Defined as couple’s inability to conceive after 1 year of unprotected intercourse
Primary—When the patient has never conceived.
Secondary—When there is h/o previous conception.
Factors need to be considered are
1. Ovarian follicular development
2. Ovulation
3. Formation of functional corpus luteum
4. Associated ovarian pathologies such as benign cysts (simple/complete dermoid/fibromas)
Follicular monitoring: Best done by transvaginal sonography (TVS):
Spontaneous cycles
Induced cycles
From 10th day of menstrual cycle, observe the developing/dominant follicle with the concurrent assessment of circulating estrogen levels. Predict impending ovulation. (Presence of cumulus oophorus)
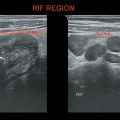
Ovulation occurs on ≅ 14th day of menstrual cycle in a 28-day cycle. Suggested by follicle rupture with crenated follicular walls with evacuation of follicular fluid and cumulus/oocyte complex with fluid in Pouch of Douglas (POD).
Corpus luteum develops after ovulation in normal cycle.
Corpus luteum cyst—2.5–4 centimeters diameter.
Corpus hemorrhagicum—Blood-filled corpus luteum.
Corpus albicans → hyperechoic structure in the ovary.
Growth of corpus luteum is proportional to luteal vascularity and serum progesterone concentration.
1. Absence of dominant follicle/or preovulatory follicle with low estrogen concentration
2. Ovulation failure
Failure of rupture of preovulatory follicle with extrusion of oocyte/cumulus complex with thick walls. (LUF syndrome—Luteinized unruptured follicle syndrome)
Capillaries in the follicular wall fenestrate and extravasate blood into the follicular lumen. (HAF—Hemorrhagic anovulatory follicle)
Correlate with basal body temperature (BBT) and midcycle progesterone levels.
Ovarian endometriomas—Functional endometrial tissue in ovary.
On USG—circumscribed cystic lesion with homogeneous low-level echoes.
Dermoid cysts—Heterogeneous mass with Rokitansky nodule (tip of iceberg).
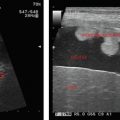
• Ovarian volume >9–11 cubic centimeters in asymptomatic patients.
• >10–12 follicles, 2–8 millimeters in size, peripherally placed (String of pearls/necklace sign) Graffian follicles in arrested stage of low FSH.
• High stromal echogenicity and may be a/w endometrial thickening in the uterus.
Table 29.1 Illustrating severity of OHSS with ovarian size
Severity | Mild | Moderate | Severe |
Ovarian size | >5 centimeters |