Inflammatory and Demyelinating Conditions
Sathish Kumar Dundamadappa
Aly H. Abayazeed
Shyam Sabat
Prachi Dubey
QUESTIONS
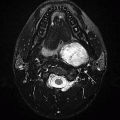
1 A 40-year-old previously healthy female presents with acute-onset right lower extremity weakness. NECT head shows a mass in the left perirolandic region, for which an MRI was recommended. Key images from the MRI are provided below.
|
1a What is the most likely diagnosis?
A. Glioblastoma
B. Primary CNS lymphoma
C. Balo concentric sclerosis
D. Metastatic disease
Hide Answer
1a Answer C. Balo concentric sclerosis. Balo concentric sclerosis is the most appropriate diagnosis because of the classic concentric morphology of the lesion resulting from alternating rings of demyelination.
1b Which of the following imaging features is typical for the above entity as shown in this case?
A. Lamellar demyelination with concentric morphology
B. Incomplete horseshoe shape of enhancement
C. Central necrosis and hemorrhage
D. Gray and white matter junction location.
Hide Answer
1b Answer A. Lamellar demyelination with concentric morphology. Lamellar demyelination with concentric morphology is the characteristic feature for this entity. Option B, suggesting incomplete horseshoe shape enhancement, is a feature seen with many forms of demyelination including multiple sclerosis.
|
Imaging Findings: A well-defined solitary lesion in the posterior left frontal lobe centered in the precentral gyrus with alternating T2/FLAIR hyper- and hypointensities in a concentric ring-like fashion, (A and B) with intense eccentric enhancement on postcontrast T1w sequences, (C and D) consistent with Balo concentric sclerosis.
Discussion: Balo concentric sclerosis (BCS) is a rare demyelinating disease, which is considered a variant of multiple sclerosis. Its characteristic feature is concentric morphology with alternating rings of myelin preservation and myelin loss. The demyelination starts centrally in the core and then extends outward in a concentric fashion. Unlike ADEM, BCS does not necessarily have to be a monophasic condition. Clinical course can range from a single self-limiting monophasic event to MS-like relapsing, remitting, and primary progressive forms. Treatment in the acute phase is with corticosteroids with excellent response, particularly if treatment is started early.
Differential Diagnosis: Acute disseminated encephalomyelitis, multiple sclerosis, abscesses, and neoplasm. The characteristic ring-like morphology however is typical for Balo concentric sclerosis, therefore it is the most likely diagnosis in this case. Abscess may have a similar appearance but will have a different clinical presentation, and typically, DWI shows intense restricted diffusion confined to the nonenhancing necrotic center compared to BCS, which shows alternating rings of diffusion restriction similar to the morphologic appearance on T2w sequences.
References: Darke M, Bahador FM, Miller DC, et al. Baló’s concentric sclerosis: imaging findings and pathological correlation. J Radiol Case Rep 2013;7(6):1-8.
Karaarslan E, Altintas A, Senol U, et al. Baló’s concentric sclerosis: clinical and radiologic features of five cases. AJNR Am J Neuroradiol 2001;22(7):1362-1327.
2 An 18-year-old female with encephalopathy, dysmetria, paresthesia, and clonus presents for initial evaluation to the ER. Following are some key images from her MRI.
|
2a Which of the following is a relevant past medical history that may be associated with this entity?
A. Recent viral infection, fever, or immunization
B. IV drug use
C. Recent high-speed motor vehicle accident
D. Immunocompromised state
Hide Answer
2a Answer A. Recent viral infection, fever, or immunization. Recent viral infection, fever, or immunization within past 2 to 4 weeks
2b In the clinical setting of recent upper respiratory tract infection, what is the most likely diagnosis?
A. Multiple sclerosis
B. Meningoencephalitis
C. Acute disseminated encephalomyelitis
D. Multifocal GBM
Hide Answer
2b Answer C. Acute disseminated encephalomyelitis.
|
Imaging Findings: Bilateral large areas of cortical/subcortical and deep white matter FLAIR hyperintensities (A and B) with corresponding enhancement (C and D).
Discussion: Acute disseminated encephalomyelitis (ADEM) is immune-mediated multifocal inflammatory disorder of the nervous system usually preceded by viral infection. Less commonly vaccination is the triggering event, 5% to 12% of patients. Often, no history of preceding illness elicited. This can occur at any age, but more common in pediatric population with median age of about 8 years.
The precise pathogenesis is not known. “Molecular mimicry” theory proposes cross-reactivity of antibodies to antigens in pathogens with myelin antigen. Per “inflammatory cascade theory,” either there is direct nervous tissue damage secondary to infection with antigens leaking into circulation or multiple cytokines/chemokines.
On imaging, there is generally widespread bilateral and asymmetric lesions. Subcortical and deep white matter are the most common sites involvement. Peripheral cortical involvement can be seen. Periventricular and callosal white matter involvement is less common, contrary to MS. Deep gray matter involvement is seen in about 50% cases. Cerebellar, brainstem, and spinal cord involvement is seen in 30% to 50% of patients. The lesion size varies from a few mm to large tumefactive nature. Enhancement is variable, and if present shows variable morphology, nodular, ring, diffuse and inhomogeneous. On CT, the lesions appear hypodense but CT is less sensitive for diagnosis. T2-weighted MR imaging is most sensitive, and the lesions are seen as ill-defined hyperintensities.
ADEM is generally monophasic. The lesions that evolve or appear within first 3 months are considered part of the initial disease. A subset of patients show recurrent or multiphasic disease. Recurrent ADEM refers to recurrence of lesions in the same location, and multiphasic disease refers to lesions occurrence at a different brain location.
Most of the patients show clinical as well as imaging resolution within months. Up to a quarter of patients can show subtle neurocognitive deficits. More aggressive variants of ADEM include acute hemorrhagic leukoencephalitis, acute hemorrhagic encephalomyelitis, and acute necrohemorrhagic leukoencephalitis.
Differential Diagnosis:
Multiple sclerosis: Generally smaller and well-defined lesions. “Black-hole” appearance of lesions on T1 images. Preferential involvement of periventricular and callosal white matter. Oligoclonal bands on CSF analysis
Vasculitis: Generally older age group. Hemorrhage is more common. Vascular imaging helps
References: Barkovich AJ, Raybaud C. Pediatric neuroimaging, 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2011.
Marin SE, Callen DJ. The magnetic resonance imaging appearance of monophasic acute disseminated encephalomyelitis. Neuroimaging Clin N Am 2013;23(2):245-266. doi: 10.1016/j. nic.2012.12.005.
3 A 22-year-old female presents with long-standing history of drug-resistant partial complex seizures and progressive cognitive decline. Key images are shown below:
|
3a What is the most likely diagnosis?
A. Sturge-Weber syndrome
B. Rasmussen encephalitis
C. Dyke-Davidoff-Masson syndrome
D. Focal cortical dysplasia
Hide Answer
3a Answer B. Rasmussen encephalitis. Profound atrophy in the right insulotemporal region in the setting of previous reported encephalitis is most compatible with Rasmussen encephalitis.
3b What are the most common changes expected on MRI during the prodromal phase of this illness?
A. Normal brain MRI
B. Cortical edema and enhancement.
C. Cortical restricted diffusion
D. Parenchymal petechial microhemorrhages
Hide Answer
3b Answer A. Normal brain MRI. In the prodromal phase of illness, the MRI and CT are usually normal.
|
Imaging Findings: There is nonenhancing atrophy in the left hemisphere with medial temporal, orbitofrontal (A), perisylvian, (B and C) volume loss.
Discussion: Rasmussen encephalitis is progressive unilateral focal encephalitis of uncertain etiology (viral trigger of genetic predisposition to immunodysfunction is suggested) that affects patients between 1 and 15 years of age.
Three phases of the disease:
Prodromal stage: Low seizure frequency; may exhibit mild hemiplegia. Imaging may be normal.
Acute stage: Seizures (partial complex seizures), progressive hemiparesis, and cognitive impairment. On imaging, there is swelling of the involved parenchyma, which is usually fronto-insular-temporal and may be parietal. Cortical and subcortical CT hypodensity and MRI T2 and FLAIR cortical and white matter (WM) hyperintensity may be seen. Pial or cortical enhancement secondary to the parenchymal inflammation is occasionally seen.
Residual or chronic stage: Stable neurologic deficits and continuing seizures refractory to medical treatment. On imaging, atrophy of the involved parenchyma may be seen
Differential Diagnosis:
Sturge-Weber syndrome: Port-wine facial nevus and enhancement of pial angioma are the classic findings. Cortical calcifications are also seen as well as parenchymal volume loss.
Dyke-Davidoff-Masson syndrome: There is unilateral brain atrophy, compensatory calvarial thickening, and hyperaeration of the paranasal sinuses following in utero or perinatal hemispheric infarction.
Focal cortical dysplasia: Blurring of gray-white matter junction, subcortical WM signal abnormality, cortical thickening and signal change, and abnormal sulcal/gyral pattern. WM signal tapering from subcortical region to the ventricular margin is the classic finding.
References: Faingold R, et al. MRI appearance of Rasmussen encephalitis. Pediatr Radiol 2009;39(7):756.
Fiorella DJ, et al. (18)F-fluorodeoxyglucose positron emission tomography and MR imaging findings in Rasmussen encephalitis. AJNR Am J Neuroradiol 2001;22(7):1291-1299.
Misra UK, et al. The prognostic role of magnetic resonance imaging and single-photon emission computed tomography in viral encephalitis. Acta Radiol 2008;49(7):827-832.
Varadkar S, et al. Rasmussen’s encephalitis: clinical features, pathobiology, and treatment advances. Lancet Neurol 2014;13(2):195-205.
4 A 19-year-old male with lymphoma presents with acute mental status change.
|
4a What is the most likely diagnosis?
A. Status epilepticus
B. Low-grade glioma
C. Herpes encephalitis
D. Autoimmune paraneoplastic limbic encephalitis
Hide Answer
4a Answer D. Autoimmune paraneoplastic limbic encephalitis. Autoimmune paraneoplastic limbic encephalitis, in view of the clinical history, is the most likely explanation for the T2/Flair hyperintensity in the bilateral medial temporal lobes (A and B) with restricted diffusion (C).
4b Which of the following have been implicated as a cause for nonneoplastic autoimmune limbic encephalitis?
A. Anti-glutamic acid decarboxylase (GAD) antibodies
B. Anti-Hu antibodies
C. Anti-Yo antibodies
D. Anti-Ri antibodies
Hide Answer
4b Answer A. Anti-glutamic acid decarboxylase (GAD) antibodies. Anti-glutamic acid decarboxylase antibodies have been implicated in nonneoplastic causes of autoimmune limbic encephalitis. The other antibodies mentioned in the answer choices have been associated with paraneoplastic encephalitis.
|
Imaging Findings: MR sequences demonstrate bilateral symmetric T2/FLAIR hyperintensity in the mesial temporal lobes (hippocampus and amygdala) (A and B) with significant enhancement (C) and no hemorrhage (D).
Discussion: Limbic encephalitis is the most common clinical paraneoplastic syndrome that is seen in patients with small cell lung cancer and is immune mediated by Anti-Hu autoantibodies (found in ˜60% of patients). Other cell surface antigens such as voltage-gated potassium channels (VGKC), N-methyl-D-aspartate receptor (NMDAR), and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR) may present with limbic encephalitis.
MRI is the most sensitive imaging modality (CT is usually normal) and will show T1 hypointensity, T2/FLAIR hyperintensity, no diffusion restriction, no hemorrhage, and occasional patchy enhancement in the mesial temporal lobes (hippocampus and amygdala), insula, cingulate gyrus, subfrontal cortex, and inferior frontal white matter.
FDG-PET will show increased glucose metabolism in the mesial temporal lobes. Other less common paraneoplastic syndromes:
Brainstem encephalitis: Seen with testicular germ cell tumors, on MRI will show T2 hyperintensity in the midbrain, pons, cerebellar peduncles, and basal ganglia.
Paraneoplastic cerebellar degeneration: Seen with breast cancer, ovarian cancer, and Hodgkin lymphoma; and on MRI will show cerebellar atrophy.
Differential Diagnosis:
Status epilepticus: Clinical history of seizure is usually present. On MRI, there is usually unilateral abnormal T2/FLAIR single corresponding to the clinical side of the seizure. DWI restriction and cortical enhancement are typical.
Low-grade glioma: Unilateral T2 hyperintense mass with mild mass effect. No enhancement is typical. Can be impossible to differentiate from limbic encephalitis.
Herpes encephalitis: DWI restriction, mass effect, enhancement, and hemorrhage are common. Characterized clinically by rapid-onset and febrile illness.
References: Darnell RB, et al. Paraneoplastic syndromes affecting the nervous system. Semin Oncol 2006;33(3):270-298.
Khan NL, et al. Histopathology of VGKC antibody-associated limbic encephalitis. Neurology 2009;72(19):1703-1705.
Kotsenas AL, et al. MRI findings in autoimmune voltage-gated potassium channel complex encephalitis with seizures: one potential etiology for mesial temporal sclerosis. AJNR Am J Neuroradiol 2014;35(1):84-89.
Voltz R, et al. A serologic marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer. N Engl J Med 1999;340(23):1788-1795.
5 A 55-year-old male with HIV positive status, noncompliant with antiretroviral treatment, presented with disorientation. Key images from an MRI are shown below:
|
5a Which of the following is the most likely diagnosis?
A. Lymphoma
B. Progressive multifocal leukoencephalopathy (PML)
C. HIV encephalitis
D. Toxoplasmosis
A lumbar puncture was performed and the patient was started on antiretroviral therapy, and appropriate treatment was started. After treatment, CD4 counts improved; however, there was further deterioration of clinical status. A repeat MRI was performed, and key images are provided below:
|
Hide Answer
5a Answer B. Progressive multifocal leukoencephalopathy (PML). There are nonenhancing asymmetric confluent white matter lesions with periventricular and subcortical involvement typical for PML.
5b Based on the above scenario, what is the most likely diagnosis?
A. Lymphoma
B. Progressive multifocal leukoencephalopathy (PML)
C. Kaposi sarcoma
D. Immune reconstitution inflammatory syndrome (IRIS)
Hide Answer
5b Answer D. Immune reconstitution inflammatory syndrome (IRIS). Presence of enhancement in the PML lesions with worsening of FLAIR hyperintensity upon immune reconstitution is most compatible with IRIS.
Imaging Findings: Figure 1. Confluent, large white matter FLAIR hyperintensities involving right frontal and parietooccipital lobes including subcortical U fiber involvement and lack of mass effect (A and B). No significant enhancement of mass effect is appreciated (C and D). In the current clinical setting, these findings most likely represent progressive multifocal leukoencephalopathy.
Figure 2. Subsequently, there is worsening of FLAIR hyperintense signal (A) and now development of intense enhancement (B and C). Findings are most compatible with immune reconstitution inflammatory syndrome (IRIS).
Discussion: Progressive multifocal leukoencephalopathy (PML) is a rapidly progressive and potentially fatal CNS infection due to reactivation of JC virus in the setting of immunosuppression. This includes severely immunosuppressed patients with HIV/AIDS, transplant recipients, or those undergoing monoclonal antibody treatment (e.g., natalizumab) such as for multiple sclerosis (MS). On imaging, these patients may present with extensive, confluent white matter changes, some of which may show restricted diffusion and hazy peripheral or nodular punctate enhancement.
Immune reconstitution inflammatory syndrome is seen with development of significant mass effect, often involvement of deep gray matter structures and more intense enhancement. PML-IRIS results after treatment with restoration of immunocompetence leading to an overwhelming inflammatory response directed against JC virus antigen. For clinical diagnosis of PML, clinical features, MRI findings, and lumbar puncture with CSF JCV PCR may be used for diagnosis.
Reference: Carruthers RL, et al. Progressive multifocal leukoencephalopathy and JC virus-related disease in modern neurology practice. Mult Scler Relat Disord 2014;3(4):419-430.
6 A 37-year-old previously healthy female presents with recent-onset memory loss and headaches. Key images from her MRI are provided below.
|
6a A ring-enhancing lesion was seen in the right periventricular posterior temporal lobe without restricted diffusion, (diffusion images not shown). What is the most likely diagnosis?
A. Abscess
B. Tumefactive demyelinating lesion
C. Low-grade astrocytoma
D. Primary CNS lymphoma
Hide Answer
6a Answer B. Tumefactive demyelinating lesion. The lack of restricted diffusion is atypical for abscess, and central nonenhancement is atypical for lymphoma. Low-grade astrocytoma is a differential possibility, but the age group, well-circumscribed nature, peripheral T2 hypointense ring, and thin rim of enhancement favor the diagnosis of demyelination.
6b A lumbar puncture was performed, and CSF studies were normal. The patient was started on IV steroids with excellent clinical response. Which of following is the best next step in management?
A. No further follow-up is needed.
B. FDG-PET
C. Routine clinical follow-up and an MRI within 6 to 8 weeks
D. Surgical biopsy
Hide Answer
6b Answer C. Routine clinical follow-up and an MRI within 6 to 8 weeks. Because of diagnostic overlaps, a short interval follow-up is prudent in such cases. In addition, because these patients can relapse into clinically definite multiple sclerosis or NMO, close clinical follow-up is also warranted. FDG-PET has been reported to be less intensely positive in tumefactive demyelination compared to neoplasm, but at this stage, with response to empiric treatment, this will not be the expected course of action.
|
Imaging Findings: This ring-enhancing lesion without restricted diffusion and a peripheral T2 hypointense ring is most likely to represent a tumefactive demyelinating lesion.
Discussion: Tumefactive demyelination.
Tumefactive demyelinating lesions are typically larger than 2 cm in size with mass effect and/or edema. Majority of the lesions are focal and supratentorial, making diagnosis difficult particularly if the patient has no known history of demyelinating disease. Certain imaging features, such as a T2-hypointense ring surrounding the lesion, open of ring of enhancement with the open aspect pointing toward gray matter and hypodensity on CT corresponding to the areas of enhancement on MRI have been associated with demyelinating lesions more than neoplasms or infections. Restricted diffusion may be seen in the lesion core or at the lesion edge. The degree of restricted diffusion with abscess is usually more intense than seen with tumefactive MS.
In the proper clinical setting, biopsy can be deferred in favor of empirical treatment unless a diagnosis of lymphoma is strongly suspected because CNS lymphoma often responds to steroids reducing the yield on subsequent biopsy. Even on biopsy, a 31% misdiagnosis rate has been reported, and often repeat biopsy has been suggested.
Short-term management with IV steroids is typically used with excellent response. Follow-up MRI within 6 to 8 weeks should be considered, particularly if the diagnosis of tumefactive demyelination is not confirmed.
References: Frederick MC, Cameron MH. Tumefactive demyelinating lesions in multiple sclerosis and associated disorders. Curr Neurol Neurosci Rep 2016;16(3):26.
Pilz G, Harrer A, Wipfler P, et al. Tumefactive MS lesions under fingolimod: a case report and literature review. Neurology 2013;81(19):1654-1658.
7 Following are the key images from a contrast-enhanced MRI of a 40-year-old female with diabetes.
|
7a Based on the above images, which of the following is the most likely symptom expected in this patient?
A. Left-sided facial paralysis
B. Right-sided facial pain and paresthesia
C. Left-sided sensorineural hearing loss
D. Fever, neck stiffness, and left-sided ear discharge
7b Which segment of the facial nerve most commonly exhibits physiologic enhancement?
A. Cisternal segment
B. Meatal or canalicular segment
C. Tympanic segment
D. Parotid segment
Hide Answer
7b Answer C. Tympanic segment. The proximal tympanic segment can normally enhance due to perineural venous plexus.
|
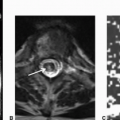
Imaging Findings: Enhancing meatal and labyrinthine segment of the left facial nerve is seen (B and C) without corresponding mass lesion or nodularity on the axial 3D CISS (A).
Discussion: Bell palsy is defined as acute peripheral nerve paralysis of unknown cause. Herpes simplex reactivation is the commonly proposed mechanism. Imaging is generally undertaken when the clinical presentation is unusual, to rule out other potential etiologies.
Contrast enhancement is most commonly seen at the geniculate ganglion and the proximal tympanic segment although mild enhancement has also been described in the mastoid , labyrinthine and meatal segments. This is due to the presence of a perineural venous plexus.
Distinctive imaging features of Bell palsy are abnormal enhancement of the facial nerve, commonly extending from intracanalicular through tympanic segment and at the most mild smooth enlargement of the nerve. This abnormal enhancement may persist for months after clinical improvement.
Other facial nerve neuritis can have a similar appearance. Ramsay Hunt syndrome (herpes zoster oticus) typically shows abnormal enhancement in the facial nerve, the vestibulocochlear nerve, the internal auditory canal, and often the inner ear labyrinth. Vesicles can be seen in the external ear. In cases of cranial nerve involvement with CNS Lyme disease, abnormal enhancement is seen in multiple cranial nerves, 7th nerve being the most commonly involved nerve. Unilateral involvement is more common, but bilateral involvement is characteristic.
If there is nodularity and enlargement of the nerve, alternate etiologies like metastasis, lymphoproliferative disorders, and perineural spread of malignancy should be considered.
Reference: Gebarski SS, Telian SA, Niparko JK. Enhancement along the normal facial nerve in the facial canal: MR imaging and anatomic correlation. Radiology 1992;183(2):391-394. doi: 10.1148/radiology.183.2.1561339.
8 A 36-year-old female with headaches and left upper extremity paresthesias presented for initial evaluation. An MRI was performed, and key images are provided below.
|
8a Initial workup revealed an abnormal chest x-ray and elevated serum angiotensin-converting enzyme (ACE) levels. Lumbar puncture was normal. Which of the following is the most likely diagnosis?
A. Multiple sclerosis
B. Subacute embolic infarction
C. Metastasis
D. Neurosarcoidosis
Hide Answer
8a Answer D. Neurosarcoidosis. It is the most likely diagnosis given the age group, reported chest x-ray findings, and elevated ACE levels.
8b How common is isolated neurosarcoidosis without systemic manifestations of sarcoidosis?
A. <1% of cases
B. 25% to 50% of cases
C. 50% to 75% of cases
D. >75% of cases
Hide Answer
8b Answer A. <1% of cases. Isolated CNS sarcoidosis without systemic manifestations is extremely rare, <1% of cases.
|
Imaging Findings: There is bilateral inferior frontal parenchymal T2 hyperintensity (A) with pial enhancement along the sulci (B and C).
Discussion: Sarcoidosis is an idiopathic systemic disorder characterized by noncaseating granulomas on pathology. Serum ACE levels have been found to be elevated during active disease and often used to diagnose and monitor the disease. Imaging features of neurosarcoidosis are nonspecific making it a challenging diagnosis in the absence of systemic disease. It has a predilection for basilar pial involvement; however, it can present with parenchymal, pial, and dural lesions anywhere in the brain. Management is not well established with steroids being the first line of treatment.
References: Smith AB, Horkanyne-Szakaly I, Schroeder JW, et al. From the radiologic pathology archives: mass lesions of the dura: beyond meningioma-radiologic-pathologic correlation. Radiographics 2014;34(2):295-312.
Smith JK, Matheus MG, Castillo M. Imaging manifestations of neurosarcoidosis. AJR Am J Roentgenol 2004;182(2):289-295.
9 A 45-year-female with multiple sclerosis presents for routine follow-up MRI.
|
9a According to the 2010 revised McDonald diagnostic criteria for multiple sclerosis, which of the following is defined as “dissemination in space”?
A. Clustered perpendicular periventricular lesions, (Dawson fingers)
B. Presence of an enhancing T2 hyperintense lesion
C. One or more lesion in at least two of four designated areas of CNS
D. Presence of T1 hypointense lesions at the callososeptal interface
Hide Answer
9a Answer C. One or more lesion in at least two of four designated areas of CNS. One or more lesion in at least two of four designated areas of CNS (periventricular, juxtacortical, infratentorial, or spinal cord).
9b What can be a potentially lethal complication of treatment with natalizumab, (Tysabri) in MS patients?
A. Drug-induced thrombocytopenia
B. Progressive multifocal leukoencephalopathy
C. Fulminant renal failure
D. Profound ototoxicity
Hide Answer
9b Answer B. Progressive multifocal leukoencephalopathy. Progressive multifocal leukoencephalopathy, due to JC virus reactivation in the setting of immunosuppression, is a potentially lethal complication of natalizumab and requires close clinical monitoring.
|
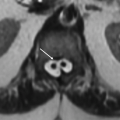
Imaging Findings: Scattered cortical/subcortical and pericallosal ovoid lesions characteristic for multiple sclerosis are seen (A and B). Note large juxtacortical lesion in the posterior temporal lobe, (arrow image A), which overlaps a part of the cortex. This image fulfills the criteria for dissemination in space with presence of both periventricular and cortical/juxtacortical lesions.
Discussion: Multiple sclerosis is a chronic demyelinating illness of the central nervous system with unclear pathogenesis. It has a female preponderance (˜2:1) and is more prevalent in the Caucasian population.
There are four major clinical subtypes of multiple sclerosis.
Relapsing-remitting multiple sclerosis (RRMS) (about 85%).
Secondary progressive multiple sclerosis (SPMS). Majority of RRMS convert to this type over years.
Primary progressive multiple sclerosis (PPMS). This subtype is progressive from the beginning (5% to 10% of MS patients). MRI findings are less dramatic relative to clinical disability.
Progressive relapsing multiple sclerosis (PRMS), involves relapses within PPMS. This is the rarest form of the disease.
MRI is a key factor in diagnosis of multiple sclerosis for assessment of dissemination in space and time to establish the diagnosis of multiple sclerosis.
According to the revised 2010 McDonald criteria, the presence of one or more lesions in the designated CNS regions is defined as dissemination in space. These regions are periventricular, juxtacortical, infratentorial, and spinal cord. However, subsequently, the recent expert consensus (MAGNIMS consensus guidelines, Lancet Neurology. 2016) recommends further revisions to the 2010 criteria, such as three or more periventricular lesions, inclusion of the optic nerve as another designated site and inclusion of cortical lesions instead of only juxtacortical lesions. Dissemination in time is defined as a new T2w or gadolinium-enhancing lesion on a follow-up MRI irrespective of the timing of the baseline MRI or simultaneous presence of an enhancing and nonenhancing lesion at any time.
On MRI, majority of these lesions are supratentorial. Less than 10% of lesions are infratentorial. The typical location is periventricular with perivenular distribution. They tend to be oval, round, or linear with an orientation parallel to lateral ventricles (“Dawson fingers”). Alternating areas of linear hyperintensity and isointensity along the ependyma on sagittal FLAIR images, known as “ependymal dot-line sign” is an early sign. On T1-weighted images, approximately 30% of these plaques appear hypointense (black holes). The T1 hypointensity in acute stages is mostly related to the edema and the majority become isointense within 3 months. The chronic black holes represent advanced axonal loss with greater extracapsular fluid and correlate with disability. Progressive atrophy indicating irreversible tissue damage also correlates with disability. Active lesions with disruption of the blood-brain barrier exhibit contrast enhancement on MRI. Less than 30% of patients show enhancing lesions. The classic peripheral enhancement incomplete ring of enhancement (horseshoe shaped) is often seen with larger lesions. Contrast enhancement in active lesions is transient and usually disappears by 4 weeks. It is unusual for a multiple sclerosis plaque to be enhancing beyond 3 months. Diffusion restriction can be seen in the small percentage of active lesions.
References: Filippi M, Rocca MA, Ciccarelli O, et al.; MAGNIMS Study Group. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol 2016;15(3):292-303.
Lassmann H. The pathologic substrate of magnetic resonance alterations in multiple sclerosis. Neuroimaging Clin N Am 2008;18(4):563-576. doi: 10.1016/j.nic.2008.06.005.
Osborn AG. Osborn’s brain: imaging, pathology, and anatomy, 1st ed. Salt Lake City, UT: Amirsys Publishing, 2013.
Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011;69(2):292-302.
Traboulsee A, Li DK. Conventional MR imaging. Neuroimaging Clin N Am 2008;18(4):651-673. doi: 10.1016/j.nic.2008.07.001.
A. Balo concentric sclerosis (BCS)
B. Neuromyelitis optica (NMO)
C. Marburg variant of multiple sclerosis
D. Susac syndrome
Hide Answer
10 Answer C. Marburg variant of multiple sclerosis. The confluent tumefactive lesions shown are typical for this entity. NMO typically shows mild to no brain involvement. BCS lesions show a typical lamellated appearance. Susac syndrome shows small lesions unlike this case, including characteristic central corpus callosal lesions.
|
Imaging Findings: Multiple confluent tumefactive hyperintense lesions on FLAIR with profound edema and mass effect (A to D).
Discussion: Marburg variant of multiple sclerosis is a rare entity with extensive multifocal areas of tumefactive demyelination. These lesions have severe inflammation and edema with evidence of enhancement and mass effect. Severe forms of ADEM may have a very similar appearance; however, ADEM is commonly seen in younger patients. Marburg variant has a severe and often lethal clinical course. Management is challenging relying on high-dose steroids, plasma exchange, immunoglobulin, and disease-modifying agents with poor outcome, such as severe disability or death.
Reference: Sarbu N, Shih RY, Jones RV, et al. White matter diseases with radiologic-pathologic correlation. Radiographics 2016;36(5):1426-1447.
11 A 35 year old male with acute onset encephalopathy, key images from an MRI are shown below:
|
11a Which of the following phrases best describes the abnormality, pointed by the arrow, on the above images?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree