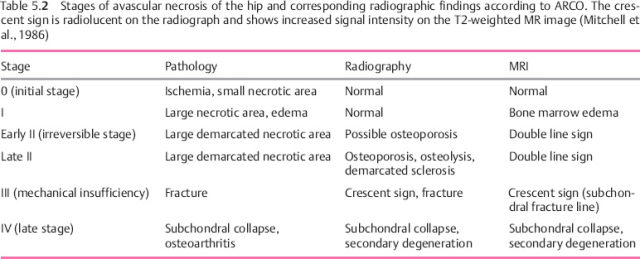
5 Ischemic Bone Disease Synonyms: avascular osteonecrosis, aseptic osteonecrosis, necrotic bone disease. Definition: Since in the area of ischemic bone disease there are many terms for the same condition, the term osteonecrosis is best defined as follows: It has become customary to apply the term osteonecrosis to ischemic injury to the epiphysis and the term bone infarct to ischemic injury to the diaphysis and metaphysis of the tubular bones. A special manifestation of ischemic bone disease primarily involves the articular cartilage: The basic aspects of ischemic bone disease, such as etiology, pathophysiology, morphology, role of the different imaging methods, and staging, will be presented by using osteonecrosis of the hip, the most common form of osteonecrosis, as an example. Synonym: avascular necrosis of the femoral head. Etiology: The conditions that cause osseous ischemia are listed in Table 5.1. Most examples of avascular necrosis of the femoral head are believed to be caused by a variety of factors, and the exact relationship between the risk factors and vascular occlusion is still controversial. Post-traumatic avascular necrosis of the femoral head (e.g., following a subcapital fracture of the femur or a hip dislocation) causes vascular disruption and acutely deficient perfusion of the femoral head. The pathophysiologic model explaining the development of necrosis of the femoral head is well described. Recurrent ischemic attacks on bone are followed by an increase in intraosseous pressure. This increased pressure is probably due to edema, since bone marrow functionally represents a closed compartment. The intraosseous capillaries and venules are compromised by this increased pressure, resulting in the vicious circle found in the ‘compartment syndrome’ of the extremities. Osseous necrosis can develop from four sources: arterial supply, venous drainage, intraluminal capillary obstruction, and compression of the capillaries and sinusoids in the marrow space (Table 5.1). Course: The ischemic necrosis passes through stages that can be quite variable in length and can last days to years (Table 5.2). The initial stage is reversible, and the necrotic area is not demarcated. Vascular insufficiency is followed by ischemia-induced bone marrow edema, which increases intraosseous pressure. An ischemic period of 12–48 hours damages the bone marrow and, subsequently, the trabecular bone. Restoration of normal blood flow can prevent progression to frank necrosis, whereas persistent vascular insufficiency leads to a demarcation of the necrosis, either through confluence of several small necrotic areas or as an innately large necrotic region. When this occurs, the irreversible stage has been reached. The subsequent course is primarily determined by the mechanical property of the necrosis, which in turn depends on the size of the necrotic area. If the necrosis is small and surrounded by buttressing reactive bone, the bone will not collapse, preventing a fracture of the subchondral plate and any intra-articular extension. A large necrotic area results in mechanical insufficiency of the osseous structure. This mechanical insufficiency begins with a subchondral fracture above the necrosis, initially with the configuration of the femoral head being maintained. The late stage is characterized by collapse of subchondral bone and articular cartilage, with subsequent degeneration that progresses to severe deformity and destruction of the joint. A special manifestation of the initial stage of necrosis of the femoral head is the bone marrow edema syndrome. Therapy: Untreated, 50% of cases develop fragmentation and destruction of the femoral head within 3 years. Early detection (with MRI) is of utmost importance since the reversible initial stage may heal with conservative therapy such as decompression. Furthermore, necrosis without fragmentation can be treated surgically with preservation of the head.
Osteonecrosis
Osteonecrosis of the Hip
 Epidemiology: The peak incidence is at 40 years of age, and bilateral involvement occurs in 30%–70% of cases.
Epidemiology: The peak incidence is at 40 years of age, and bilateral involvement occurs in 30%–70% of cases.
 The clinical findings range from no complaints (silent hip) to slight pain on weight bearing to persistent pain with inability to walk. The complaints are usually seen with ischemic attacks, osseous fragmentation, and delayed degenerative changes.
The clinical findings range from no complaints (silent hip) to slight pain on weight bearing to persistent pain with inability to walk. The complaints are usually seen with ischemic attacks, osseous fragmentation, and delayed degenerative changes.
| Affected vascular component | Etiology risk factors |
|---|---|
| Arterial | Fracture Hip dislocation Massive arterial embolism, recurrent fat embolism Vasculitis |
| Venous | Legg-Calvé-Perthes disease Massive venous thrombosis Idiopathic (?) |
| Intraosseous capillaries | Fat embolism Diabetes mellitus Vasculitis in systemic lupus erythematosus Sickle cell anemia Caisson disease (nitrogen bubbles) |
| Intraosseous vessels | Abnormal fat metabolism Hypertrophy of fatty tissue (corticosteroids, alcohol) Hyperemia Gaucher disease (glycosylceramide lipidosis) |
- < 30%, the avascular necrosis is stable,
- > 40%, the avascular necrosis has a poor prognosis, i.e., progression should be expected,
- 30%–40%, the avascular necrosis falls in the transitional range with an unpredictable outcome.
 Technical considerations: Radiographs should be obtained in the AP and lateral projections.
Technical considerations: Radiographs should be obtained in the AP and lateral projections.
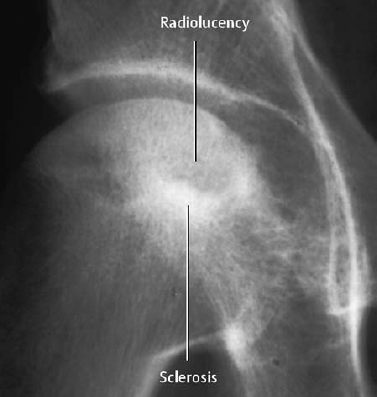
In early necrosis, a subtle osteopenia can be observed in the affected region of the femoral head (early Stage II). With progression, the necrosis appears as localized osteolysis or diffuse osteoporosis, subchondral pseudocyst, and sclerosis (Figs. 5.1–5.3). The demarcated band-like sclerosis may be variable (Stage II). Diagnostic signs of avascular necrosis of the femoral head are the subchondral location and demarcation of these changes without signs of mass effect. The radiographic signs of an advanced necrosis are subchondral fracture (Stage III), articular extension (Fig. 5.4), and secondary degenerative changes with joint space narrowing and marginal osteophyte formation (Stage IV, Table 5.2).

Fig. 5.2 Small avascular necrotic area of the femoral head with a region of subchondral sclerosis.
In Stages 0 and I (ARCO), the radiographs are normal. In Stage II, radiographic findings are present, but are often too subtle to diagnose avascular necrosis. Since a negative radiographic finding is unreliable, conventional radiography is not suitable for the detection or exclusion of early avascular necrosis of the femoral head. However, it remains the first step in the diagnostic investigation since it can establish or exclude a variety of other diagnoses.
 The three-phase bone scan with Tc 99m diphosphonate is used. Specific signs of avascular necrosis of the femoral head are decreased accumulation in the initial stage (‘cold spot’) and at a later stage increased accumulation in the reactive border zone (‘cold in hot spot’) A frequent nonspecific sign is the diffuse accumulation of activity in the femoral head as a manifestation of bone repair (Fig. 5.6). The discrete but specific (‘cold in hot spot’) scintigraphic finding of bilateral avascular necrosis of the femoral head can easily be interpreted as a false-negative finding (Fig. 5.7)
The three-phase bone scan with Tc 99m diphosphonate is used. Specific signs of avascular necrosis of the femoral head are decreased accumulation in the initial stage (‘cold spot’) and at a later stage increased accumulation in the reactive border zone (‘cold in hot spot’) A frequent nonspecific sign is the diffuse accumulation of activity in the femoral head as a manifestation of bone repair (Fig. 5.6). The discrete but specific (‘cold in hot spot’) scintigraphic finding of bilateral avascular necrosis of the femoral head can easily be interpreted as a false-negative finding (Fig. 5.7)
A diffuse accumulation of activity in the femoral head with extension into the femoral neck and intertrochanteric region most likely represents bone marrow edema syndrome.

Fig. 5.3 Avascular necrosis of the femoral head, recognized as osteolysis with a marginated sclerotic rim.

Fig. 5.4 Avascular necrosis of the femoral head with subchondral fracture (ARCO III).

Fig. 5.5 Avascular necrosis of the femoral head with mixed sclerosis and an especially pronounced region of resorption.
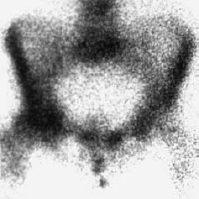
Fig. 5.6 Bone scan of an avascular necrosis with diffuse uptake on the right (nonspecific).
Fig. 5.7 Bone scan with the specific sign of a bilateral avascular necrosis of the femoral head referred to as ‘cold in hot spot’.
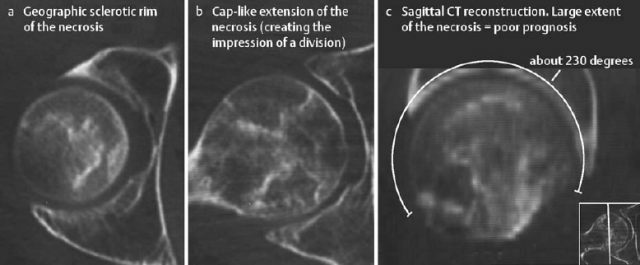
Fig. 5.8 CT of an extensive avascular necrosis of the femoral head. The reformatted image shows a large area of necrosis and implies a poor prognosis. Moreover, it precludes a displacement osteotomy.
 CT is performed with thin axial (1 – 2 mm) and coronal sections, as well as with sagittal reformations (Figs. 5.8–5.10).
CT is performed with thin axial (1 – 2 mm) and coronal sections, as well as with sagittal reformations (Figs. 5.8–5.10).
CT enables early detection of a subchondral fracture or a collapse of the articular surface – both signs of mechanical insufficiency – free of superimposed structures. With the help of 2-D reconstructions, the prognostically relevant extent of the necrosis can be accurately determined. The percentage of the affected femoral head surface can be estimated as follows:
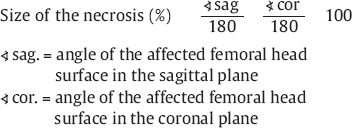
CT is the method of choice for the early detection of a subchondral fracture (Stage III). Both CT and MRI are methods of choice for surgical planning, since both enable an accurate assessment of the extent and location of the necrosis.
 For the exclusion of an avascular necrosis of the femoral head, a T2-weighted sequence with fat suppression (e.g., STIR), supplemented by a T1-weighted echo sequence, is used. MRI units designed for the simultaneous application of a body coil and a surface coil are best suited for this examination, since this allows exclusion of bilateral involvement of the femoral heads. A positive finding should be followed with a T1-weighted sequence in the sagittal plane to calculate the quantitative parameters (see CT). Contrast enhancement is not mandatory, but does permit a semi-quantitative assessment of the ongoing reparative processes.
For the exclusion of an avascular necrosis of the femoral head, a T2-weighted sequence with fat suppression (e.g., STIR), supplemented by a T1-weighted echo sequence, is used. MRI units designed for the simultaneous application of a body coil and a surface coil are best suited for this examination, since this allows exclusion of bilateral involvement of the femoral heads. A positive finding should be followed with a T1-weighted sequence in the sagittal plane to calculate the quantitative parameters (see CT). Contrast enhancement is not mandatory, but does permit a semi-quantitative assessment of the ongoing reparative processes.
The characteristic findings of avascular necrosis of the femoral head on MRI are the necrosis itself and its surrounding reparative granulation tissue (Figs. 5.11, 5.12). In (ARCO) Stage I, the necrosis exhibits a pattern of edema with low signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image. In Stage II, a signal pattern of fat or a mixed type is encountered. The fat-equivalent signal pattern consists of high signal intensity on the T1-weighted and T2-weighted images and mimics the signal intensity of healthy fatty bone marrow.
The margin of the necrotic area exhibits a typical pattern on MRI and is critical, since it allows a confident diagnosis. This is a well demarcated line of low signal intensity on the T1-weighted image, accompanied by an inner line of high signal intensity (granulation tissue) along the side of the necrosis and an outer line of low signal intensity (sclerosis, fibrosis) along the healthy bone on the T2-weighted image (= ‘double line sign’). After intravenous injection of contrast medium, the inner line shows strong enhancement (Fig. 5.11).
 MRI is indicated in all patients with clinical suspicion of an avascular necrosis of the femoral head and in patients with persistent hip pain of undetermined etiology.
MRI is indicated in all patients with clinical suspicion of an avascular necrosis of the femoral head and in patients with persistent hip pain of undetermined etiology.
MRI is the best method to distinguish avascular necrosis of the femoral head from other disorders.
MRI is the method of choice to diagnose, stage, and determine the extent of an avascular necrosis of the femoral head. The disadvantage of MRI is its limited differentiation between Stages II and III avascular necrosis of the femoral head.
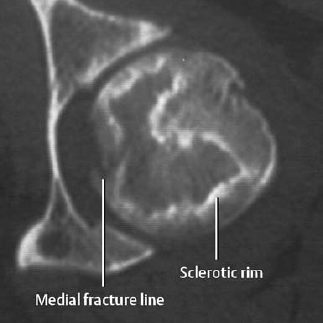

Fig. 5.10 CT of avascular necrosis of the femoral head with a multicystic or septated pseudocystic appearance and a defect in the anterior subchondral cortex.
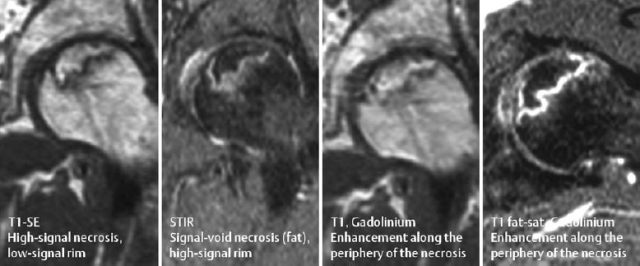
Fig. 5.11 Several MRI sequences of avascular necrosis of the femoral head. Reparative granulation tissue, which strongly enhances, is seen around the periphery of the necrosis.
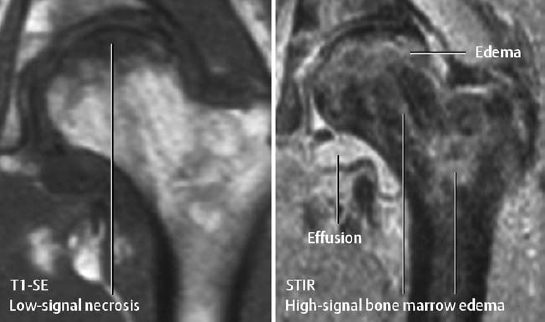
Fig. 5.12 MRI of an avascular necrosis of the femoral head with flattening of the femoral head. The STIR sequence shows the heterogeneous necrotic area and an area of increased signal intensity in the femoral neck and peritrochanteric region representing bone marrow edema.
Osteonecrosis in other Locations
Osteonecroses in other areas are less common than in the femoral head, but involvement of these locations should be considered in the presence of risk factors or a history of trauma.
The commonest other locations for osteonecrosis are the carpal bones (especially the lunate and scaphoid), the distal femur, and distal metatarsal heads. The humeral head, proximal tibia, patella, talus, and navicula of the foot are less commonly involved (Table 5.3) (Fig. 5.15). Rarely the sesamoids may also be involved (Fig. 5.18).
Osteonecroses of the major joints (knee and shoulder) show an image pattern similar to that found in the hip. The osteonecroses of the smaller bones of the hand and foot are somewhat different in imaging, therapy, and prognosis and will be described in more detail.
Osteonecrosis of the Lunate
Synonyms: Kienböck disease, lunatomalacia.
This condition occurs most often in young men involved in manual labor (e.g., pneumatic hammer operators). Another predisposing factor is the increased pressure on the lunate caused by an ulnar minus variance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Bone is an organ composed of mineralized and nonmineralized tissue. Osteonecrosis is a disease that causes bone death.
Bone is an organ composed of mineralized and nonmineralized tissue. Osteonecrosis is a disease that causes bone death.