Despite marked advances in limiting image times for magnetic resonance imaging, CT remains the primary modality for most indications for imaging the abdomen and pelvis. The technology of multidetector CT (MDCT) scanners continues to advance, with progressive increases in the number of detectors, now exceeding 128 detector rows, and progressive decrease in acquisition times. Concern is now focused on CT radiation dose and overuse as thin-slice rapid scanning during multiple phases of contrast enhancement has rapidly expanded the indications for body CT. Isotropic voxel scanning allows CT data obtained in the axial plane to be reconstructed with the same resolution in any plane. (An isotropic voxel is of the same size in all directions.) Coronal, sagittal, and oblique plane reconstructions have become routine. CT angiography, enterography, and colonography are commonly used.
Evaluation of the abdomen and pelvis by CT requires greater attention to patient preparation, technique, and individualization than CT evaluation of any other area of the body. The best quality studies are produced when the radiologist evaluates the patient clinically, assesses the nature of the imaging problem, and tailors the study to optimize the information that the examination provides.
Technical Considerations
When a request is presented for an abdomen-pelvis CT scan, the radiologist should assess the clinical problem to be evaluated by reviewing the available patient history and all pertinent available previous imaging studies. Medical history of importance to CT examination includes the current indication for the study, the risk of administering contrast agents, including history of allergic reactions or impaired renal function, the presence of cardiac or other diseases, past abdominal surgical procedures, history of malignancies and radiation therapy, and the findings and availability of previous imaging studies performed elsewhere. Previous imaging studies are reviewed to ensure that all previously identified abnormalities and questionable findings are appropriately reevaluated.
Decisions to be made to individualize the examination include:
- •
Area scanned: anatomic landmarks and scan extent.
- •
Radiation dose (tube current, peak tube potential), pitch, scan speed, rotation time specific to the size of the patient. Specific pediatric protocols should be used.
- •
Beam collimation (detector width and number of detector rows).
- •
Type and concentration of contrast agent to be administered: intravenous, oral, rectal, or intracavitary.
- •
Intravenous contrast agent concentration, administration rates, method of administration, and scan timing for arteriography and venography, or for arterial phase, venous phase, and delayed phase enhancement of solid organs and tissues.
- •
Slice thickness, reconstruction intervals, reconstruction planes, and three-dimensional image reconstructions.
Most institutions have developed standard protocols for a variety of indications, which depend in part on the scanner manufacturer and the number of detector rows. These may be modified as needed to appropriately address the patient problem.
Gastrointestinal Contrast Agents
Nearly all CT scans of the abdomen require the administration of intraluminal contrast agents to demonstrate the lumen of and to distend the gastrointestinal tract. Radiopaque agents may be dilute concentrations of barium or iodinated contrast agents. Iodinated agent concentrations of 1% to 3% are optimal for intraluminal opacification for CT, as compared with the 30% to 60% solutions used for fluoroscopy. Barium mixtures and water-soluble iodinated agents are equally effective as opaque oral contrast agents.
Air and water are excellent as low-attenuation contrast agents. Carbon dioxide is preferred for instillation into the rectum to insufflate the colon for CT colonography. Effervescent crystals with a small volume of water may be given orally to distend the stomach with gas. Water serves as an excellent low-density contrast agent for the upper gastrointestinal tract. Urine in the distended bladder provides excellent contrast for bladder lesions. Patient preparation may include having the patient avoid urination or clamping an indwelling Foley catheter. Low-attenuation barium-based contrast agents are used for CT enterography.
Intravenous Contrast Agents
Intravenous contrast agents improve the quality of abdominal CT by opacifying blood vessels, increasing the CT attenuation of abdominal organs, confirming perfusion, and increasing image contrast between lesions and normal structures. MDCT allows multiphase imaging to demonstrate the passage of contrast agent through the arterial system, organs and tumors, and the venous system. Delayed images show contrast agent excretion by the kidneys, late enhancement, or prolonged retention of intravenous contrast agent in organs and lesions. For most applications, intravenous contrast agents are administered by power injectors that provide accurate control of the rate and volume of administration.
Low-osmolarity “nonionic” iodine-based agents are the intravenous contrast agents of choice for most abdominal scanning because of their lower rate of adverse reactions. Sterile iodinated contrast agents approved for intravenous injection can be injected into indwelling catheters, drainage tubes, sinus tracts, and fistulas to evaluate the extent of disease. For intravenous administration, iodine concentrations of 60% and 75% are most commonly used. Older ionic contrast agents of higher osmolality are no longer used for intravascular injection because of significantly higher rates of adverse reactions. However, these cheaper ionic agents may be used for intracavitary injection, where adverse reactions are rare. For injection into the bladder for CT cystography, or through indwelling catheters for demonstration of fistulas, sinus tracts, or abscess cavities, the contrast agent is usually diluted to an iodine concentration of 2% to 3%.
Although detailed review of adverse reactions and safe use of intravenous contrast agent is beyond the scope of this text, patient safety is always the first priority. Adverse reactions associated with intravenous contrast agent administration include anaphylaxis, cardiac and respiratory arrest, nephrotoxicity, and hives. The reader is referred to the Suggested Reading section for several excellent reviews on safe use of iodinated intravenous contrast agents.
How to Interpret CT Scans of the Abdomen and Pelvis
When one is just beginning to learn to interpret body CT scans, it is very useful to develop a checklist to ensure that all structures are inspected and that all key observations are noted to make accurate and comprehensive diagnoses. A system of structured reporting or dictation templates aids in ensuring complete review of all elements of the study.
Because of the dramatic increase in the number of images obtained by MDCT, image viewing is best performed on a computer workstation using the reconstructed digital images obtained directly from the CT scanner. Image display workstations allow rapid scrolling through serial images, the ability to conveniently change window level and window width settings, and the ability to perform rapid image reformatting in multiple anatomic planes and with three-dimensional techniques.
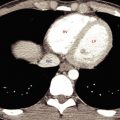
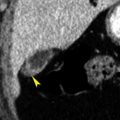
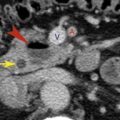
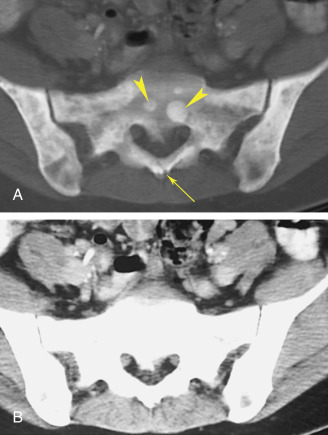
Each CT image of the abdomen contains much more information than can be displayed by any one window width and level setting. Routine “soft-tissue” windows (window width ∼400 Hounsfield units [HU]; window level 30–50 HU) define most abdominal anatomy. However, the liver may also be inspected using narrower “liver windows” (window width ∼100–150 HU; window level 70–80 HU) to increase image contrast within the liver and improve visibility of subtle lesions. The lung bases are included on scans through the upper abdomen and should be inspected using “lung windows” (window width 1000–2000 HU; window level 600–700 HU). Lung windows are also used to detect free intraperitoneal air and gas collections. Lastly, inspection of the bones using “bone windows” (window width ∼2000 HU; window level ∼600 HU) may yield important clues to pathologic findings within the abdomen and pelvis ( Fig. 8.1 ).
Each organ and structure should be systematically examined on serial images obtained through all phases of the CT examination. No interpretation will be accurate without consideration of the “phase” of contrast enhancement (arterial, venous, cortical, nephrogram, delayed, etc.).
- •
Lung bases: nodules, infiltrates, scars, pleural effusions, atelectasis
- •
Liver: size, homogeneous parenchymal attenuation, uniform enhancement, portal veins, hepatic veins, hepatic arteries, lesions cystic or solid, enhancement of lesions
- •
Biliary tree and gallbladder: visible bile ducts, wall thickness, presence and distention of the gallbladder, low density stones, high density stones
- •
Spleen: size (normal up to 14 cm), inhomogeneous enhancement early, homogeneous enhancement late, splenules, splenic vein, splenic artery
- •
Adrenals: Y or V shape, limb thickness less than 1 cm, no convex margins
- •
Pancreas: size and position, head, neck, body, tail, size of the pancreatic duct, patent splenic vein, lucent peri-pancreatic fat
- •
Kidneys: normal length 9-13 cm in adults, symmetric enhancement, calyces and pelvis and ureter, position and orientation
- •
Lymph nodes: retroperitoneum, mesentery, omentum, porta hepatis, pelvis
- •
Blood vessels: aorta, inferior vena cava, celiac axis and branches, superior and inferior mesenteric arteries, renal arteries, renal veins, splenic vein, superior mesenteric vein, portal vein
- •
Stomach: position, distention, contents, wall thickness, fold thickness
- •
Duodenum and small bowel: position, distention, wall thickness, surrounding fat, mesentery
- •
Colon and rectum: position, distention, wall thickness, luminal contents, diverticula
- •
Uterus and ovaries: size, position, endometrium, follicles, assess appropriateness for the patient’s age and phase of the menstrual cycle, uterine and adnexal masses
- •
Prostate and seminal vesicles: size, contour, definition, calcifications
- •
Bladder: distension, wall thickness, luminal contents
- •
Bones: degenerative changes, metastatic disease, mineralization
After diligent use of a checklist, detailed inspection of the images becomes automatic and familiar. Remember that you “see” what you look for and that it is hardest to “see” what is not there: absent gallbladder, ectopic kidney, etc.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree