may not be detected on non-contrast enhanced CT examinations.
- Lesions may show no enhancement reflecting neutropenic state of patients, although in normal immune status patients, they usually display peripheral enhancement on contrast enhanced CT examinations. Additionally, lesions may occasionally show central enhancement on contrast enhanced CT examinations reflecting abundant inflammatory response or granuloma formation.
- On MR:
- Untreated Lesions – Acute Phase:
- Abscesses are frequently smaller than 1-cm and are generally between 2 and 20 mm in size.
- Multiple small foci of lesions with moderate to marked high signal on T2-WI, mild to moderate low signal on T1-WI. Peripheral rim enhancement on postgadolinium images (Figure 10.9) is apparent in normal immune status patients. Central enhancement is occasionally seen, which reflects that the lesions are in a phlegmonous or fibrinous state.
- Lesions may show no rim or perilesional enhancement in patients in a neutropenic state, although at least faint rim enhancement may be observed on later postgadolinium hepatic venous and interstitial phase images.
- Partially Treated Lesions – Subacute Phase (After the start of treatment)
- Lesions show mild to moderate high signal on T2-WI
- Lesions show variable signal ranging from mildly low signal to mild to moderately high signal on T1-WI.
- Dark perilesional rings may be observed on T1-WI or T2-WI, representing collections of iron-laden macrophages throughout granulation tissue surrounding and within the periphery of lesions (Figure 10.10).
- Lesions usually demonstrate peripheral enhancement on postgadolinium hepatic venous and interstitial phase images. Additionally, lesions may display central enhancement on postgadolinium hepatic venous and interstitial phase images, reflecting the reconstitution of immune response and granuloma formation.
- Completely Treated Lesions – Chronic Healed Lesions
- Lesions show mildly low signal on T1-WI and variable and mildly to moderately low-high signal on T2-WI (Figure 10.11).
- Lesions show negligible enhancement on postgadolinium images.
- Capsular retraction may be observed adjacent to the lesions due to their fibrotic nature.
- Lesions may show no enhancement reflecting neutropenic state of patients, although in normal immune status patients, they usually display peripheral enhancement on contrast enhanced CT examinations. Additionally, lesions may occasionally show central enhancement on contrast enhanced CT examinations reflecting abundant inflammatory response or granuloma formation.
- Are generally caused by Candida species, especially Candida Albicans, and seen in immune-compromised patients including AIDS patients, patients on chemotherapy especially for leukemia, patients undergoing bone marrow transplantation, and prolonged duration of neutropenia (Figure 10.9).
- Differential Diagnosis and Pearls for Abscesses
- Clinical history and laboratory findings are critical.
- Metastases may mimic abscesses as both show peripheral rim type of enhancement. Metastases can be distinguished from abscesses by observing progressive centripetal enhancement in late phases of contrast enhancement, which is a typical feature of metastases. Generally, any stroma related to abscesses exhibits enhancement on arterial phase images, with no progressive enhancement of previously unenhanced tissue; abscesses show progressively intense enhancement of already enhanced stroma (which can be marked) rather than progressive enhancement of previously unenhanced stroma. Progressively intense enhancement of internal septations of abscesses should not be confused with centripetal enhancement of solid metastatic tissue.
- Metastases with large necrotic components may mimic the appearance of hepatic abscesses, and the differentiation of these type of metastases from abscesses is difficult. This reflects that progressive centripetal enhancement, which is a distinguishing marker for metastases, is not present (due to necrosis) and therefore cannot be used as the distinctive feature. Clinical history therefore is of paramount importance. Although pyogenic abscesses always should have perilesional enhancement on optimally timed hepatic arterial dominant phase images, metastases exhibit this only for mucinous type tumors such as colon cancer. Attention therefore to this opposing phenomenon is also essential, as metastases may also show perilesional enhancement.
- Metastases may also mimic abscesses clinically if they become secondarily infected. This may sometimes be observed, particularly with colon cancer metastases.
- Metastases may mimic abscesses as both show peripheral rim type of enhancement. Metastases can be distinguished from abscesses by observing progressive centripetal enhancement in late phases of contrast enhancement, which is a typical feature of metastases. Generally, any stroma related to abscesses exhibits enhancement on arterial phase images, with no progressive enhancement of previously unenhanced tissue; abscesses show progressively intense enhancement of already enhanced stroma (which can be marked) rather than progressive enhancement of previously unenhanced stroma. Progressively intense enhancement of internal septations of abscesses should not be confused with centripetal enhancement of solid metastatic tissue.
- Clinical history and laboratory findings are critical.
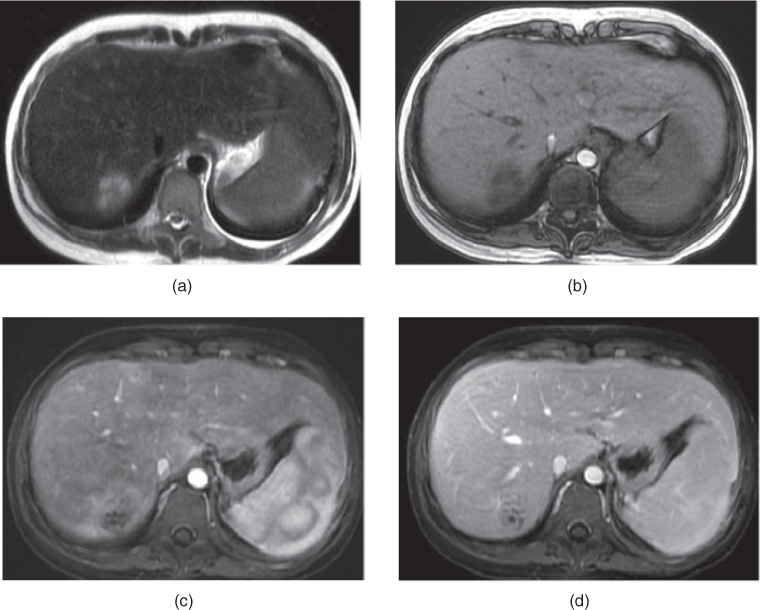
Figure 10.1 Transverse T2-weighted SS-ETSE (a), transverse T1-weighted 2D-GE (b), transverse T1-weighted hepatic arterial dominant phase (c), and hepatic venous phase (d) 3D-GE images demonstrate pyogenic abscess in the immunocompromised patient. The lesions show high signal on T2-weighted images (a), peripheral parenchymal transient enhancement on the hepatic arterial dominant phase images (c) and progressive enhancement on postgadolinium images (c, d). The lesion displays the “cluster of grapes” sign. Progressive rim enhancement and enhancement of internal septations are seen on postgadolinium images (c, d). The lesions are composed of small abscesses coalescing into and forming multiloculated larger abscess cavities.
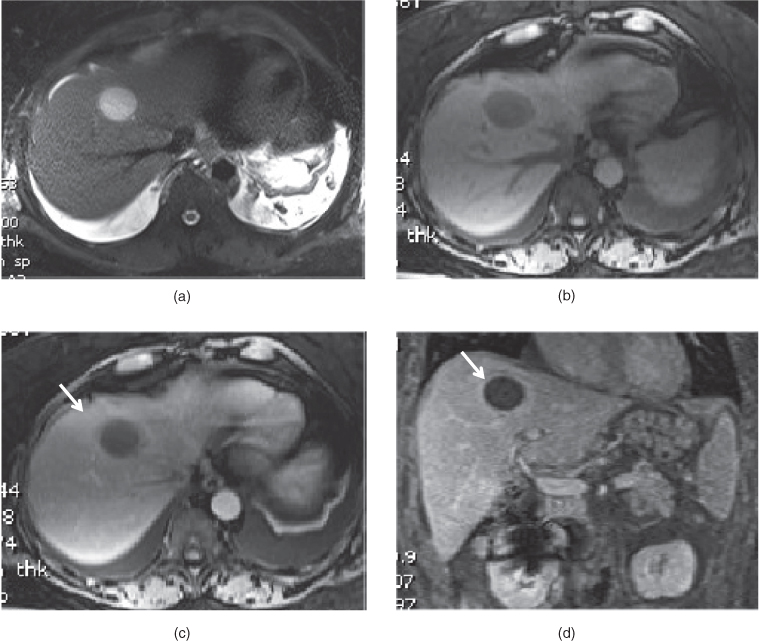
Figure 10.2 Transverse T2-weighted fat-suppressed SS-ETSE (a), T1-weighted fat-suppressed 3D-GE (b), T1-weighted fat-suppressed postgadolinium hepatic arterial dominant phase (d) and coronal hepatic venous phase (e) 3D-GE images demonstrate a solitary bacterial abscess. The abscess shows high signal intensity due to its high fluid content on T2-weighted image (a). Mild peripheral parenchymal transient enhancement (arrow, c) surrounding the abscess is noted on the hepatic arterial dominant phase (c). The enhancement of the wall of abscess (arrow, d) is noted on the hepatic venous phase image. Mild edema is also seen surrounding the abscess.
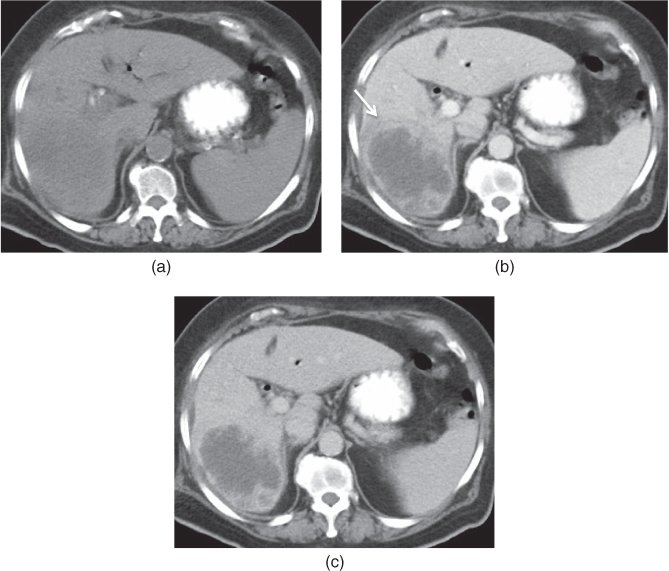
Figure 10.3 Transverse precontrast (a), postcontrast hepatic arterial dominant phase (b) and hepatic venous phase (c) CT images show a large abscess in the right lobe of the liver. The abscess has thick irregular walls. Peripheral surrounding parenchymal edema and early transient increased enhancement are detected in the early phase of enhancement (arrow, b). The walls of the abscess demonstrate thick irregular enhancement in the early and late phase of enhancement. Note that no stromal enhancement is seen in the abscess, which is a feature distinguishing abscess from metastasis.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree