In this article, we share our experience in establishing a clinic-based practice for MR imaging-guided interventions. Clinic resources and operational logistics are described and our institutional cost analysis for supporting the clinic activity is provided. We highlight the overall value of the clinic model in transitioning the field of interventional MR imaging from the “proof-of-concept” to the “working model” era and engage in a detailed discussion of our experience with the positive impact of the clinic on streamlining the procedural workflow, increasing awareness of the technology, expanding referral bases, and boosting the satisfaction of both patients and referring services.
Key points
- •
Implementing a clinic-based practice has positively impacted the maturation of Emory’s Interventional MRI Program into a regional destination for comprehensive MR imaging-guided interventional services.
- •
Providing a home for practice activities, the clinic represents a distinct and visible entity that is accessible by referring services and individual patients.
- •
The clinic-based operation represents a substantial departure from the tradition of episodic care that has long been associated with radiology services.
- •
The cost analysis of providing a regular interventional MR imaging clinic should not view this activity as merely a revenue-generating practice.
Introduction
MR imaging has lent itself to a unique role in guiding diagnostic and therapeutic interventional procedures for a variety of clinical indications. The integration of state-of-the-art MR imaging technology during interventions may be used to delineate an occult target; navigate an instrument through complex anatomic structures; accurately deliver a device, drug, or energy; and/or monitor the real-time effect of a treatment. These possibilities have expanded the scope of minimally invasive interventions beyond the current standards of care and have increased the options available for a sector of patients who, until recently, had a limited number of alternatives for diagnosis or treatment.
The field of interventional MR imaging has clearly grown over the past few years and has surpassed the “proof-of-concept” phase. The continued growth of this field is marked by the increasing number of academic institutions with interventional MR imaging capabilities, the growing diversity of interventional MR imaging applications adopted at these institutions, and the expanding technological innovations that support this growth and solidify our belief in a prosperous future for this field. Compared with conventional x-ray, CT, and ultrasound-guided interventions, interventional MR imaging still awaits wider implementation as a mainstream technology.
There have been a number of interesting discussions and debates within the interventional MR imaging community aimed at a better understanding of the current obstacles and challenges to a more widespread application of this unique and useful technology. A comprehensive overview of the highlighted challenges at these discussions is beyond the scope of this article. Among those challenges, the lack of clinical demand resulting from insufficient awareness of interventional MR imaging technology among referring physicians and patients, and the lack of streamlined efficient interventional MR imaging workflow strategies resulting from infrequent practice, are complex and interrelated issues relevant to the topic of a clinic-based practice model of interventional MR imaging.
The Interventional MRI Program at Emory University was launched in July of 2011 with a goal of establishing a destination site for a comprehensive clinical service of MR imaging-guided interventions. Learning from the evolution of the field of general interventional radiology and how the adoption of clinical-based practices had significantly boosted referrals for therapeutic procedures, we established the Interventional MRI Clinic in October of 2011 with a vision of breaking the cycle of “lack of demand”/”infrequent practice” through direct outreach to potential physician referral bases, creating a visible entity for patients and referring services to contact, and streamlining the issues related to interventional MR imaging workflow ( Fig. 1 ).
Introduction
MR imaging has lent itself to a unique role in guiding diagnostic and therapeutic interventional procedures for a variety of clinical indications. The integration of state-of-the-art MR imaging technology during interventions may be used to delineate an occult target; navigate an instrument through complex anatomic structures; accurately deliver a device, drug, or energy; and/or monitor the real-time effect of a treatment. These possibilities have expanded the scope of minimally invasive interventions beyond the current standards of care and have increased the options available for a sector of patients who, until recently, had a limited number of alternatives for diagnosis or treatment.
The field of interventional MR imaging has clearly grown over the past few years and has surpassed the “proof-of-concept” phase. The continued growth of this field is marked by the increasing number of academic institutions with interventional MR imaging capabilities, the growing diversity of interventional MR imaging applications adopted at these institutions, and the expanding technological innovations that support this growth and solidify our belief in a prosperous future for this field. Compared with conventional x-ray, CT, and ultrasound-guided interventions, interventional MR imaging still awaits wider implementation as a mainstream technology.
There have been a number of interesting discussions and debates within the interventional MR imaging community aimed at a better understanding of the current obstacles and challenges to a more widespread application of this unique and useful technology. A comprehensive overview of the highlighted challenges at these discussions is beyond the scope of this article. Among those challenges, the lack of clinical demand resulting from insufficient awareness of interventional MR imaging technology among referring physicians and patients, and the lack of streamlined efficient interventional MR imaging workflow strategies resulting from infrequent practice, are complex and interrelated issues relevant to the topic of a clinic-based practice model of interventional MR imaging.
The Interventional MRI Program at Emory University was launched in July of 2011 with a goal of establishing a destination site for a comprehensive clinical service of MR imaging-guided interventions. Learning from the evolution of the field of general interventional radiology and how the adoption of clinical-based practices had significantly boosted referrals for therapeutic procedures, we established the Interventional MRI Clinic in October of 2011 with a vision of breaking the cycle of “lack of demand”/”infrequent practice” through direct outreach to potential physician referral bases, creating a visible entity for patients and referring services to contact, and streamlining the issues related to interventional MR imaging workflow ( Fig. 1 ).
Practice philosophy and referral patterns
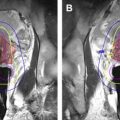
Emory’s Interventional MR imaging program has been in existence for 44 months with the Interventional MRI Clinic operating for 41 months. The practice now supports a direct referral process from both internal and external physicians and direct patient self-referrals. Our practice philosophy at the Emory’s Interventional MRI program has been to offer MR imaging guidance as a means for maintaining the minimally invasive diagnostic and therapeutic options for patients who are otherwise not suitable candidates for conventional interventional radiologic procedures, thereby complementing, rather than competing with, other coexisting hospital resources and services. This approach readily filters referrals to the interventional MR imaging service to those medically and/or technically challenging cases and has helped the recognition of the program as a unique and valuable institutional asset. Given the complexity of these cases, institutional multidisciplinary boards have become a major constituent of the program’s referral base with a growing number of community and regional health care entities becoming aware of the program and continually adding substantial numbers of referrals ( Fig. 2 ).
Currently, only patients undergoing assessment for, or follow-up after, therapeutic MR imaging-guided interventions are evaluated in the Interventional MRI Clinic. Diagnostic MR imaging-guided interventions (eg, biopsies) are typically needed on shorter notice than therapeutic interventions and are expected to be honored within 1 to 2 weeks so as to facilitate timely subsequent patient management. We believe that evaluating these patients in a dedicated clinic visit is neither necessary nor practical. Reviewing patients’ medical records, laboratory values, and prior imaging studies usually suffices in making a decision on the appropriateness of the procedure for the patient. Typically, the need for MR imaging guidance is explained to the patient by the clinic’s medical secretary during a phone call and is reviewed with the patient at the time of formal consent before the procedure. Some of these patients may subsequently be seen in the clinic if, based on the initial diagnostic procedure, a therapeutic MR imaging-guided intervention is needed (see Fig. 2 ).
Patients in the pediatric age group receive their MR imaging-guided interventions—typically sclerotherapy procedures performed for the treatment of low-flow vascular malformations—in a dedicated interventional MR imaging suite at the children’s hospital. These children undergo their initial examination, evaluation for procedure appropriateness, and follow-up assessments at the same Interventional MRI Clinic.
Patients undergoing neurosurgical MR imaging-guided interventions (eg, selective laser amygdalohippocampectomy, deep brain stimulator placement) are evaluated in a dedicated clinic operated by neurosurgery partners who share the same interventional MR imaging suite (see Fig. 2 ).
Clinic space and staff
The Interventional MRI Clinic uses a dedicated space at an outpatient Emory clinic facility. The interventional MR imaging clinic is held weekly on a half-day basis, alternating with other surgical and interventional radiology clinics. The clinic space is contiguous with the outpatient oncology center (The Winship Cancer Institute), facilitating coordinated visits with other care providers. The main Emory University Hospital facility is located across the street and is interconnected via a skywalk and a tunnel, facilitating patient access to preadmission testing on the same clinic visit day. Patient care at the clinic is supported by a clinical team composed of an MR imaging interventionist (S.N.) on 0.10 full-time equivalent (FTE) basis, a dedicated interventional MR imaging nurse practitioner on 0.20 FTE basis, a medical secretary on 0.20 FTE basis, and a registered nurse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree