Chapter 31 Investigations of the genitourinary tract
As outlined in Chapter 28, contrast-enhanced imaging of the urinary tract was originally developed in the early 1920s, when suitable contrast agents were first used. For the most part of the 20th century contrast conventional radiography was the only option for imaging of the tract, but all complementary imaging methods, and especially ultrasound, now offer a significant contribution to imaging the area.
The advent of low radiation dose computed tomography (CT) of kidneys, ureters, bladder (KUB) has now moved towards extra-low dose CT KUB (equivalent dose to a plain radiography KUB exposure), making CT a suitable option in this area.1 Comparison has been made between ultra-low dose (contrast-enhanced) CT and KUB (particularly relating to renal colic assessment), finding CT to be comparable in diagnostic yield to KUB.2 MRI also has a place in imaging the urinaryly system, thanks to its superior ability to demonstrate differences in soft tissue appearances. There is additional information on imaging methods for the urinary system at the end of the section on the urinary tract below.
As a result of these developments in imaging, the use of intravenous urography (IVU) has slowly receded since the 1980s, mainly because of the increased availability and use of ultrasound. However, it may still be used in some centres, in emergency cases, or where there may still be difficulties using or accessing other imaging modalities (more specifically CT). According to the Royal College of Radiologists (RCR), the unavailability of CT is the only reason for performing an IVU.3
Common pathologies and clinical indications for imaging of the Urinary System
This is not an exhaustive list and any suggested imaging methods are based on current UK guidelines.3
Calculus/calculi
Renal calculi are formed in the urine and create problems for patients when they lodge in the urinary tract, causing severe pain (renal colic) and, potentially, ureteric obstruction, hydronephrosis and haematuria. Stones as small as 0.4 cm can cause renal colic. The constituents of calculi vary, but the most common are calcium oxalate and calcium phosphate; they are often radio-opaque (but can also be radiolucent and not visible via X-ray imaging) and can therefore be visualised on the plain radiographic image. However, owing to their (usually) small size they may not always be well visualised; this is also complicated by the surrounding (possible superimposition of) soft tissue structures of the abdominal viscera, and also mesenteric nodes and phleboliths. This obviously means that plain radiographic imaging of the abdomen, albeit a reasonable tool for imaging renal stones, is not as useful to determine ureteric stones and their position. Current UK guidelines suggest unenhanced low-dose CT as the investigation of choice, with IVU indicated only when CT is unavailable.3
Large radio-opaque calculi may occupy the space within the pelvicalyceal system, filling it in almost exactly the same shape as the system; these are known as staghorn calculi (Fig. 31.1) and can mimic the appearance of a contrast-filled pelvicalyceal system. They can be an incidental finding seen on abdomen images.
Benign and malignant prostatic disease
Although the prostate gland is not located within the urinary tract itself, prostatic disease affects urinary tract imaging by its extrinsic effects on the system. A large proportion of men from late middle age onwards will have an enlarged prostate due to benign prostatic hypertrophy/hyperplasia (BPH).4 Symptoms of this include frequency of micturition, poor urine stream and dysuria. Extreme forms can cause bladder outlet obstruction. Although a benign condition, BPH will often require treatment in order to alleviate its symptoms, as they often significantly affect the patient’s quality of life. It is important to differentiate between BPH and carcinoma of the prostate, which can cause similar symptoms.
If the urinary tract contains contrast agent, if prostatic enlargement of any type is present the bladder appears to have a depression at its base, in the shape of a mushroom. Bladder ultrasound with measurement of postvoid residual volume is the examination of choice when investigating BPH and the extent of its effect, and contrast radiography is not indicated for this condition.3 Ultrasound will help differentiate between BPH and prostatic carcinoma and is usually used in conjunction with assessment of blood levels of prostate-specific antigen (PSA); an elevated PSA level may indicate malignancy.
Commonly encountered malignant tumours
The most common type affecting the intrinsic system is transitional cell carcinoma, and the most common location is the bladder. A common method of imaging assessment for bladder malignancy is ultrasound; however, cystoscopy is considered to be the optimum method. Epithelial cell tumours also affect the renal tract and are best demonstrated by contrast-enhanced CT. At one time the IVU was considered to be superior to CT for demonstration of these tumours but advances in multislice CT technology led to a change in opinion.5
For the diagnosis of suspected renal cell adenocarcinoma or transitional cell carcinoma, the optimal methods of imaging have long been considered to be ultrasound or CT; however, MRI is now known to be sensitive and is being used increasingly, especially if contrast administration is contraindicated.3
Duplex system
This is a duplication of part or parts of the urinary system involving the kidney and ureter. The most extensive form presents as a single kidney which has two sets of calyces, two renal pelves and two ureters (Fig. 31.2); this may be unilateral or bilateral. Less extensive forms of the variant may show as two renal pelves entering a single ureter, or two pelves entering two ureters, which later fuse before entering the bladder. The variant is usually an incidental finding but is monitored in children because of its relationship to recurrent urinary tract infection (UTI).
Horseshoe kidney
A relatively rare variant. The two kidneys are joined at their upper or lower poles, the latter being by far the most common. Each kidney has its own ureter, and if the kidneys are joined at their lower pole X-ray contrast images show the calyces appearing similar to those in a ‘normal’ kidney which has been placed in an oblique position (Fig. 31.3). In these cases the ureters cannot leave the kidney pelvis and hilum medially as in the normal kidney, and travel forward and over the adjoined lower poles. Ultrasound, CT and MRI will also identify this variant.
‘Reflux’ and pyelonephritis
More specifically known as ureteric or vesicoureteric reflux and reflux nephropathy; it commonly affects children. Urine flows backwards from the bladder owing to failure of the vesicoureteric valve. Reflux, in these cases, refers to backtracking of urine from the bladder into the ureter and upwards towards the kidney. This can lead to pyelonephritis, renal dysfunction and scarring, and in chronic cases renal failure. Vesicoureteric reflux can be assessed using micturating cystography and radionuclide imaging (RNI), which provides a non-invasive approach to diagnosis.6,7
Urinary tract obstruction
This can be due to a number of causes, either intrinsic or extrinsic. Obstruction affects the tract’s ability to drain, potentially causing hydronephrosis, kidney enlargement and loss of renal cortex. If obstruction is caused by a calculus, unenhanced low-dose CT is the imaging modality of choice. Contrast-enhanced CT (CT urogram), ultrasound, Doppler ultrasound, RNI and MRI all have a place if considering intrarenal blood flow, renal function, or assessment of patients who are not suitable for administration of intravenous contrast agent. IVU is not recommended unless CT is unavailable.3
Renal transplant
Transplant patients will have one functioning kidney: the transplanted one, attached to a short ureter and placed in the right iliac fossa. The current recommendations for assessment of transplanted kidneys are for Doppler ultrasound with the use of RNI (can distinguish acute rejection) or MR/MRA (if ultrasound is equivocal).3
Radiographic examination of the urinary system
Intravenous urography (IVU)
• Cross-renal, collimated to the kidneys and upper ureters
• Bladder anteroposterior (AP) with caudal angle of approximately 15° to clear the bladder from the upper border of symphysis pubis
Contrast agent can be seen almost immediately after injection, shown as a ‘blush’ in the renal cortex and known as a nephrogram (Fig. 31.4). This shows glomerular filtration of the contrast agent before it reaches the calyceal systems. It is important to see the renal outlines, as changes in the smooth outline may indicate the presence of tumours, cysts or cortical scarring. It also provides early information on renal size. It is possible to see appearances of renal blush for some time after injection and it is not always considered necessary to show the first blush immediately after injection of contrast agent, as renal outlines can be assessed along with the calyceal systems at later stages in the examination.
Around 5 minutes after injection the calyces should be seen to fill with contrast agent (Fig. 31.5), which then passes down the ureters to fill the bladder. In some cases the calyces empty quickly, preventing adequate demonstration of the calyces and renal pelvis. To counteract this, compression over the abdominal area level with the iliac crests is required, which restricts the flow of excreted contrast down the ureters. This therefore retains contrast agent in the kidney for a longer period to ensure adequate imaging of the collecting systems. Compression is usually left in place for around 5 minutes before an image of the kidneys is taken, but it must be noted that excessive and prolonged compression may cause the calyces to appear slightly blunted and distended (imitating early hydronephrosis). It is recognised that compression is often applied routinely, often 5 minutes after injection, to ensure optimal contrast build-up in the calyces, but there are contraindications to the use of compression that must be considered. These include:
• images in the opposite phase of suspended respiration to potentially change the position of overlying appearances such as bowel gas, faeces or radio-opacities
• zonography to clear images of bowel gas and faeces
• tomography to provide more detailed information after calyceal and renal pelvis images suggest or cannot exclude filling defects.
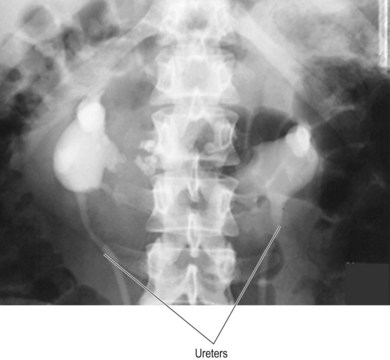
Once the calyceal system has been demonstrated it is necessary to provide information on the ureters and bladder; evidence of ureteric drainage is especially important. A KUB projection (around 15–20 minutes after injection) will show most of the tract, including some early bladder information (Fig. 31.6). If the use of compression has been necessary it must be released before this KUB can be taken, in order to allow kidney drainage. Compression release usually allows for good visualisation of ureteric drainage, as the contrast-enhanced urine flows down the ureter. Some sections of the ureters may not be visible on the KUB, owing to the fact that urine is transported down these structures by peristalsis and portions of the ureters will be constricted; these portions will not be visible on the image. This in itself does not really pose a problem: if the ureter is obstructed then there should be other evidence to suggest this, including distended or blunted calyces, hydronephrosis (seen initially as delayed concentration of contrast agent and later as distended and club-shaped calyces), distended ureters (or even megaureter) and failure of contrast to pass the obstructed area on prone KUB or oblique bladder images. The prone KUB is particularly useful to show the ureteric obstruction site: the kidneys lie posteriorly in the retroperitoneal abdomen and the ureters extend from the kidneys anteriorly until they are approximately level with L4/L5 and then towards the bladder, which is situated anteriorly in the pelvis. Therefore, in the supine patient urine is moving in an upward direction for the first section of the ureter; turning the patient prone after sitting them upright for 5 minutes reverses this and allows the urine to drain towards the site of obstruction.
Series of projections for the IVU
Texts describing excretion urography do vary on the suggested standard or routine ‘protocol’ for the examination,7–10 but it must be accepted that owing to the decline in its use as a front-line examination a ‘conventional’ IVU series is no longer a valid concept. Providing a useful IVU series must be governed by the need to keep radiation dose to the patient as low as is reasonably practical, as stated in current regulations and guidelines,3,11–13 and the need to use a series that will provide the best possible diagnostic images for each patient and their clinical history (or the appearances found as the examination progresses).
1 Control KUB on inspiration for assessment of gross anatomy and presence of obvious pathology such as radio-opaque calculi
2 Position the patient for a cross-renal image
3 Injection of the contrast agent
4 Cross-renal 5 minutes after injection, to assess renal outlines and calyces and taken on arrested expiration. If calyces are not well demonstrated, apply compression if this is not contraindicated, and repeat the cross-renal 5 minutes later. If there is suspected pathology, or gas or faeces impair detail, undertake zonography or tomography of the renal area. Fulcrum heights selected for this will vary according to patient build, but three ‘cuts’ are usually taken from a range between 7 and 11 cm
5 If compression has not been applied, 15–20 minute KUB with contrast, taken on inspiration. If compression has been applied, release compression and undertake KUB after calyces have been adequately demonstrated
6 Collimated AP 15° caudal angle bladder image, taken after micturition
Hydronephrosis (Fig. 31.7)
This may be known to pre-exist or may manifest itself during the examination as:
• Failure to demonstrate the calyces (especially easy to note when one kidney appears normal in comparison to a non-apparent kidney on the other side in the early stages of the examination). This is due to excessive urine, which dilutes the contrast agent, remaining in the kidney. Often there is concentration of the contrast agent later in the examination, but sometimes not for several hours. The cause of the hydronephrosis is impairment or obstruction of drainage at some point, from the pelviureteric junction down to the bladder, usually due to calculus or tumour. It can also be caused by bladder outlet obstruction
• Blunted and distended calyces
• Chronic hydronephrosis is likely to be accompanied by loss of renal cortex