Imaging Presentation
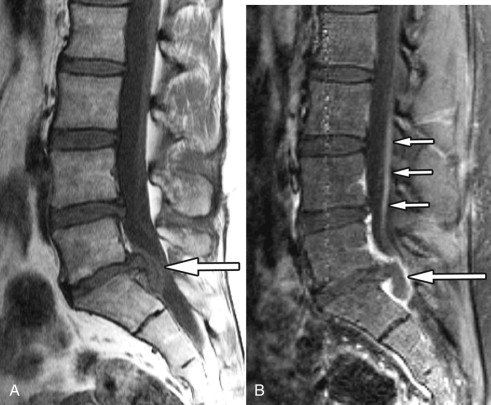
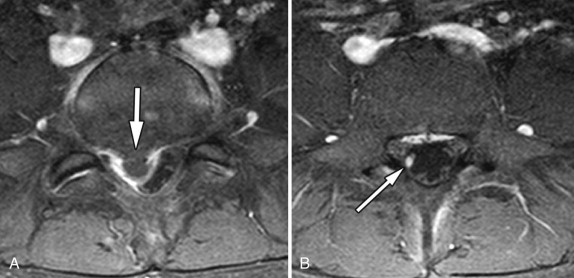
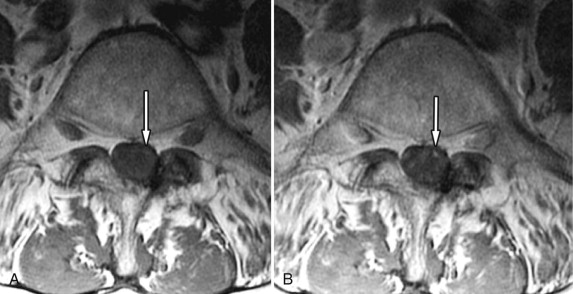
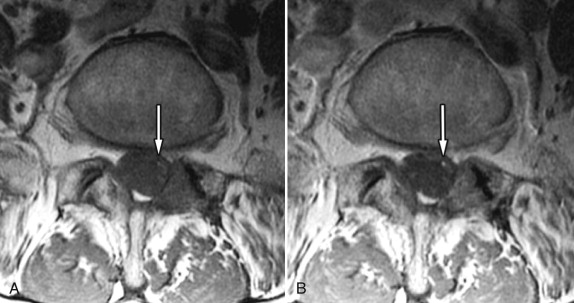
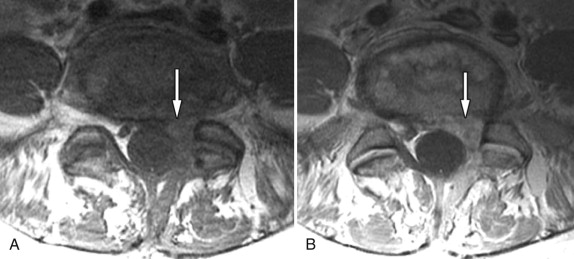
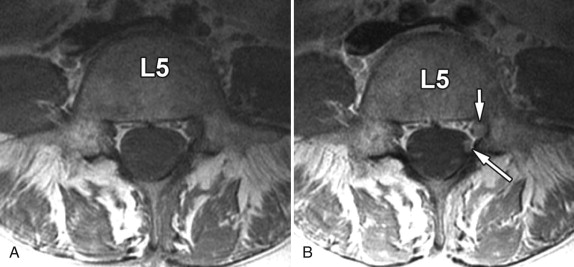
Magnetic resonance (MR) imaging reveals a very large disc extrusion compressing the thecal sac on the right at the L5-S1 level. There is intense contrast enhancement surrounding the disc fragment and diffuse enhancement of the intrathecal right S1 nerve root above the level of the disc herniation, indicating S1 radiculitis ( Figs. 40-1 to 40-3 ) .
Discussion
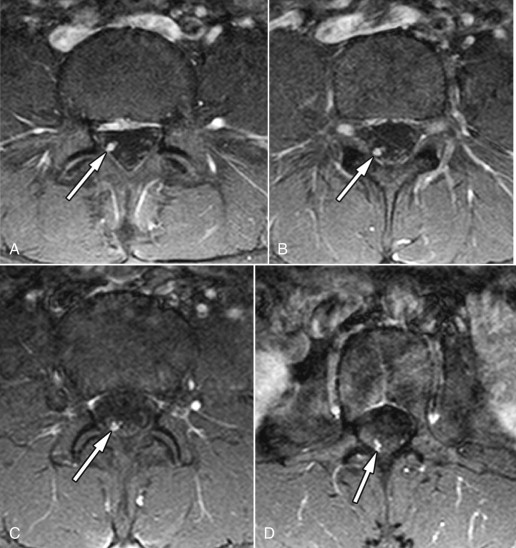
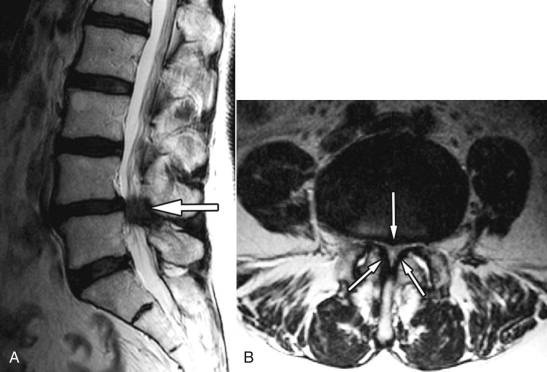
Intrathecal radiculitis is an important pain-producing condition that is frequently not recognized, which is supported by the fact that there exists a paucity of publications in the literature on this subject. Takata and colleagues in 1988 described visible intrathecal nerve root swelling on post-myelogram computed tomography (CT) images in 60% of the patients in their series who had symptomatic lumbar disc herniations. The enlarged intrathecal nerve root is often caused by a disc herniation, central canal stenosis, or postoperative granulation tissue ( Figs. 40-1 to 40-11 ) . The affected nerve corresponds to the patient’s radicular pain distribution. Intrathecal nerve roots of the cauda equina may enhance on MR imaging after IV contrast enhancement if the blood nerve barrier that normally exists is disrupted. The blood-nerve barrier can break down as a result of mechanical factors, trauma, an autoimmune response, or ischemia. Mechanical compression of the nerve root can result in neural edema and eventually ischemic compromise of the nerve root if the condition is prolonged. Although the precise cause of the blood-nerve breakdown is not known, the nerve root enhancement likely reflects a low-grade inflammatory process involving one or more cauda equina nerve roots; hence, we refer to this condition as intrathecal radiculitis . Intrathecal radiculitis may occur preoperatively or postoperatively and may occur with or without nerve root enlargement (see Figs. 40-1 to 40-9 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








