Fig. 1.1
(a) Example of short-axis (to the nerve) in-plane (to the needle) injection. (b) Example of short-axis (to the nerve) out-of-plane (to the needle) injection
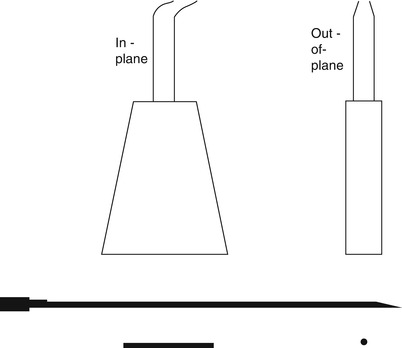
Fig. 1.2
When the needle is inserted in-plane it can be seen in its entirety, tip always in view. When the needle is inserted out-of-plane, only a cross section of the needle can be visualized and you cannot tell how deep it has advanced
Setting Up an Exam
First and foremost, the practitioner must be in a comfortable and ergonomic position to perform an injection. Next the patient must be comfortable. Injections can be done with the patient seated, supine, side-lying or prone. For patients prone to vasovagal responses or with poor balance or trunk control, seated is not recommended. For anxious patients, oral anxiolytics may be needed on occasion. For cervical procedures, an intravenous line may be placed. Risks, benefits, and alternatives of all procedures should be discussed with the patient and their family, and informed consent obtained. Common risks to all injections include bleeding, infection, worsening pain, allergic reaction, nerve damage, tendon, or ligament rupture. Risks specific to corticosteroids include local atrophy or skin depigmentation, increased blood pressure or sugar, mood swings, insomnia, rash, and flushing, but these are rare at the doses most commonly used.
The appropriate type of machine and transducer should then be selected. High-frequency linear array transducers (usually 10 MHz+) have higher resolution and have allowed the growth in musculoskeletal ultrasound (MSK-US) to be possible [6]. They are usually preferred for injections and come in wide, medium, or small footprint “hockey-stick” sizes. Certain structures are more easily injected with small footprint probes (finger, toe joints), but usually the larger the footprint, the better because greater areas of tissue can be scanned at a time.
Low-frequency (curvilinear) transducers are helpful for imaging deeper structures, have large footprints, but have poorer resolution. They usually run in the 2–6 MHz range. It is easier to localize a needle at the beginning of an injection because the ultrasound beams are directed perpendicularly at the obliquely oriented needle; as the needle is advanced, the center of the transducer now emits beams 90° to the skin but oblique to the advancing needle. The transducer must be “heel-toed” or “rocked” to promote a more perpendicular beam orientation (Table 1.1).
Table 1.1
Transducers and frequency
Type of transducer | Frequency | ||
|---|---|---|---|
Linear | More accurate, less anisotropy | High frequency (10 MHz+) | Better resolution, less depth |
Curvilinear | May help with needle visualization | Low frequency (5–2 MHz) | Poorer resolution, better depth |
Larger footprint | |||
Hockey stick | Smaller footprint for interventions | High frequency (10 MHz+) | Better resolution, less depth |
Once the appropriate machine and transducer are selected, input the patient’s demographics and adjust the presets (small parts, MSK, superficial, etc.). Many machines also come with needle enhancement software, which directs the beam more perpendicular to the needle rather than the skin. While helpful in some cases, these software tools are in no way as helpful as proper technique in maximizing needle visualization.
Place gel and a probe cover, followed by additional gel, then apply the probe. Grab the probe firmly and always brace the hand scanning against the skin. Once an image is obtained, identify a bony landmark and work off of that. Optimize the image by adjusting the depth, then focal zone. The number and width of focal zones can often be adjusted. The time gain compensation (TGC) can also be tuned to optimize visualization of structures at specific depths by selectively directing the sound beams, reducing attenuation and absorption. The last thing to adjust is the gain, which changes the overall brightness of the screen (Fig. 1.3).
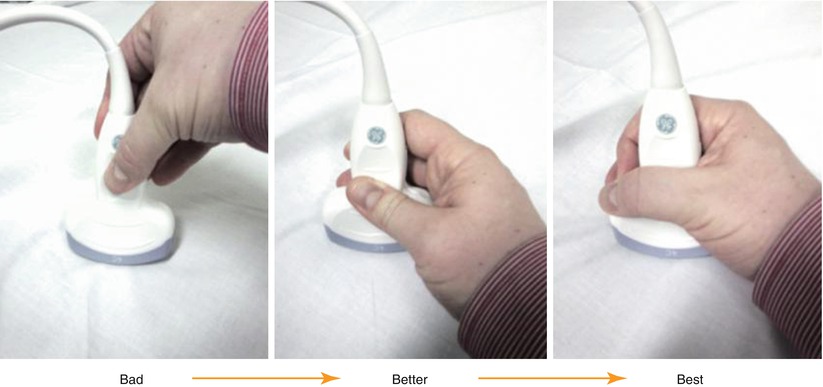
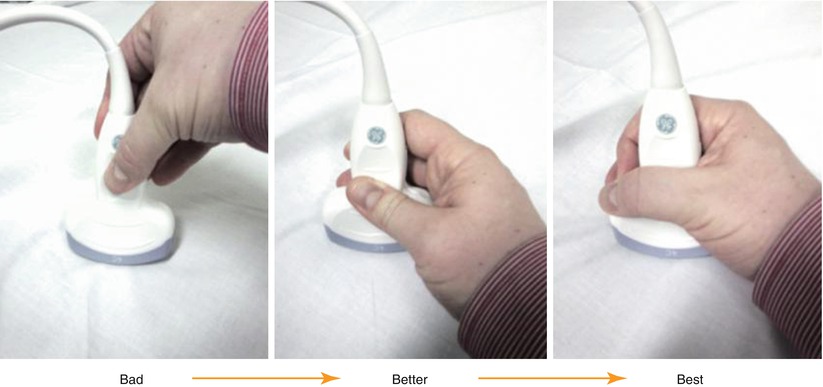
Fig. 1.3
Hold the transducer firmly while bracing the pinky or ulnar side of the hand on the patient for added control
Doppler mode can be used to identify flow. This is helpful in identifying blood vessels but can also be used to detect needle movements or small amounts of injectate, improving needle localization in difficult cases. Color Doppler shows directional flow, but Power Doppler is more sensitive for picking up movement.
Tissue Characteristics
Table 1.2
General ultrasound terms
Echogenicity – the capacity of a structure in the path of an ultrasound beam to reflect back sound waves | |||
 | |||
Anechoic | Isoechoic | Hypoechoic
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |





