Fig. 1
(a–e) Fluoroscopic control of the correct positioning of the electrothermic catheter (IDET) in the L4–L5 disc using the posterolateral approach
Warming of the fibrous annulus reduces the symptoms and stabilizes the discal lesion through the reorganization of the collagen fibers, the strengthening of the disc, the lesion of ring fissures, and ablation of pain receptors.
It is indicated for the treatment of bulging disc or contained herniated disc without root compression symptoms and resistance to pharmacological therapy and physiotherapy for more than 6 months.
To obtain a better evaluation of contained hernia, disc compression, or disc pressure, a previous discography may be needed.
The complication rate is 0.8 % with high frequency of osteonecrosis post-IDET.
The success rate is between 40 and 71 % of cases.
Percutaneous Coblation Nucleoplasty
This technique is performed with low temperatures (50–70°) differently from traditional radiofrequency that uses high temperatures (150–200°), obtaining the same results in a shorter time (2–3″ versus 15–17″).
Under fluoroscopic guidance, a thermic coagulator (Perc-D coblation Probe) is introduced into the nucleus pulposus; then a bipolar current is applied on the extremity of the electrode, producing a radiofrequency field that breaks collagen bonds. It creates inside the nucleus “an ionic plasma” containing simple molecules and ionized gas such as O2, H2, and NO that will be removed through the needle used to introduce the electrode. The warmth produced does not exceed 70°, and it has a limited diffusion of 2 mm, creating a canal of thermic lesion in the nucleus pulposus. By a manual 360° rotation of the probe for 6 times, without any other movements of in-outside, the system creates six canals of thermic lesion with a rapid dehydration of the nucleus and reduction of disc volume of about 10–20 %. The following contraction of the collagen fibers allows the reduction of the protruded portion with decompression of the compressed root (Fig. 2a–b).
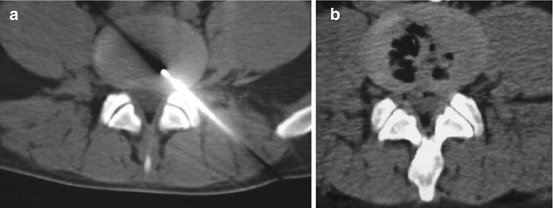
Fig. 2
(a) Coblation nucleoplasty at level L4–L5 under CT control using the posterolateral approach in a patient in the prone position; (b) posttreatment control LL and AP fluoroscopic control of the correct position of the needle at the C5–C6 level
Essential condition is the integrity of the fibrous annulus; otherwise, the mechanism of retraction cannot happen. Best indication is the symptomatic herniated but not extruded disc.
Results obtained from control trials report the resolution of pain symptoms in 70–80 % of cases with duration of pain relief for at least 6 months.
The risk of complications is very low. Principal complications are discitis, anterior disc perforation caused by probe, and cauda equina syndrome.
Dekompressor Percutaneous Discectomy
The aim of this technique is to remove the nucleus pulposus.
A discogram is suggested.
The dekompressor probe (Stryker, Kalamazoo, MI, USA) is introduced through the coaxial 17 gauge trocar into the nucleus pulposus. The trocar can be curved manually if the access is difficult, especially when the herniated disc is at level L5–S1. After switching on the rotating engine, the probe is moved forward and backward, removing and removing tissue (Fig. 3a–d).
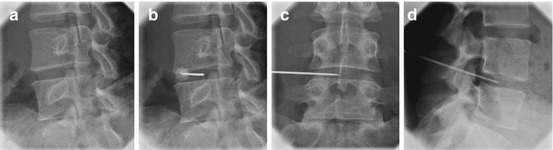
Fig. 3
(a–d) Dekompressor percutaneous discectomy at level L4–L5 in patient in the prone position and under fluoroscopic guidance with oblique tube orientation using the posterolateral approach
The procedure is complete when there is no more material to extract or when the radiologist feels obtaining a satisfactory decompression.
The lumbar percutaneous discectomy dekompressor can be performed under CT or fluoroscopic guidance, without technique limitations; however, if it is performed by fluoroscopic guidance with the patient in the prone position, a posterolateral approach is needed to arrive into the disc using the lateral foramen as the landmark.
The location of the hernia is the most important parameter for the efficacy of therapy. The indications are central or posterolateral and foraminal or extraforaminal herniated disc. The reduction of symptoms is over 70 in 79 % of foraminal posterolateral or extraforaminal hernia.
This technique offers many advantages:
The calibre of the probe is only 16G (1.5 mm), reducing the risk of damage to the longitudinal posterior ligament and the annulus.
The probe and the trocar can be curved manually in case of difficult approach.
The probe rotation system allows the nucleus aspiration not only in case of central or paracentral herniation but also in case of foraminal and extraforaminal herniated disc without root damage.
Removing 3 cm of disc material resulted in a significant pressure decrease on the peripheral disc portion, resolving the disc-radicular conflict.
Success is achieved in 70–79 % of cases.
Three cases of broken probe have been reported.
Chemodiscolysis with O2-O3 Mixture with Periradicular and Periganglionic Infiltration
Ozone is an unstable, colorless, irritating gas, with a thorny smell, oxidative power, and antiseptic, disinfectant, and antiviral properties. It is prepared and used in real time, transforming a small percentage of O2 to O3 by special generators. The mixture O2-O3 is injected in the intradiscal space and in the foramen: 3–4 mL in the disc and 10 mL in the foramen. The administrated dose for treating the disc is 30–40 μm/mL, and it is resulted to be the best concentration to dehydrate the nucleus and to reduce the inflammation.
The rationale is that the pain is due to mechanical compression on the root with associated inflammatory changes in periganglionic and periradicular spaces.
With the patient in the prone position, the technique is usually performed under CT for better evaluation of gas distribution into the disc or periganglionic space.
The technique can be performed also by fluoroscopic guidance with control of the intradiscal or canal gas distribution.
A needle is inserted in the nucleus pulposus (18–20 gauge calibre and 7–10 cm length) by oblique paravertebral approach using as target the specific articular facet (Fig. 4a–c). Sometimes, especially at the L5–S1 level, when the “classic” oblique approach might be difficult for anatomical reasons, a further needle inclination of 30° is necessary in the craniocaudal direction, to reach the specific disc space, or a translaminar medial approach should be performed without fear of crossing the dural sac to reach the vertebral disc (Figs. 5a–d and 6a–c).
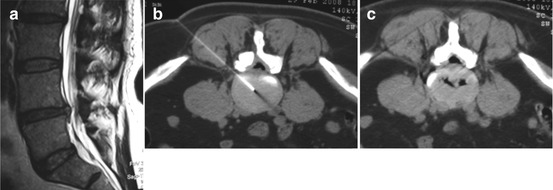
Fig. 4
(a) Sagittal T2W MRI shows a herniated disc at level L4–L5; (b) axial T2W MRI shows right posterolateral herniated disc L4–L5; (c) axial CT at level L4–L5 in a patient in the prone position; the needle is inserted in the nucleus pulposus L4–L5 by the posterolateral approach, with gas distribution into the disc and right periganglionic space
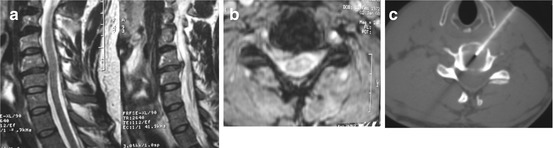
Fig. 5
(a) Sagittal T2W MRI shows a herniated disc at level L5–S1; (b) axial T2W MRI shows left posterolateral herniated disc at L5–S1; (c) axial CT at level L5–S1 in a patient in the prone position; the needle is inserted into the nucleus pulposus L5–S1 by left translaminar approach
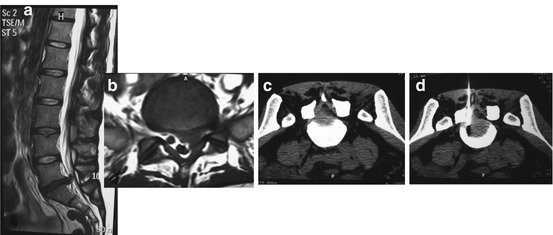
Fig. 6
(a, b) Sagittal and axial T2W show a herniated disc at level C5–C6; (c and d) axial CT at level C5–C6 in a patient in the supine position; the needle is inserted into the nucleus pulposus by anterolateral approach with manual dislocation of the carotid axis
The needle is placed in the center of the disc and the gas mixture is slowly injected in the nucleus pulposus, then into the epidural and intraforaminal space with a local anti-inflammatory effect.
Extruded herniated disc or free herniated fragments are contraindications.
Discography is not needed because it adds no diagnostic information necessary for the treatment and may affect the impact of the ozone gas.
The oxygen-ozone mechanisms of action have been investigated and include:
Anti-inflammatory effect due to oxidative action on the chemical pain mediators.
Improvement of capillary blood perfusion and the resolution of venous stasis with better tissue oxygenation and reduction of the root edema.
Direct action, through oxygenation process, on the bounds of nucleus pulposus mucopolysaccharides filled with water with secondary disc dehydration.
No damage is reported if the O2-O3 goes into the CSF or subarachnoid space.
The success rate is reported in 70–80 % of cases.
No early or late neurological or infectious complications have been reported following O2-O3 injection.
A recent meta-analysis about the effectiveness and safety of ozone treatments for herniated lumbar discs shows that pain and function outcomes are similar to the outcomes for lumbar discs treated with surgical discectomy, but the complication rate is much lower (<0.1 %) and the recovery time is significantly shorter.
Jellified Ethyl Alcohol (Discogel®)
It is formed by a sterile viscous solution containing 96 % pure ethyl alcohol (a cellulose derivative product) added to a radiopaque element – tungsten – that when injected into the vertebral disc at the cervical or lumbar level produces a local necrosis of the nucleus pulposus. Its action is mechanical via dehydration of the turgescent and protruding disc, which is compressing the peripheral nerves of the cord, causing extreme pain.
After asepsis and local anesthesia, the product is injected into the nucleus pulposus under CT or fluoroscopic guide with post-lateral approach for thoracic or lumbar level and anterolateral approach at for the cervical level.
Preferably the disc is punctured using a small needle of:
18 gauge for thoracic and lumbar discs, so as to reach the central region of the intraspinal space.
20 gauge for cervical disc.
The quantity of jellified ethyl alcohol injected varies between 0.2 and 0.8 mL, according to the dimension of the disc and extent of the hernia.
It is recommended to use:
0.2 mL of jellified ethyl alcohol for cervical discs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree