• This involves the selective injection of contrast medium into the right and left coronary arteries and the left ventricle (while recording the resultant moving images) • A percutaneous femoral arterial catheterization is the usual approach (an alternative percutaneous route is the radial artery) • The severity and length of a stenosis • Poor ventricular function is associated with an increased risk, but a greater potential benefit (the prognosis is related to the degree of ventricular dysfunction) • High-risk patients with unstable angina or non-ST elevation myocardial infarction may benefit from early angioplasty or stenting • Demonstration of the effects of IHD on ventricular function • Detecting structural complications such as a VSD, papillary muscle dysfunction (causing mitral regurgitation) and ventricular thrombus • Demonstrating the origins of the main coronary arteries (especially with transoesophageal echocardiography) • This detects reversible wall motion abnormalities (indicating reversible ischaemia) using the same stimulants as for CT or MR stress imaging • It enables risk stratification for patients with known or suspected IHD (a normal study indicates a very good prognosis) • It enables preoperative risk assessment (this determines myocardial viability) • It is more sensitive for detecting ischaemia than a conventional ECG-based exercise test • Factors affecting the accuracy of the technique: the threshold for defining a significant stenosis Complications of cardiac angiography* ACC/AHA guidelines for coronary angiography* • Severe resting left ventricular dysfunction (LVEF <35%) • MDCTA can detect significant (>50%) stenoses with a 90% sensitivity and specificity (if there is not significant calcification) • Images are obtained at end diastole • Evaluation of aortic and other vascular disease as well as some structural cardiac abnormalities (such as pericardial constriction, tumours and thrombus) • Evaluation of arterial and venous great vessel anatomy • Evaluation of cardiac dimensions (there are limitations imposed by the need for iodinated contrast medium and the radiation exposure) • Assessment of myocardial viability and perfusion – images can be analysed in a similar manner to that with MR perfusion imaging • Assessment of resting myocardial perfusion, which can be used to evaluate the size of an acute myocardial infarction and recovery following reperfusion • It is able to accurately determine CABG patency and may be able to determine the patency of the infarct-related artery after coronary thrombolysis • Multiphase reconstruction provides cine images of ventricular and valve movement Radiation dose from cardiac imaging studies compared with other imaging studies* • ‘Black blood’ imaging: the myocardium and vascular wall appear bright and the blood dark • A 180° inverting pulse is applied to the whole imaging volume followed by a slice selective 180° ‘de-inversion’ pulse: the net result is inverted spins outside of the imaged slice but the spins within the imaged slice are unchanged (they have experienced both inversion and de-inversion) • ‘White blood’ imaging: blood produces a higher SI than that seen with spin-echo sequences • This is because only one radiofrequency pulse is used and there is less time for the blood to move out of the imaging plane between slice selection and image acquisition (turbulent blood flow will produce areas of signal loss) • The gradient-echo sequence can be repeated more rapidly with a reduced RF flip angle, allowing the acquisition of cine loops • This allows quantification of flow velocities • Positive velocity encoding: if a gradient is applied in the direction of blood flow for a finite time and then turned off, the relationship of phase will change in relation to the two ends of the gradient (the protons at the stronger end of the gradient precess at a faster rate during its application than those at the weaker end) • Negative velocity encoding: when the gradient is turned off, the rate of precession becomes constant again in the slice, but the phase relationship has changed and the phase signature remains
Ischaemic heart disease
CONVENTIONAL CORONARY ANGIOGRAPHY AND ECHOCARDIOGRAPHY
CONVENTIONAL CORONARY ANGIOGRAPHY
Technique
 at least 3 shaped catheters are required – one for each coronary artery and one for the left ventricle)
at least 3 shaped catheters are required – one for each coronary artery and one for the left ventricle)  low osmolality contrast media is used with rapid filming at 25+ frames/s
low osmolality contrast media is used with rapid filming at 25+ frames/s  images are acquired in multiple orientations with very short exposures (5–10 ms) to freeze cardiac motion
images are acquired in multiple orientations with very short exposures (5–10 ms) to freeze cardiac motion
Considerations during coronary angiography
 the presence of a complete occlusion (± collateral vessels)
the presence of a complete occlusion (± collateral vessels)  the number of affected vessels
the number of affected vessels  the vessel diameter and stenosis configuration
the vessel diameter and stenosis configuration
 Significant (>50% diameter reduction) accessible stenoses in 1 or 2 vessels (with a diameter > 2mm) are treated by angioplasty or stenting
Significant (>50% diameter reduction) accessible stenoses in 1 or 2 vessels (with a diameter > 2mm) are treated by angioplasty or stenting
 Left main coronary artery disease or significant disease affecting all 3 coronary arteries is usually best treated with a CABG
Left main coronary artery disease or significant disease affecting all 3 coronary arteries is usually best treated with a CABG
ECHOCARDIOGRAPHY
Indications
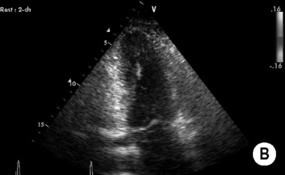
 A large infarct will appear hypoechoic, whereas fibrotic scar tissue is stiffer than normal myocardium and appears hyperechoic
A large infarct will appear hypoechoic, whereas fibrotic scar tissue is stiffer than normal myocardium and appears hyperechoic
 demonstrating any anomalous origins and coronary artery aneurysms (e.g. Kawasaki’s disease)
demonstrating any anomalous origins and coronary artery aneurysms (e.g. Kawasaki’s disease)
Stress echocardiography
 the endpoint of the test is the appearance of new wall motion abnormalities (chronic ischaemia causes diffuse dysfunction, an acute myocardial infarction causes more localized changes)
the endpoint of the test is the appearance of new wall motion abnormalities (chronic ischaemia causes diffuse dysfunction, an acute myocardial infarction causes more localized changes)
 whether there is single or multivessel disease
whether there is single or multivessel disease  whether an adequate stress is achieved (especially for exercise-based protocols)
whether an adequate stress is achieved (especially for exercise-based protocols)  the presence of other disease processes which affect myocardial function (such as cardiomyopathy, microvascular disease, or hypertrophy)
the presence of other disease processes which affect myocardial function (such as cardiomyopathy, microvascular disease, or hypertrophy)
Vascular
Haematoma
False aneurysm
Arteriovenous fistula
Mycotic aneurysm
Retroperitoneal haematoma
Acute occlusion
Arterial dissection
Cardiac
Arrhythmias (catheter manipulation)
Myocardial infarction
Coronary dissection
Systemic embolus (including stroke)
Myocardial perforation
Contrast medium
Heart failure (reduced with low-osmolality contrast agent)
Arrhythmias (sinus bradycardia, sinus arrest, ventricular fibrillation in 0.1-1.0%)
ECG changes (wide QRS, long QT, ST changes, change in QRS axis)
Hypotension (reduced with low-osmolality contrast agent)
Allergic/idiosyncratic (reduced with non-ionic contrast agent)
Renal impairment (possibly reduced with low-osmolality contrast agent)
• High-risk treadmill score (score ≥ 11)
• Severe exercise left ventricular dysfunction (exercise LVEF <35%)
• Stress-induced large perfusion defect (particularly if anterior)
• Stress-induced moderate size multiple perfusion defects
• Large, fixed perfused defect with left ventricular dilatation or increased lung uptake (201TI)
• Stress-induced moderate size perfusion defect with left ventricular dilatation or increased lung uptake (201TI)
• Echocardiographic wall motion abnormality (involving more than two segments) developing at a low dose of dobutamine or at a low heart rate
• Stress echocardiography evidence of extensive ischaemia
CT IMAGING IN ISCHAEMIC HEART DISEASE
CARDIAC CT AND CT ANGIOGRAPHY (CTA)
CORONARY CTA
 it can reliably demonstrate normal coronary arteries and detect stenoses with a high positive (90%) and negative (95%) predictive value
it can reliably demonstrate normal coronary arteries and detect stenoses with a high positive (90%) and negative (95%) predictive value  it allows reliable identification of patients who do not need coronary angiography
it allows reliable identification of patients who do not need coronary angiography  in addition (in up to 10% of cases) MDCT can detect significant non-cardiac diagnoses (e.g. pneumonia or pneumothorax)
in addition (in up to 10% of cases) MDCT can detect significant non-cardiac diagnoses (e.g. pneumonia or pneumothorax)
 there are limitations related to heavy arterial calcification and imaging vessels < 2mm in diameter
there are limitations related to heavy arterial calcification and imaging vessels < 2mm in diameter  accurate imaging requires a slow enough heart rate (<70 beats/min) and good breath holding (at least 10s)
accurate imaging requires a slow enough heart rate (<70 beats/min) and good breath holding (at least 10s)
OTHER CARDIAC CT INDICATIONS
Procedure
Effective dose (mSv)
Yearly background radiation
3.6
Chest radiograph
0.032–0.1
Skull examination
0.15
Lumbar spine series
3
Bone scintigram
4.4
Coronary arteriogram
2–6
EBCT calcium scoring
0.5–1
Coronary MDCTA
6–8 (constant tube current)
MR IMAGING IN ISCHAEMIC HEART DISEASE
CARDIAC MRI (CMR) AND MR ANGIOGRAPHY (MRA)
Types of imaging
Spin-echo imaging
 this is useful for high-definition anatomical imaging of the heart and vessels but is rather slow to perform
this is useful for high-definition anatomical imaging of the heart and vessels but is rather slow to perform
 the time at which this is applied is the time at which the longitudinal magnetization of blood has reached zero from the initial inversion – therefore blood flowing into the slice will generate no signal (‘black blood’)
the time at which this is applied is the time at which the longitudinal magnetization of blood has reached zero from the initial inversion – therefore blood flowing into the slice will generate no signal (‘black blood’)  there may be variable signal from slow or in-plane blood flow (producing artefacts)
there may be variable signal from slow or in-plane blood flow (producing artefacts)
Gradient-echo imaging
 this also allows quantification of ventricular stroke volumes (comparing end-systolic and end-diastolic volumes)
this also allows quantification of ventricular stroke volumes (comparing end-systolic and end-diastolic volumes)
Phase shift velocity mapping
 when the gradient is reversed and applied for the same period of time as the original gradient, the phase signature of still material is cancelled, but flowing blood moving during the gradients to a different phase territory retains a phase change proportional to its velocity
when the gradient is reversed and applied for the same period of time as the original gradient, the phase signature of still material is cancelled, but flowing blood moving during the gradients to a different phase territory retains a phase change proportional to its velocity
Ischaemic heart disease

 transoesophageal echocardiography can also image the heart
transoesophageal echocardiography can also image the heart it improves the definition of the margins of the ventricular cavity and enhances the accuracy of echocardiography for assessing ventricular function in poor echocardiography patients
it improves the definition of the margins of the ventricular cavity and enhances the accuracy of echocardiography for assessing ventricular function in poor echocardiography patients  it can also assess myocardial perfusion
it can also assess myocardial perfusion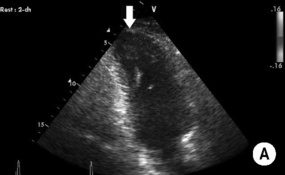
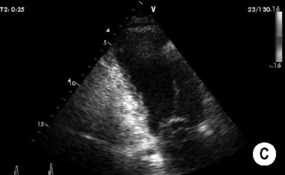
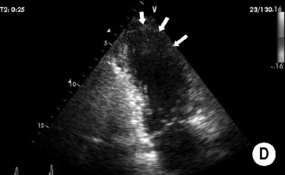
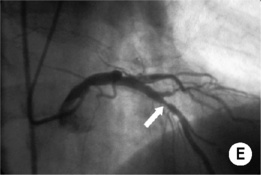
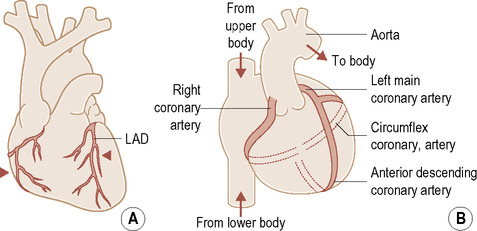
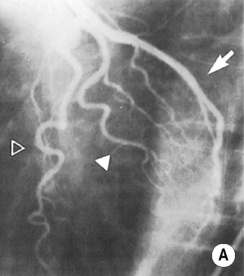
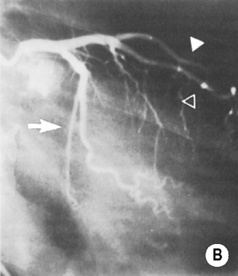
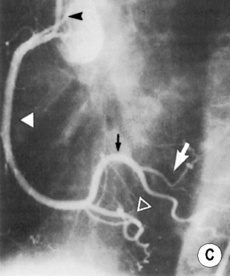
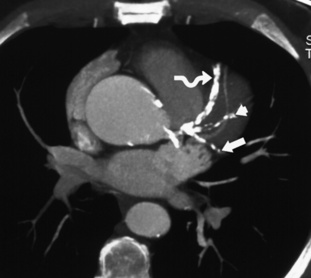
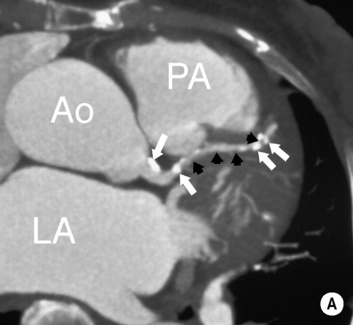
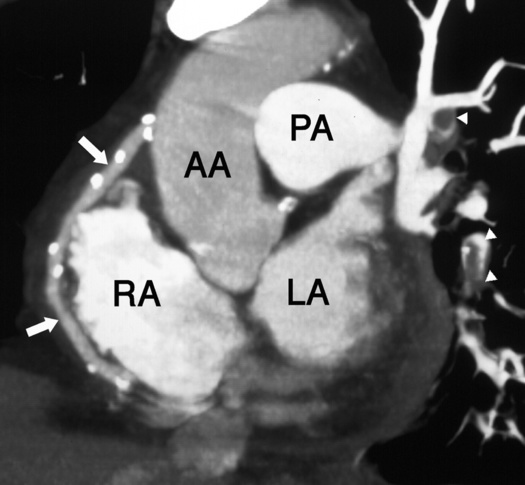
 (B) right anterior oblique (RAO) projection. Open arrowhead = left anterior descending artery (LAD), solid arrowhead = diagonal, branch arrow = circumflex/obtuse marginal vessels. In (B) the LAD and its diagonal branch overlap but the LAD may be identified by its septal branches and its extension to the apex of the heart. The small circumflex branch (arrow) has the characteristic straight appearance which suggests that it is running in the left atrioventricular (AV) groove. The larger obtuse marginal branch has left the AV groove and is running on the surface of the left ventricle. (C,D) Right coronary artery: (C) LAO projection
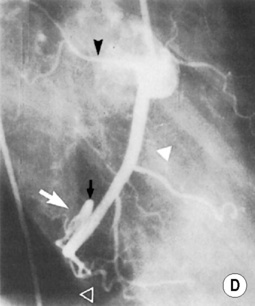
(B) right anterior oblique (RAO) projection. Open arrowhead = left anterior descending artery (LAD), solid arrowhead = diagonal, branch arrow = circumflex/obtuse marginal vessels. In (B) the LAD and its diagonal branch overlap but the LAD may be identified by its septal branches and its extension to the apex of the heart. The small circumflex branch (arrow) has the characteristic straight appearance which suggests that it is running in the left atrioventricular (AV) groove. The larger obtuse marginal branch has left the AV groove and is running on the surface of the left ventricle. (C,D) Right coronary artery: (C) LAO projection  (D) RAO projection. Solid white arrowhead = right coronary artery, open arrowhead = posterior descending coronary artery, black arrowhead = sinus node artery, black arrow = inverted U at the crux, white arrow = posterolateral left ventricular branch. In (C) the entire right coronary artery is seen in profile as it passes around the heart in the right side of the AV groove. The posterior descending branch is the last branch before the crux. Beyond the crux (marked by the inverted U) are posterolateral left ventricular branches supplying the free wall of the left ventricle. In (D) both the origin and the terminal part of the right coronary artery are foreshortened but the sinus node artery (black arrowhead) can be distinguished from the conus and other right ventricular (RV) branches. As seen in (D) it runs posteriorly to the atria, whereas the conal and RV branches run anteriorly to the right ventricle.*
(D) RAO projection. Solid white arrowhead = right coronary artery, open arrowhead = posterior descending coronary artery, black arrowhead = sinus node artery, black arrow = inverted U at the crux, white arrow = posterolateral left ventricular branch. In (C) the entire right coronary artery is seen in profile as it passes around the heart in the right side of the AV groove. The posterior descending branch is the last branch before the crux. Beyond the crux (marked by the inverted U) are posterolateral left ventricular branches supplying the free wall of the left ventricle. In (D) both the origin and the terminal part of the right coronary artery are foreshortened but the sinus node artery (black arrowhead) can be distinguished from the conus and other right ventricular (RV) branches. As seen in (D) it runs posteriorly to the atria, whereas the conal and RV branches run anteriorly to the right ventricle.* images are usually obtained at end diastole (at the point of least movement artefact)
images are usually obtained at end diastole (at the point of least movement artefact)  there is a significant associated radiation burden (although tube current modulation can nearly halve the dose)
there is a significant associated radiation burden (although tube current modulation can nearly halve the dose) acquisition times are still longer than with EBCT, but they do provide better spatial resolution
acquisition times are still longer than with EBCT, but they do provide better spatial resolution the typical volume of contrast ranges from 50 to 120ml with an injection rate of 4–7ml/s
the typical volume of contrast ranges from 50 to 120ml with an injection rate of 4–7ml/s a curved MPR can follow any tortuous anatomy
a curved MPR can follow any tortuous anatomy an imaginary source of illumination is used to provide 3D perspective
an imaginary source of illumination is used to provide 3D perspective 3D reconstructions can benefit from the removal of areas of a certain attenuation or SI (e.g. bone for CTA or fat for MRA)
3D reconstructions can benefit from the removal of areas of a certain attenuation or SI (e.g. bone for CTA or fat for MRA) tissue densities ≥ 130HU are used as an attenuation level for calcified plaque
tissue densities ≥ 130HU are used as an attenuation level for calcified plaque  alternatively, the actual volume of plaque is quantified (CVS: total calcium volume score)
alternatively, the actual volume of plaque is quantified (CVS: total calcium volume score)  some studies suggest that a high calcium score predicts an increased risk of an adverse coronary event
some studies suggest that a high calcium score predicts an increased risk of an adverse coronary event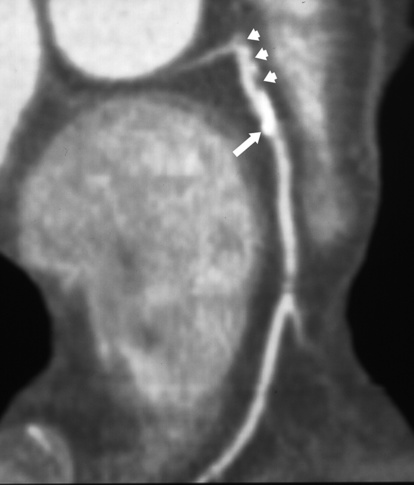
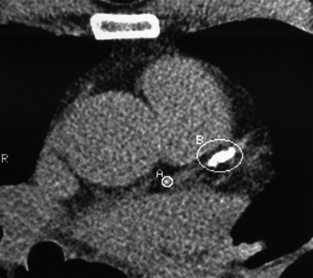
 LAD score 227).*
LAD score 227).*