Clinical Presentation
The patient is a 75-year-old male who presented with severe mid low back pain. He has difficulty walking distances but reports no lower extremity pain. Physical examination reveals some vague tenderness to deep palpation of the back. No lower extremity weakness. Normal sensory examination. Normal deep tendon reflexes.
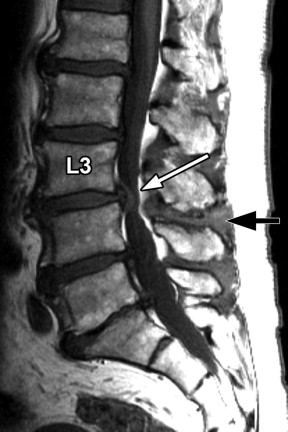
Imaging Presentation
Multilevel spondylosis deformans, intervertebral disc degeneration, and generalized disc bulging are seen with imaging. Severe circumferential thecal sac narrowing is present at the L3-4 level as a result of disc bulging, thickened ligamentum flava, and bilateral facet hypertrophy. Abnormal T2 signal hyperintensity and contrast enhancement is demonstrated in the L3-4 interspinous ligaments and adjacent spinous processes, and contrast enhancement of the L3-4 facet capsules is shown bilaterally. Findings are consistent with severe central stenosis at the L3-4 level, active inflammatory facet arthropathy, and interspinous ligamentous inflammation (i.e., interspinous bursitis, also known as Baastrup’s disease ) ( Figs. 39-1 to 39-7 ) .






Discussion
The space between adjacent lumbar spinous processes contains an interspinous ligament or ligaments and bilateral paraligamentous bursae. Small, short bilateral paired muscles, the interspinous lumborum muscles, are located on both sides of the interspinous ligament at a given lumbar level. These tissues can become inflamed and be a source of back pain. Interspinous ligamentous inflammation or bursitis (often referred to as Baastrup’s disease or Baastrup’s sign ) most commonly occurs at the L4-5 level but can occur at any lumbar level.
Normally, the spinous processes are covered by noncartilaginous connective tissue. As this disorder evolves, chronic active or episodic inflammation occurs in the interspinous ligaments, and over time the abutting surfaces of the involved spinous processes contact and eventually become flattened and sclerotic, with small cystic erosions or geodes occurring where the spinous processes contact ( Figs. 39-8 to 39-10 ) . This process may lead to interspinous adventitial bursal formation and eventually formation of a synovial-lined articulation between the spinous processes. When interspinous bursal formation occurs, both calcium pyrophosphate dihydrate (CPPD) and hydroxyapatite crystal deposition may be present in the bursa. When interspinous ligamentous inflammation occurs, the adjacent posterior paraspinal musculature and nearby facet capsules may also be inflamed ( Figs. 39-11 to 39-13 ) . Patients with interspinous ligamentous inflammation are usually symptomatic, reporting moderate to intense low back pain near the midline.













