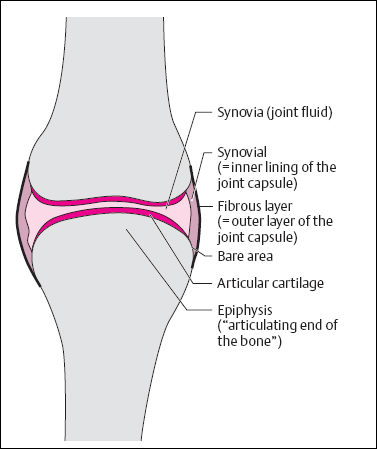
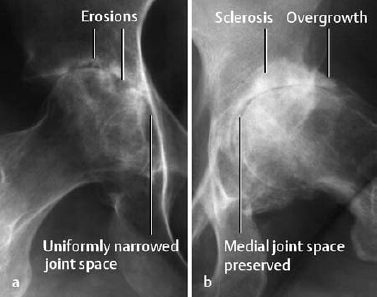
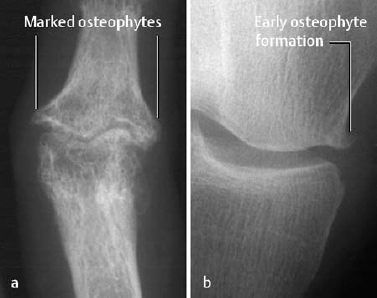
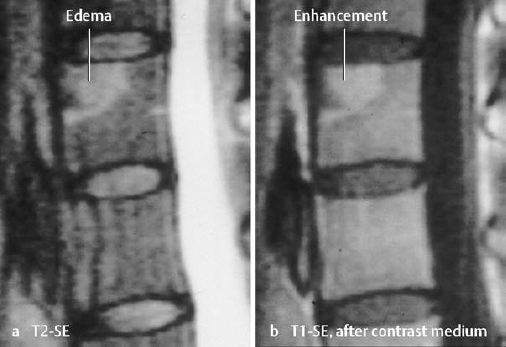
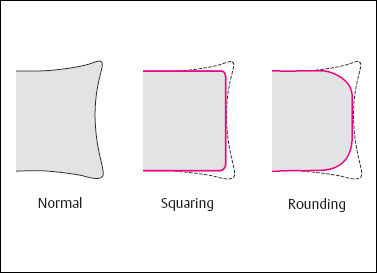
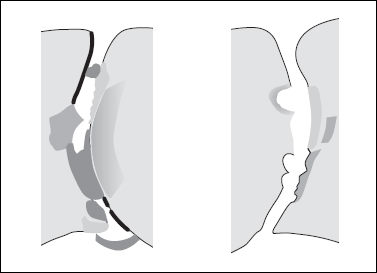
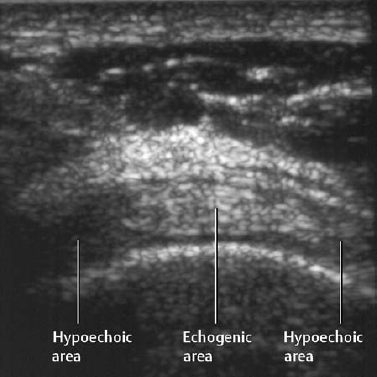
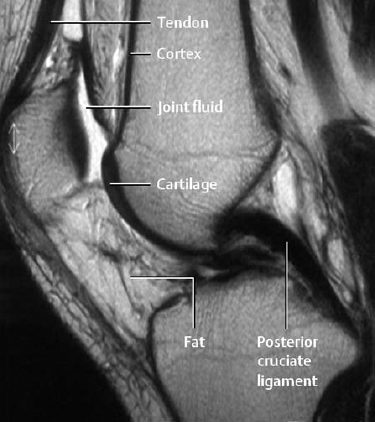
9 Joints Diseases of the joints comprise a clinically important, heterogeneous group of diseases with numerous overlapping pathologic, radiologic, and, above all, clinical manifestations. Degenerative and traumatic joint lesions are by far the most commonly encountered entities. Articular inflammations follow an aggressive course and generally are not infectious. Septic arthritis is relatively uncommon. Neurogenic, metabolic, and hematologic diseases also can lead to joint destruction. The classifications of joint diseases are not always universally accepted and are the subject of ongoing scientific discussion. Classifications are based on qualitative (presence or absence of radiographic finding) and quantitative (degree of severity) aspects, and are correlated with the pattern of anatomic distribution. The fact that joint diseases affect the soft tissues primarily (above all the synovial lining, articular cartilage, and tendons) and the bones secondarily is common to all joint disorders. A synovial joint consists of (Fig. 9.1): These entities together with muscles, tendons, and ligaments form an anatomic unit. The epiphyses of the articulating bones: The trabecule of the epiphyseal and metaphyseal spongiosa commonly follow characteristic courses (trajectories) along lines of compression forces. The cortex of articulating bones gradually decreases in width toward the joint. Where bone is covered by articular cartilage, the cortex is reduced to a very thin osseous layer that appears radiographically as a delicate line, referred to as the subchondral bone plate. It can be seen free of any superimposed structures along convex articular surfaces. Articular cartilage: With few exceptions, this consists of hyaline cartilage, which is nourished by diffusion from the joint fluid. In the calcified zone of the cartilage, small vessels arising from the subchondral bone region have been detected as well. Healthy cartilage is strikingly elastic and serves the role of shock absorber. With normal use, a liquid film always remains between the articulating cartilage surfaces. Joint capsule: By enveloping the joint, the capsule creates an intra-articular and extra-articular space. It inserts at the epiphysis of the articulating bone slightly outside the cartilage cover, creating an intra-articular area not covered by cartilage, referred to as the bare area. The joint capsule consists of an outer, predominately collagenous connective tissue, the fibrous capsule, and an inner synovial lining, also referred to as the synovial membrane. The synovial lining also covers all of the intra-articular osseous structures except the articular cartilage. It secretes synovial fluid, determines the fluid’s components, and phagocytizes any foreign material, such as organisms or cartilage fragments. Fig. 9.1 Anatomy of the synovial joint. Technical considerations and indications: Conventional radiography still plays a central role in diagnosing and monitoring joint disorders and in planning therapy. The routine examination consists of at least two views obtained in different projections, frequently with comparison views of the contralateral side. Digital radiography has the advantage over conventional film-screen systems of displaying the findings of interest at a brightness that is optimal for interpretation. Magnification radiography is reserved for special situations and has been largely replaced by sonography and MRI. Fluoroscopy with spot film is helpful only in selected cases, e.g., visualizing radiolucent halos around implants or displaying soft-tissue calcifications free from superimposed structures. Conventional tomography has largely been replaced by computed tomography and is performed only to address specific questions, e.g., in the region of the occipitocervical and cervicothoracic transition. Computed tomography is indicated for evaluating the sacroiliac, sternoclavicular, and temporomandibular joints and the atlanto-occipital transition, and for assessing specific problems related to degenerative changes of the spine. A special application is the combination of CT with myelography (‘CT myelography’) to achieve a detailed analysis of the nerve roots. For the large joints, computed tomography can delineate the radiographic features without superimposition of other structures. Arthrography, performed alone or combined with CT or MRI, is primarily used for the evaluation of the shoulder, wrist, and hip. The indications today center on post-traumatic and degenerative changes. The fundamental radiographic signs are described here to avoid repetition in subsequent chapters. The differential diagnostic implications are merely summarized. Soft-tissue swelling is recognized by an altered silhouette and by displaced or obliterated fat planes. This indicates juxta-articular bone loss. It appears as heterogeneous to patchy demineralization, indistinct spongiosa texture, and decreased number of trabeculae. These findings have a gradual transition to the variably wide homogeneous band of demineralization involving the opposing articulating end of the bone. Loss of the subchondral bone plate precedes erosions (‘pre-erosion’ according to Dihlmann). The cause can be either a trophic demineralization (from hyperemia) or a direct effect of pus or pannus (‘direct sign’). An erosion is a confined osseous defect involving the articulating end of the bone (‘joint socket’). Seen in profile, it is a defect, and seen end on, it appears as a ‘cyst.’ Depending on the activity of the disease process, the erosion can have an indistinct, distinct, or even sclerotic border. Fig. 9.3 a Juxta-articular osteoporosis in rheumatoid arthritis. For comparison: the osteoporosis in Sudeck disease (b) involves all bones. Fig. 9.4 Loss of subchondral bone plate in rheumatoid arthritis. Fig. 9.5 a Acute erosion from rheumatoid disease. b Same erosion with marginal sclerosis formed after methotrexate therapy and, as a result, less distinctly demarcated. Fig. 9.6 Erosion and its differential diagnosis. These are round, partially confluent defects in the articular ends of the bone. In arthritic conditions, they are also referred to as ‘signal cysts’. This indicates cartilage destruction. This is a reactive osteosclerosis formed by a coarse, often disorganized framework of lamellar bone. Single or multiple metadiaphyseal lamellar reactions are often present and often occur in the vicinity of the affected joints. Reactive bone apposition occurs as osteophytes and protuberances. The shape and distribution of these are often clues to differential diagnostic considerations. Joint destruction can progress to mutilation and end in ankylosis with fibrous or osseous bridging. Fig. 9.8 Concentric (a) and eccentric (b) joint-space narrowing in longstanding juvenile rheumatoid arthritis (a) and osteoarthritis (b). Fig. 9.9 Subchondral sclerosis indicates degenerative joint disease. a Preserved joint space, very subtle osteophyte formation. b Marked osteoarthritis of the knee. Fig. 9.10 Widening of the phalanges due to periosteal reaction in psoriatic arthritis. Fig. 9.11 Osteophytic overgrowth of different degrees at an interphalangeal joint (a) and knee (b). Fig. 9.12 a, b Mutilation. Typical ‘pencil-in-cup’ type in (b). c Osseous ankylosis of a proximal interphalangeal joint. Anterior spondylitis (Romanus lesion): This represents the focal destruction of the anterior or posterior borders of the vertebral body and is similar to an erosion. The Romanus lesion is an early manifestation of an inflammation affecting the spine (Fig. 9.14). This defect is almost always surrounded by a broad sclerosis, producing a rather typical triangular sclerosis referred to as shiny corner sign (Fig. 9.13). It can occur with or without associated focal destruction. Squared and rounded vertebra: Inflammatory destruction of the anterior surface of the vertebral body (anterior spondylitis) does not produce the classic Romanus lesion, but instead leads to loss of the anterior vertebral border. This results in squaring of the vertebral body due to flattening of its normally concave anterior surface (more often seen in the lateral than in the AP projection). Postinflammatory squaring can also develop differently; periosteal reaction with or without anterior spondylitis can fill the anterior concavity. Progression of anterior spondylitis causes destruction of the superior and inferior vertebral corner, resulting in a rounded vertebra (Fig. 9.15). Andersson lesion, type A (inflammatory type): This is an inflammatory reaction with focal destruction of the disk and vertebral body. It is characterized by irregularities along the end plates, usually accompanied by extensive sclerotic zones. Differentiation from mechanically induced osteochondrosis (predilection for L4 – S1) is sometimes difficult. Andersson lesion, type B (noninflammatory, pseudodegenerative type): This is a pseudarthrosis following a diskovertebral fracture of the demineralized and extensively ossified, stiff axial skeleton (as occurs in ankylosing spondylitis, Fig. 9.119). Syndesmophytes: These are ossifications of the outer fibers of the anulus fibrosus, caused by a progressive inflammatory process. Initially, they are thin, vertical outgrowths along the contour of the disk. With progression, the syndesmophytes thicken and involve the anterior longitudinal ligament and paravertebral soft tissues. The end result is the ‘bamboo spine’. Spondylophytes: These are ossifications of the vertebral margins caused by disk degeneration, but might be secondary to an inflammation. The submarginal spondylophyte arises at the insertion of the anterior longitudinal ligament, several millimeters from the diskovertebral junction. Initially, it grows horizontally and then vertically (forming a hook). The marginal osteophyte merges horizontally with the end plate. In addition to these major types – syndesmophyte secondary to an inflammatory process and spondylophyte secondary to degenerative alterations – numerous intermediate types are encountered. Parasyndesmophytes are asymmetric ossifications that are thicker than syndesmophytes and not vertically oriented but are curved or commashaped and separated (‘para-’) from the margin of the vertebral body. They occur in three types: steer-horn type; paradiskal elongated, thin type; and paradiskal ossicle. The term mixed osteophyte is applied by some authorities to an osteophyte constituting a mixture of syndesmophyte and spondylophyte. Any interpretation of these special types is difficult, and in assigning an etiology one should always consider further radiographic findings (Fig. 9.17). Block vertebra: This can be a developmental abnormality or the result of a preceding inflammatory process. Sacroiliitis is the hallmark of the seronegative and HLA-B27-positive spondyloarthropathies. Unilateral sacroiliitis can also occur on the basis of a bacterial infection. Seronegative spondyloarthropathies constitute a heterogeneous entity of clinically defined subcategories: Radiographic signs of sacroiliitis (‘variegated picture’ of Dihlmann, Fig. 9.16): Fig. 9.13 ‘Shiny corner’ in anterior spondylitis. Fig. 9.14 MRI of a Romanus lesion. a The T2-weighted SE sequence shows triangular edema at the anterior-superior corner of a vertebral body. Strong enhancement after the administration of contrast medium. b T1-weighted SE sequence. Fig. 9.15 Squaring and rounding of the vertebral body due to anterior spondylitis. Fig. 9.16 ‘Variegated picture’ of sacroiliitis. Fig. 9.17 Comparison of the different ossifications between vertebral bodies. a Syndesmophyte, thin ossification, vertical growth. b Parasyndesmophyte, separated from the margin of the vertebral body. c Parasyndesmophyte of the ‘Steer-horn type.’ d Degenerative spondylophytes. Visualization of the joint requires probes with frequencies of 7 to 13 MHz. For examination of the strongly reflective structures of the neonatal hip, a frequency of 5 MHz is adequate. The examination of each joint should follow an established protocol, which may be supplemented by additional sections, depending on the clinical question. When tendons and muscles are examined, the acoustic anisotropy of the muscular and collagenous fibers must be taken into consideration. Due to the internal orientation of these structures, the echogenicity changes with the angulation of the probe. Differences in echogenicity caused by this effect should not be misinterpreted as lesions (Fig. 9.18). Any report of sonographic findings should include the following aspects: Location: Anatomic location and contact with neighboring structures. Echogenicity: Anechoic, hypoechoic, hyperechoic. Margin: Sharp, indistinct, partially sharp, partially indistinct. Acoustic quality behind the lesion: Acoustic enhancement, acoustic shadowing. Most Important Sonographic Differential Diagnoses: Anechoic lesions: Cysts, ganglions, effusions. Caution: Hematomas, abscesses, and, rarely, tumors can be anechoic. Hypoechoic lesions: Hematomas, abscesses, granulation tissue, many lipomas (characteristic ‘pennate’ structures), many benign and almost all malignant tumors, many tendon tears. Some effusions or cysts can also contain echogenic fluid. Echogenic lesions: Lipomas, tendon ruptures (reflecting interfaces), calcifications or ossifications (typical acoustic shadowing), defects at the bone surface (e.g., erosions, Hill-Sachs deformity). What Questions Can Be Answered by Sonography of Joints and juxta-Articular Structures? The three-phase bone scan with Tc 99 m diphosphonate is performed with anterior and lateral views. The strength of bone scanning is that it provides an overview of disease manifestations in the skeleton, yielding information critical for the differential diagnosis. The most important indications are: Fig. 9.18 Because of acoustic anisotropy of fibers, the echogenicity of lamellated structures (here: normal rotator cuff) depends on the angle of the interrogating sound beam. This effect must be distinguished from pathologic differences in echogenicity. Exquisite visualization of soft tissues and bone marrow has made MRI an examination of enormous value. Examination technique: To achieve good resolution, the use of suitable superficial coils is mandatory. Examination protocols: Soft-tissue contrast is determined by the selected pulse sequences and is characteristic for each individual structure and for the joint content (Fig. 9.19). Signal patterns of pathologic processes: Which Questions Can MRI of the Joints and Adjacent Structures Answer? Fig. 9.19 MRI of the knee. Normal sagittal plane of a T2-weighted TSE sequence. These basically different diseases are in reality inseparably intermingled, since damage of the cartilage plays the crucial role in both diseases. ‘Primary’ osteoarthritis invariably induces an inflammatory reaction of the synovitis due to faulty articulation and cartilaginous debris in the joint (secondary arthritis). Likewise, the cartilage damage of ‘primary’ arthritis causes a secondary osteoarthritis. These mechanisms explain why radiographically visualized joint changes represent a summation effect of the outcome of both disease processes. Conclusion: differentiating the signs of degenerative joint disease from those of arthritis is often difficult and sometimes impossible. However, the critical clinical relevance (i.e., totally different therapeutic approaches) demands that a differentiation should always be attempted, whether a disease is caused and maintained primarily by synovitis or by damaged cartilage. The cause of osteoarthritis is defective cartilage, with the cartilage in part damaged by mechanical or metabolic processes. In many cases, however, the etiology remains unclear (see page 308–312 for further details). In the course of degenerative alterations, cartilage destruction leads to uneven mechanical loading, with overloading and subsequent destruction of still spared intact cartilage (Fig. 9.20). The primary result of cartilage destruction is narrowing of the load-bearing zone of the joint space. The lack of the shock-absorbing cartilage increases the impact load of the subchondral bone, resulting in small areas of osteonecrosis, which become hypervascular toward the marrow space. The hypervascularity leads to increased osteoblastic activity and trabecular thickening, ultimately resulting in a sclerosis. Since the bone cannot withstand the continued overload, trabecular microfractures occur and, ultimately, the trabecular structures collapse. This leads to the formation of so-called ‘detritic cysts’, which strictly speaking are not cysts, but are designated as such because of their radiographic appearance. It is still unresolved whether they are formed solely by subchondral compression fractures or by joint fluid extending into the trabecular space or both. A connection to the joint capsule can be detected only in some cases. The composition of the cyst contents (myxoid, proteoglycans, articular cartilage fragments, and metaplastically formed cartilage) suggests a combination of both mechanisms. Within the cyst, vascularized fibro-cartilage tissue can form and lead to enhancement on MRI. On conventional radiography, the subchondral cysts appear as localized osteolytic lesions that are more-or-less surrounded by a pronounced sclerotic rim (Fig. 9.22).
Introduction and Synopsis
Anatomy of the Synovial Joints
Signs of Joint Diseases on Radiography and CT
 For the interpretation of radiographs, a bright spotlight with circular collimation (to bring out the soft tissues) and a magnifying glass (to analyze delicate osseous structures) should always be available.
For the interpretation of radiographs, a bright spotlight with circular collimation (to bring out the soft tissues) and a magnifying glass (to analyze delicate osseous structures) should always be available.
Radiographic Signs of the Peripheral Joints and Their Role in the Differential Diagnosis
Soft-tissue Swelling (Fig. 9.2)
Juxta-articular Osteoporosis (Fig. 9.3)
Loss of the Subchondral Bone Plate (Fig. 9.4)
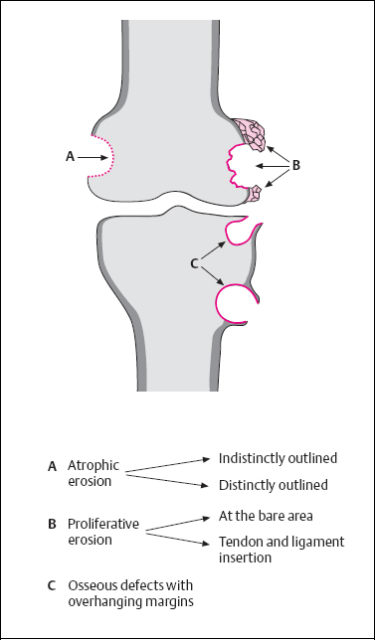
Erosion (Fig. 9.5, 9.6)




Circumscribed Osteolytic Foci (‘Subchondral Cysts,’ ‘Geodes’) (Fig. 9.7)
Joint-space Narrowing (Fig. 9.8)
Subchondral Sclerosis (Fig. 9.9)
Lamellar Periosteal Reaction (Fig. 9.10)
Reactive Bone Apposition (Fig. 9.11)
Mutilation and Ankylosis (Fig. 9.12)




Radiographic Signs at Specific Joints
Spine
Sacro-iliac (SI) Joints
 Only the anteroinferior aspect of the SI joint is a synovial articulation. The posterior and superior portion (the fibrous retro-articular space) of the ‘joint’ is connected by ligaments and lacks articular cartilage.
Only the anteroinferior aspect of the SI joint is a synovial articulation. The posterior and superior portion (the fibrous retro-articular space) of the ‘joint’ is connected by ligaments and lacks articular cartilage.


Sonography
 Hypoechoic lesions are nonspecific, and the differential diagnosis generally is determined by the clinical presentation and the findings of other imaging methods. Especially in synovial arthritis, the differentiation between hypoechoic effusion and pannus is very difficult or even impossible.
Hypoechoic lesions are nonspecific, and the differential diagnosis generally is determined by the clinical presentation and the findings of other imaging methods. Especially in synovial arthritis, the differentiation between hypoechoic effusion and pannus is very difficult or even impossible.
Scintigraphy
MRI
Image Analysis
Arthritis versus Osteoarthritis (Overview)
Pathogenesis of Osteoarthritis and Its Radiographic Features
| Pathologic changes | Corresponding radiologic changes |
|---|---|
| Synovitis with joint effusion | Soft-tissue swelling, widened joint space |
| Hyperemia | Juxta-articular osteoporosis |
| Destruction of cartilage caused by inflammation or pannus | Joint-space narrowing |
| Destruction of subchondral bone and the ‘bare area’ caused by inflammation or pannus | Loss of the subchondral bone plate, marginal erosions, subchondral ‘signal’ cyst formation, mutilation |
| Extension of synovial fluid into the spongiosal space, subchondral compression fractures, and necroses | Subchondral ‘detritic’ cyst formation |
| Fibrosis and osseous ankylosis | Osseous ankylosis |
| Contractures of capsules, ligaments, and muscles | Deformities, subluxation, dislocation |
| Reactive osseous appositions, in part with fibrocartilage cover | Osteophytes |
| Reactive osteosclerosis forming a coarse, often disorganized meshwork of lamellar bone | Subchondral sclerosis |
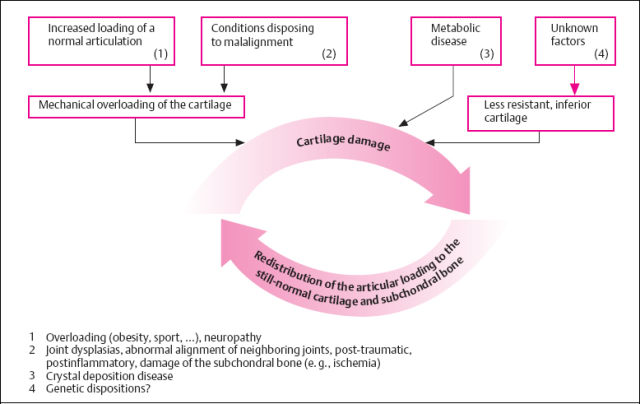
Fig. 9.20 Conceptual overview of the pathophysiology of osteoarthritis.
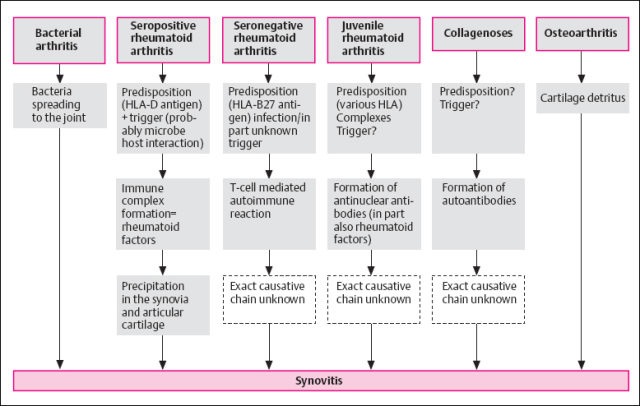
Fig. 9.21 Conceptual overview of the pathophysiology of inflammatory arthritis.
With progression of the destructive and reparative processes, joint deformities increase over years, leading to misalignment and, ultimately, mutilation.
Pathogenesis of Arthritis and Its Radiographic Appearance
Arthritis has a vast number of causes (Fig. 9.21). They all have in common that they induce an inflammation of the synovial lining that is responsible for the disease process. This explains the similarity of the morphologic articular changes, regardless of the particular cause.
Any individual arthritis, in contrast, is characterized by its clinical course and age of onset, as well as by the distribution of the lesions in the skeletal system (‘distribution pattern’) and joints.
Synovitis with thickening of the synovial lining and hyperemia initially causes joint effusion and periarticular edema that are clinically and radiographically apparent as soft-tissue swelling. The effusion can cause joint-space widening, with potential damage to the joint capsule (e.g., due to recurrent inflammation). Furthermore, the hyperemia allegedly is a major cause of juxta-articular osteoporosis (arthritic collateral phenomenon).
Arising from the synovial lining as well as in the subchondral region, vessels and soft tissues proliferate and form granulation tissue (‘pannus’). The pannus and inflammatory effusion erode joint cartilage and also bone not covered by the protecting cartilage layer (‘bare area’) adjacent to the capsular insertion, This leads to the formation of erosions. In the course of the disease, cartilage destruction progresses, and pannus extends from the peripheral and subchondral sites towards the joint, initially leading to the destruction of the subchondral bone plate and eventually to erosions and osteolytic defects (Fig. 9.23).
With progression of the disease process, cartilage and bone are further destroyed (resulting in joint space narrowing), eventually leading to complete destruction with mutilation and misalignment. This affects small joints quite frequently. With complete destruction of the joint, the disease arrests since the inflammation has subsided. In this stage, the reparative processes can produce an initially fibrous and later osseous bridging of the former joint resulting in ankylosis.
A long chronic process may show sclerosis around the erosions and cysts representing signs of repair. This enables differentiation between old and acute lesions.
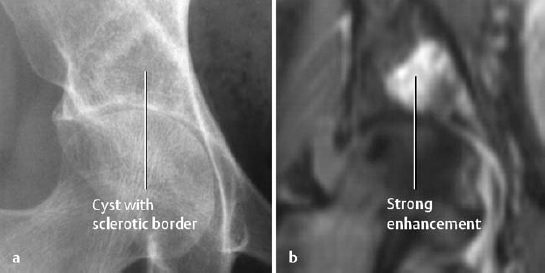
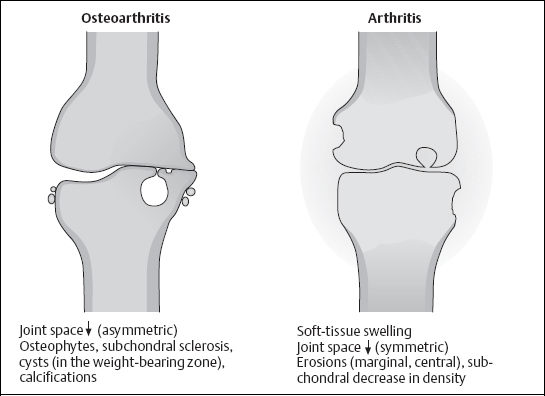
Fig. 9.23 Schematic comparison of the most relevant signs of erosive osteoarthritis and inflammatory arthritis.
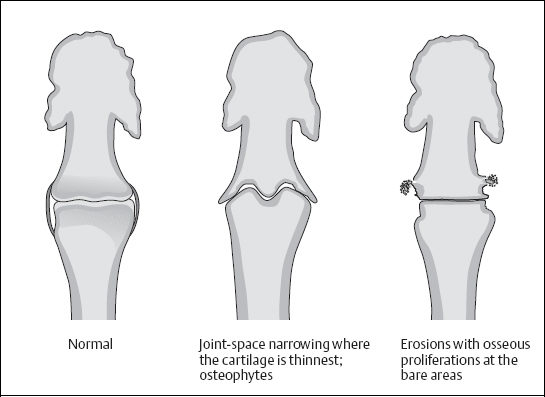
Fig. 9.24 Schematic comparison of erosive osteoarthritis and psoriatic arthritis.
Enthesopathies (Fibro-ostosis and Fibro-ostitis)
Anatomic Consideration: The epiphyseal and apophyseal insertions of the tendons, ligaments, and joint capsules lack periosteal coverage, and the fibers of the fibrous structures are not directly anchored to the underlying bone. Instead, a zone of fibrocartilage is interposed between the taut fiber bundles and bone. This fibrocartilage is mineralized along its interface with bone. At the diaphysis, in contrast, the fiber bundles extend fan-like into the covering periosteum, intertwine with the periosteal fibers, and only then penetrate into the osseous tissue. Thus, there are definite morphologic differences despite the identical functions of these tendinous, ligamentous, and capsular attachments (so-called ‘stretch protection’).
It should be kept in mind that the region of osseous insertion of fibers always preserves its potential of new bone formation. Trauma, degeneration, inflammation, and altered metabolism can act on this zone and induce new bone formation.
Fibro-ostosis
This is a traumatic or degenerative enthesopathy. It also occurs with sclerosis and acromegaly. An especially extensive manifestation is diffuse idiopathic skeletal hyperostosis (DISH).
Pathologic findings, clinical presentation, and imaging features depend on the duration, location, and extent of the change. Repetitive trauma induces ‘inflammatory’ tissue reactions with lymphocytic infiltration, edema, and resorptive changes at the bone. This can progress to calcifications and cystic bone defects.
Locations: Calcaneus (posterior and plantar calcaneal spur), greater trochanter, ischial tuberosity, olecranon, and iliac crest (Fig. 9.26). Other locations are less common.
 Fibro-ostosis is usually asymptomatic. Inflammatory reaction due to overuse can cause pain and swelling (e.g., ‘epicondylitis’ in tennis players, golfers).
Fibro-ostosis is usually asymptomatic. Inflammatory reaction due to overuse can cause pain and swelling (e.g., ‘epicondylitis’ in tennis players, golfers).
 – Irregular calcifications of the tendons and ligaments (Fig. 9.25).
– Irregular calcifications of the tendons and ligaments (Fig. 9.25).
- New bone formation at the tendon insertions (spurs, excrescence, Fig. 9.26).
Insertion defects are possible at the site of muscle insertions. These contour defects (‘rarefying fibro-ostosis’) occur in the region of the pubic bone, ilium, and sacrum, as well as in the region of the femoral neck and humerus (Fig. 9.27).
Fibro-ostitis
Two types of fibro-ostitis are distinguished:
- productive fibro-ostitis (new bone formation with specific radiographic features),
- rarefying fibro-ostitis (inflammatory insertion erosions, Figs. 9.28, 9.29).
Fibro-ostitis is a sign of inflammatory joint diseases, especially common in psoriatic arthritis, Reiter syndrome and ankylosing spondylitis.
 The clinical findings consist of localized swelling and pain.
The clinical findings consist of localized swelling and pain.
 The productive fibro-ostitis produces new bone, which is irregularly outlined and has indistinct frayed borders.
The productive fibro-ostitis produces new bone, which is irregularly outlined and has indistinct frayed borders.
The rarefying fibro-ositis is characterized by an indistinctly outlined osseous defect at the insertion of the tendon, ligament or capsule. Reactive sclerosis is common around the defect (Fig. 9.29).
 ‘Acute’ fibro-ostosis with inflammatory tissue reaction and fibro-ostitis in rheumatoid diseases are not always distinguishable on imaging studies, since both conditions show evidence of inflammation on bone scan (increased activity) and MRI (edema).
‘Acute’ fibro-ostosis with inflammatory tissue reaction and fibro-ostitis in rheumatoid diseases are not always distinguishable on imaging studies, since both conditions show evidence of inflammation on bone scan (increased activity) and MRI (edema).
 Enthesopathy in rheumatoid diseases can be detected on MRI quite early, before osseous changes are manifest (Fig. 9.30).
Enthesopathy in rheumatoid diseases can be detected on MRI quite early, before osseous changes are manifest (Fig. 9.30).
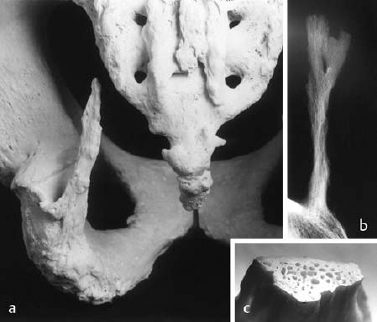

Fig. 9.26 Extensive classic fibro-ostoses (enthesopathic change) within the pelvis.
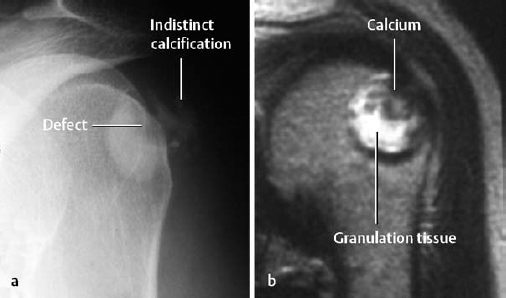
Fig. 9.27 Chronic calcifying fibro-ostosis at the insertion of the infraspinatus muscle, a Oblique projection. The T2-weighted SE sequence (b) indicates absence of inflammation in the region of the tendinous insertion (no edema).

Fig. 9.28 Enthesopathy (fibro-ostitis) at the insertion of the infraspinatus muscle in psoriasis.
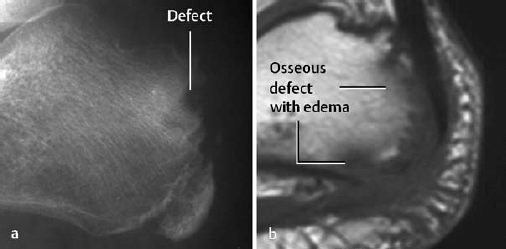
Fig. 9.29 Rarefying fibro-ostitis at the calcaneal tuberosity in an 8-year-old boy with seronegative spondyloarthropathy, a Lateral view. b T1-weighted SE image.
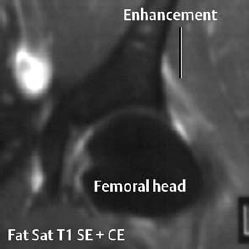
Fig. 9.30 Enthesopathy without osseous involvement in seronegative spondyloarthropathy.
Degenerative Joint Diseases
Osteoarthritis of the Peripheral Joints
 The etiology of joint degeneration is multifactorial. Misalignment, neuromuscular dysfunction, ligamentous loosening, repetitive local stress, and trauma are the commonest causes of articular overload. The compressible, noncalcified hyaline cartilage resists the increased mechanical stress at the articular surface for a relatively long time. The compressive force, however, is transmitted to the underlying calcified cartilage and subchondral bone plate. Both layers act as a functional unit that is barely compressible and more susceptible to damage by overloading. Whether the damage begins in the subchondral region or in the cartilage is undetermined. Both layers are connected by tiny channels, which are assumed to exchange fluid and to equalize the pressure between the subchondral region and cartilage. Many connecting channels are found in articular zones subjected to a high load, and correspondingly fewer channels in those zones are subjected to a lower load.
The etiology of joint degeneration is multifactorial. Misalignment, neuromuscular dysfunction, ligamentous loosening, repetitive local stress, and trauma are the commonest causes of articular overload. The compressible, noncalcified hyaline cartilage resists the increased mechanical stress at the articular surface for a relatively long time. The compressive force, however, is transmitted to the underlying calcified cartilage and subchondral bone plate. Both layers act as a functional unit that is barely compressible and more susceptible to damage by overloading. Whether the damage begins in the subchondral region or in the cartilage is undetermined. Both layers are connected by tiny channels, which are assumed to exchange fluid and to equalize the pressure between the subchondral region and cartilage. Many connecting channels are found in articular zones subjected to a high load, and correspondingly fewer channels in those zones are subjected to a lower load.
Distribution of Arthritic Changes
Primary osteoarthritic changes are found mainly in the spine and in the hip, knee, first metacarpophalangeal articulation, and interphalangeal articulations (Fig. 9.31). In contrast, the shoulder, elbow, foot, and ankle are infrequently involved. Osteoarthritic changes found in these joints should always be considered secondary in nature. Why primary arthritic changes rarely involve the ankles but commonly involve the hands is unknown.
Secondary osteoarthritic changes have preferred sites determined by the underlying joint disorder (see Table 9.2).
| Causes | Sites |
|---|---|
| Trauma | Knee, hip, shoulder, elbow, hand, ankle |
| Joint dysplasia | Hip |
| Osteonecrosis | Hip, knee, shoulder |
| Rheumatoid arthritis | Hand, foot, hip, knee |
| Acromegaly | Hand, foot, knee, shoulder |
| Gout | Hand, foot, knee, elbow |
a) Damage to the Hyaline Articular Cartilage and Synovial Lining
Damage to the articular cartilage is called chondromalacia. The four stages in cartilage damage are:
I Cartilage edema (Fig. 9.32),
II Start of cartilage fragmentation with defects (Fig. 9.33),
III Cartilaginous fibrillation with large defects (Fig. 9.35),
IV Complete cartilage denudation.
In cartilage degeneration, the superficial zone of collagenous fibers is damaged first (in some cases accompanied by degradation of proteoglycans). The cartilage matrix, which consists mainly of hydrophilic proteoglycans, accumulates more water and becomes swollen, leading to cartilage edema. The resultant increased mechanical friction, together with the lost normal elasticity of the cartilage, leads to fragmentation of the cartilage substance with formation of defects.
Fragmentation and defect formation progress, producing the phenomenon known as fibrillation. This is the most frequently observed finding, since it also is the time when patients consult their physician because of increasing joint pain. Further progression leads to denudation of the articular surface (Fig. 9.34).
The synovial lining plays a major role in causing symptoms in osteoarthritis. Increased friction leads to mechanical and histochemical irritation (synovitis), and with time a chronic effusion with its complications may develop (e.g., synovial cysts). Morever, nourishment of the cartilage supplied by synovial fluid is compromised. This can be followed by shrinkage of the joint capsule, adding joint deformities to the altered cartilage coat and cortical bone end.
b) Subchondral Damage
Continued overloading quickly leads to small areas of marrow edema, microhemorrhage and microfracture, and even focal osteonecrosis. Edematous areas can resolve within a few weeks without any residue. However, hyperemia, cellular infiltration, and proliferation of fibrovascular tissues might develop in the otherwise highly vascularized and nerve-rich subchondral bone. These changes can also be fully repaired, but might leave behind defects in the form of subchondral cysts (filled with liquid, myxoid, fibrous, or cartilaginous material) or reparative bone and subchondral sclerosis. These ‘residues’ (cysts, subchondral sclerosis) interfere with the fluid exchange between the subchondral region and cartilage. The radiologic manifestations of these processes are local subchondral osteopenia, cysts, or sclerosis.
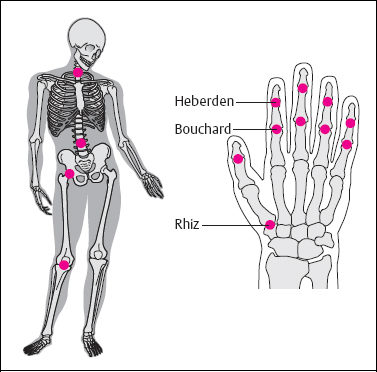
Fig. 9.31 Distribution pattern of primary degenerative osteoarthropathy at the peripheral joints.
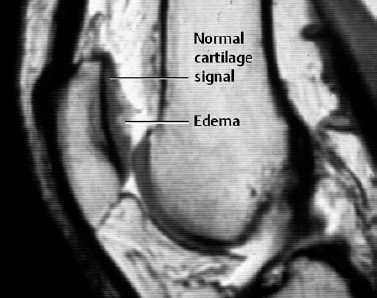
Fig. 9.32 Sagittal MR arthrography of the knee, T1-weighted SE sequence. Cartilage edema along the retropatellar articular surface, indicating the first stage of damage to the articular cartilage.
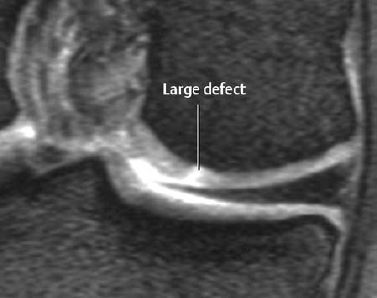
Fig. 9.33 The start of cartilage fragmentation of the knee; indirect MR arthrography, gradient echo sequence. Stage II.
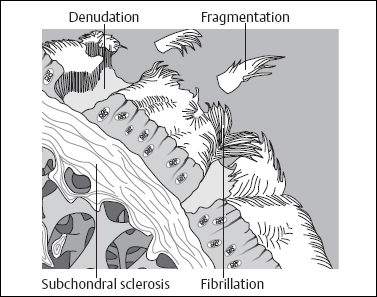
Fig. 9.34 Degenerative changes of the cartilage and subchondral region.
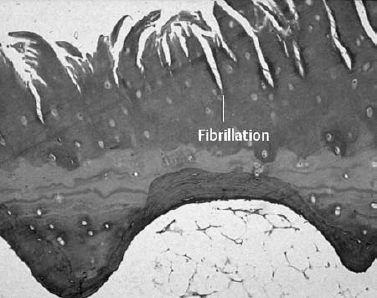
Fig. 9.35 Histologic section through the articular cartilage. Stage III.
Chondrocytes are highly specialized and cannot divide. If damaged, they become hypertrophied and develop increased nuclei to achieve increased production of matrix and collagenous fibers (= intrinsic repair). Subchondral damage can induce the formation of new cartilage, which arises from the depth of the subchondral region or from the edge of the articular cartilage to cover the defects in the cartilage or the denuded articular surface (= extrinsic repair). This ‘reparative’ cartilage contains more fibers than the original cartilage, and its surface is quite irregular and less compressible. This is why the repaired articular surface is less resistant to compressive forces.
d) Osteophyte Formation
Persistent overloading of a joint, especially if it is unstable, will produce new bone in the form of osteophytes by local activation of growth factors and by local tensile forces. The formation of osteophytes follows the same principle that underlies the formation of fibro-ostoses as metaplastic ossification of reparative connective tissue. By broadening the articulating surface, the marginal osteophytes reduce the local overload and improve stability. At the same time, they restrict joint motion, which further reduces any possible overload.
e) Meniscus and Disk Damage
Articulations can contain fibrocartilaginous structures in the form of menisci, as found in the knee, or disks, as found in the wrist, primarily to distribute the mechanical load more evenly across incongruent cartilage surfaces.
In the meniscus, the typical degenerative tear is horizontally directed. Such tears are found in 50%–70% of individuals 60 years old and older and are asymptomatic in the large majority. Meniscal damage is frequently associated with additional degenerative changes. Meniscal malformations (e.g., discoid meniscus) tend to accelerate degeneration. The typical degenerative tears in the triangular fibrocartilage of the wrist are on the radial side. An increased incidence of disk degeneration is observed with congenital ulnar minus variants.
Latent, Active, Erosive, and Atrophic Osteoarthritis
 A universally accepted terminology for degenerative alterations in joints does not exist. The most frequent, interchangeably used terms are degenerative joint disease, (degenerative) osteoarthritis, (osteo) arthrosis, and arthrosis deformans. The latter is the preferred term in the European literature. Osteoarthritis, which is widely accepted in the US, is the preferential term used in this book. Regardless of the unsettled nomenclature and arbitrary descriptive designations, a distinction between latent and active degenerative joint alterations is clinically relevant. Active joint degeneration is dominated by synovitis and produces joint symptoms perceived by the patient as signs of a disease process. There is often an associated effusion. In this setting, patients having primarily degenerative joint disease show typical symptoms of an inflammatory joint.
A universally accepted terminology for degenerative alterations in joints does not exist. The most frequent, interchangeably used terms are degenerative joint disease, (degenerative) osteoarthritis, (osteo) arthrosis, and arthrosis deformans. The latter is the preferred term in the European literature. Osteoarthritis, which is widely accepted in the US, is the preferential term used in this book. Regardless of the unsettled nomenclature and arbitrary descriptive designations, a distinction between latent and active degenerative joint alterations is clinically relevant. Active joint degeneration is dominated by synovitis and produces joint symptoms perceived by the patient as signs of a disease process. There is often an associated effusion. In this setting, patients having primarily degenerative joint disease show typical symptoms of an inflammatory joint.
Erosive osteoarthritis (synonyms: inflammatory osteoarthritis, destructive osteoarthritis, Fig. 9.38) is a special form of osteoarthritis with swelling, redness and pain as found in synovial arthritis. The cardinal symptom is the radiographically detectable erosion. Distal and proximal interphalangeal joints are preferentially affected, but involvement of any joint is possible. An effusion (best shown by sonography) is always present. In destructive osteoarthritis, the erosions are more central than marginal and either progress to large cysts or become sclerotic.
 Erosive osteoarthritis also begins with a chondropathy, followed by synovitis. Consequently, it falls in the group of degenerative joint diseases. Erosive osteoarthritis is a diagnosis of exclusion. Conditions to be excluded are gouty arthropathy, psoriatic arthropathy, rheumatoid arthritis superimposed on osteoarthropathy, and infectious arthritis.
Erosive osteoarthritis also begins with a chondropathy, followed by synovitis. Consequently, it falls in the group of degenerative joint diseases. Erosive osteoarthritis is a diagnosis of exclusion. Conditions to be excluded are gouty arthropathy, psoriatic arthropathy, rheumatoid arthritis superimposed on osteoarthropathy, and infectious arthritis.
Atrophic osteoarthritis is characterized by loss of cartilage (leading to joint-space narrowing) with absent or only minimal reactive changes (sclerosis, osteophytes). It tends to involve the hands (Fig. 9.47).
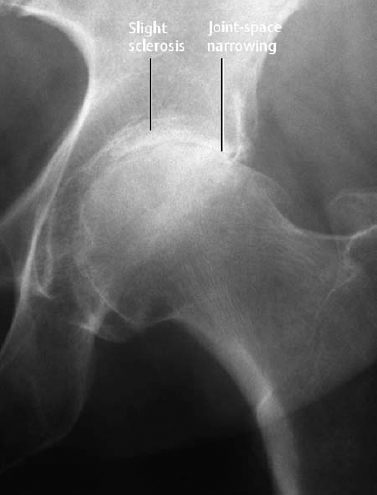
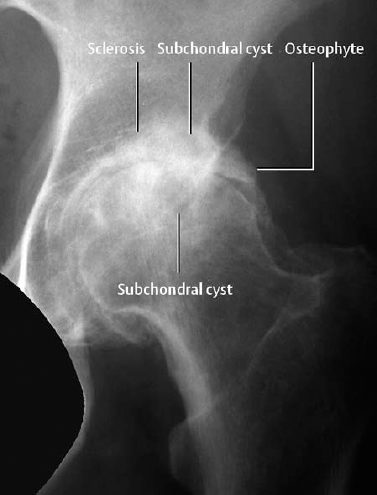
Fig. 9.37 Signs of degeneration seen here in a representative case of an advanced osteoarthritis.

Fig. 9.38 Resolution of a polyarthritis over 10 years. In 1985, the proximal interphalangeal joint of the middle finger is the only spared visualized joint. In 1991, an erosive arthritis with excessive erosions has developed here. Subsequently, the inflammatory component regresses, and a latent osteoarthritis has developed. The latent osteoarthritis of the remaining interphalangeal joints remains unchanged throughout the observation period.
 | Typical signs of osteoarthritis are – pain on weight bearing, |
- limited range of motion,
- subluxation,
- subcutaneous soft-tissue nodules (Heberden nodes at the distal interphalangeal joints and Bouchard nodes at the proximal interphalangeal joints).
Imaging is used to confirm the diagnosis and to follow the clinical course. The radiographic findings often lag behind the clinical findings for years.
 Technical consideration: To detect alignment abnormalities, radiographic films have to be obtained under weight bearing (standing).
Technical consideration: To detect alignment abnormalities, radiographic films have to be obtained under weight bearing (standing).
Primary and secondary osteoarthritic changes have the same basic manifestation (Figs. 9.36, 9.37; also compare with pages 294–296):
- joint-space narrowing, especially of the weight-bearing portions,
- subchondral sclerosis,
- subchondral cyst formation,
- osteophytes,
- joint deformity with misalignment,
- chondrocalcinosis (Fig. 9.40),
- loose intraarticular bodies (‘joint mice’),
- insertional calcifications of ligaments, tendons, capsules.
Localized subchondral radiolucency, with or without joint-space narrowing, is an early diagnostic sign, but it is rarely encountered (Fig. 9.39).
 The three-phase bone scan shows increased uptake caused by increased regional perfusion (= early phase) and by increased bone turnover (= late phase) (Fig. 9.42). The role of the bone scan is determination of the distribution pattern, which frequently assists in discriminating between arthritis and (active) osteoarthritis.
The three-phase bone scan shows increased uptake caused by increased regional perfusion (= early phase) and by increased bone turnover (= late phase) (Fig. 9.42). The role of the bone scan is determination of the distribution pattern, which frequently assists in discriminating between arthritis and (active) osteoarthritis.
 The pathologic changes of cartilage described above (cartilage edema, swelling, and fibrillation) can be visualized with MRI ‘cartilage sequences’ (T2-weighted gradient echo sequences with and without fat suppression) or by means of direct or indirect MR-arthrography of the major joints. Moreover, T2-weighted turbo (fast) spin echo sequences can also be used advantageously. The subchondral changes (microhemorrhages, microfractures, micronecrosis) are not well delineated because of their extremely small size.
The pathologic changes of cartilage described above (cartilage edema, swelling, and fibrillation) can be visualized with MRI ‘cartilage sequences’ (T2-weighted gradient echo sequences with and without fat suppression) or by means of direct or indirect MR-arthrography of the major joints. Moreover, T2-weighted turbo (fast) spin echo sequences can also be used advantageously. The subchondral changes (microhemorrhages, microfractures, micronecrosis) are not well delineated because of their extremely small size.
See pages 108 and 316 for the MRI signs of the pathology of menisci and disks.
Osteoarthritis of Specific Joints
Osteoarthritis of the Knee
The knee is a common site of primary and secondary osteoarthritis. The latter is frequently associated with misalignment, instability, preceding severe trauma, osteonecrosis, and inflammation, as well as with neurogenic, metabolic, or hematologic disorders. Radiography can distinguish between:
- medial tibiofemoral,
- lateral tibiofemoral,
- patellofemoral
osteoarthritis of the knee (Fig. 9.41). To detect or exclude misalignments, views with the patient standing (with a vertically placed measuring device) are indicated. Degenerative meniscal changes are best detected with MRI.
 PVNS (pigmented villonodular synovitis): This condition is dominated by large cystoid defects in the articular ends of the bone. In its early stages there is no joint-space narrowing.
PVNS (pigmented villonodular synovitis): This condition is dominated by large cystoid defects in the articular ends of the bone. In its early stages there is no joint-space narrowing.
Osteoarthritis of the Hip
In the hip, superolateral joint-space narrowing is more common than medioinferior narrowing (Fig. 9.43). Upright views of the hip show superolateral, superomedial or axial migration of the femoral head to the best advantage. Displacement of the femoral heads into the acetabulum with increasing depths of the acetabular cavity is referred to as acetabular protrusion. Besides dysplasias and other malformations (e.g., coxa vara and valgus), Paget disease and fibrous dysplasia should be added to the causes of secondary osteoarthritis already discussed.
An unusual variant of erosive osteoarthritis, the atrophic-destructive ‘osteoarthritis’ of the hip, leads to destruction of portions of the femoral head and, to a lesser degree, of the acetabulum, with relatively little reaction. This process takes place over months and mainly affects elderly women.
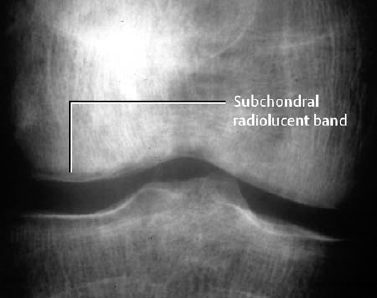
Fig. 9.39 Osteoarthritis of the knee joint.

Fig. 9.40 Chondrocalcinosis of the triangular fibrocartilage as part of degenerative joint disease.
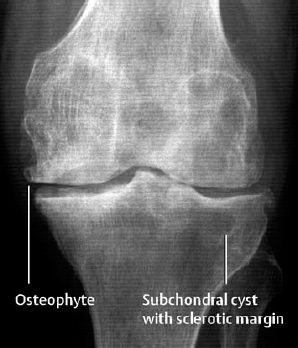
Fig. 9.41 Osteoarthritis of the medial and lateral tibiofibular joints with a large subchondral cyst.
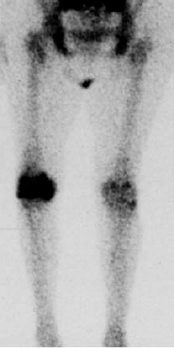
Fig. 9.42 Three-phase bone scan (late phase). Active osteoarthritis involving both knees, the right more than the left. Typical increase in activity in the weight-bearing zones.
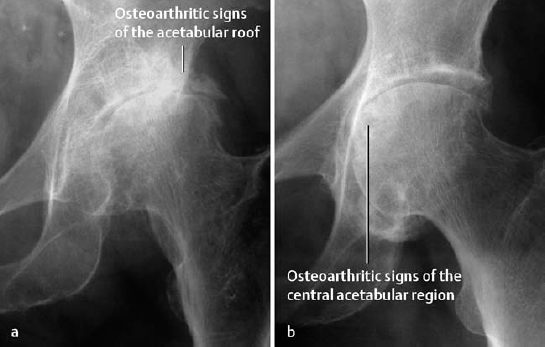
Fig. 9.43 Osteoarthritis of the hips, (a) Superolateral narrowing with upward and lateral displacement of the femoral head, (b) Medioinferior narrowing.
Infectious arthritis is diagnosed by analyzing the joint effusion after hip aspiration.
Osteonecrosis only in rare cases does involve the femoral head and the acetabulum at the same time. MRI can be used for further diagnostic evaluation of inconclusive cases.
Remember that circumferential osteophytes (‘collar’) can be mistaken for an impacted subcapital fracture of the femoral neck.
Osteoarthritis of the Shoulder
Primary osteoarthritis of the shoulder is rare. Secondary osteoarthritis (Fig. 9.44) develops on the basis of misalignment, trauma, Paget disease, dysplasias, acromegaly, and osteonecrosis, or as part of neurogenic, metabolic, and hematologic diseases. In the majority of cases, the glenohumeral and acromioclavicular articulations are equally involved. Acromioclavicular osteoarthritis can lead to the development of impingement syndrome with compression of the supraspinatus tendon.
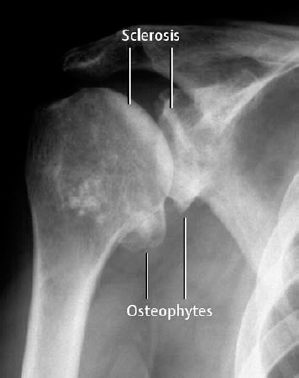
Fig. 9.44 Osteoarthritis of the shoulder with deformity, osteophytes, and marked subchondral sclerosis.
Osteoarthritis of the Finger and Carpal Bones
Primary osteoarthritis of the distal (= Heberden) and proximal (= Bouchard) interphalangeal joints is the commonest osteoarthritis (Figs. 9.45, 9.46). The so-called ‘Heberden and Bouchard nodes’ are soft-tissue protuberances caused by underlying osteophytes. Osteoarthritis of the first carpal–metacarpal articulation frequently has an erosive component (Fig. 9.48). Osteoarthritis of the carpal bones mainly affects the scaphoid-trapezium-trapezoideum complex. A primary radiocarpal osteoarthritis is relatively rare.
In 1998, Dihlmann and Dihlmann described a subtype of osteoarthritis of the fingers, which they call osteoclastic osteoarthritis of the fingers. It is characterized by subchondral osteolytic areas that involve at least one-third of the length of the phalanx. These areas are larger than detritic cysts, which are confined to the articular end of the bone.
Secondary osteoarthritic changes can be observed together with chronic inflammatory conditions, acromegaly, and metabolic disorders such as hemochromatosis, diabetes mellitus, pseudogout (= CPDD).
 Hemochromatosis leads to osteophytes with extensive cyst formation involving the metacarpophalangeal joints. This condition also often shows chondrocalcinosis.
Hemochromatosis leads to osteophytes with extensive cyst formation involving the metacarpophalangeal joints. This condition also often shows chondrocalcinosis.
Osteoarthritis of the Toes
The commonest causes of degenerative changes in the toe joints are malpositioned toes, especially the hallux valgus (Fig. 9.49). A striking finding of degenerative changes due to hallux valgus deformity is the often extreme hyperostosis and ‘cystoid’ osseous transformation in the first metatarsal head. Accompanying soft-tissue swelling (bursitis) is a frequent additional finding.

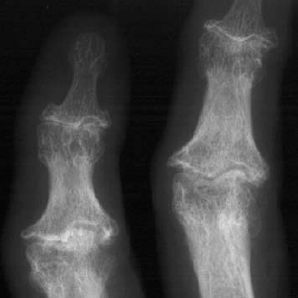
Fig. 9.46 Prominent Bouchard osteoarthritis of the proximal interphalangeal joints, and also less pronounced Heberden osteoarthritis of the distal interphalangeal joints.
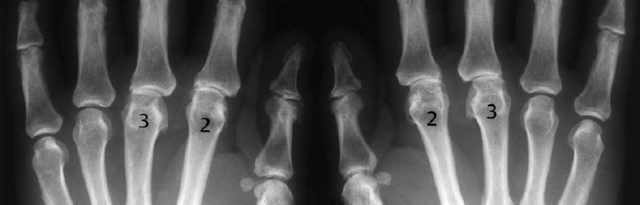
Fig. 9.47 Rare form of atrophic osteoarthritis. The joint spaces are asymmetrically narrowed.
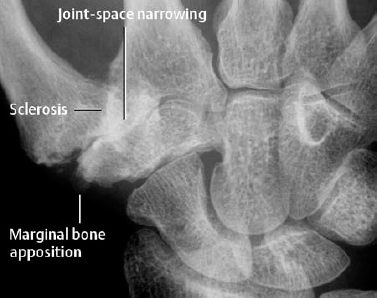
Fig. 9.48 Osteoarthritis of the first carpometacarpal joint.

Fig. 9.49 Hallux valgus with mild degenerative changes.
Degenerative Changes of the Spine
Degenerative disease of the spine is one of the most common clinical entities and affects the intervertebral disks, including apposing vertebral end plates, intervertebral (facet) articulations, and atlanto-axial articulation. Intervertebral and atlanto-axial articulations are genuine synovial articulations and consequently show the same basic abnormalities seen with degenerative disease of synovial articulations found at other sites in the body The most severe primary spinal degenerative changes are found in the lower cervical and lumbar spine regions. Degenerative intervertebral joint disease can occur both separate from and together with degenerative disk changes. Secondary degenerative changes may result from articular misalignment, abnormal distribution of load-bearing following trauma, inflammations, congenital dysplasias or developmental malformations, metabolic and hematologic conditions, or osteonecroses.
Four basic manifestations of spinal degenerative changes are distinguished:
- spondylosis deformans,
- (osteo)chondrosis (intervertebral disk degeneration),
- apophyseal (facet) joint osteoarthritis and uncovertebral osteoarthritis,
- ligamentous calcifications and ossifications.
 a) Changes of the Intervertebral Disk (Chondrosis)
a) Changes of the Intervertebral Disk (Chondrosis)
The intervertebral disk consists of the nucleus pulposus, anulus fibrosus, and cartilaginous end plates (Fig. 9.50). Its major functions are to distribute axial loading and to keep surrounding ligaments taut. The degenerative process causes Assuring and fragmentation of the otherwise spirally intertwined collagenous fibers. The fibers might only partially withstand the high pressure of the nucleus pulposus (7 x atmospheric pressure). Repetitive overloading results most commonly in slowly developing herniation of the nucleus pulposus. However, acute herniations also rarely occur. In principle, the herniation can occur in any direction, but only posterior herniations are clinically relevant, since these are the only ones that compress the nerves or spinal cord, depending on whether the herniation is central or lateral in location.
Protrusion: Bulging of the disk (nucleus pulposus and anulus fibrosus). The nucleus pulposus extends into crevices of the inner zone of the anulus fibrosus and displaces fibers of the peripheral zone (Fig. 9.52).
Prolapse: Material of the nucleus pulposus leaves the anulus pulposus and extrudes through tears in the peripheral zone of the anulus fibrosus (Fig. 9.53).
Sequester: Displaced disk material is referred to as a sequestered fragment. This is usually accompanied by a tear in the posterior longitudinal ligament, but a sequestered fragment can remain subligamentous in location. Its differentiation from a prolapse is problematic, since it is only possible if discontinuation can be demonstrated between disk and sequester (rare) (Fig. 9.54).
Furthermore, disk material can herniate superiorly and inferiorly into the adjacent vertebral bodies. These herniations are called Schmorl’s nodes.
In the process of degeneration, the disk loses water and decreases in height (Fig. 9.51). Furthermore, calcifications may be seen within the disk.
As the degenerative process progresses, reparative osseous processes involving the disk begin at the periphery, where there are no cartilaginous plates. This reparative osseous tissue grows into the disk and can lead to revascularization of the disk (the disk is partially vascularized until the fourth year of life). It is conceivable that this process removes pre-existing disk herniations.
 Neurosurgical terminology distinguishes between ‘hard’ and ‘soft’ prolapses in the cervical spine. Since all types of spinal stenosis caused by calcified tissue (spondylophytes, calcified disks) are referred to as ‘hard prolapses’ this term is pathologically incorrect. However, classifying all of these conditions under a single term appropriately considers the presentation as a chronic encroachment of clinically undetermined cause.
Neurosurgical terminology distinguishes between ‘hard’ and ‘soft’ prolapses in the cervical spine. Since all types of spinal stenosis caused by calcified tissue (spondylophytes, calcified disks) are referred to as ‘hard prolapses’ this term is pathologically incorrect. However, classifying all of these conditions under a single term appropriately considers the presentation as a chronic encroachment of clinically undetermined cause.
In contrast, the ‘soft prolapse’ corresponds to encroachment produced by tissues of soft-tissue consistency and generally presents clinically with acute symptoms.
b) Changes of the Vertebral End Plates
The intervertebral disk is avascular in adolescents and adults and is nourished by diffusion from adjacent bone marrow and bordering ligaments.
In the process of natural aging, the nucleus pulposus loses its water retention capacity, and its internal pressure decreases. This shifts weight bearing from the center to the lateral, leading to ligamentous loosening, and the limited elastic vertebral bone adjacent to the disk is subjected to increased compressive loads. This can result in microedema, microhemorrhage, microfractures, and micro-necroses similar to the processes occurring in synovial joints.
This is followed by reactive changes with pseudo-inflammatory reactions in the subdiskal skeletal zones: hyperemia, and ingrowth of fibrovascular tissue. The outcome is subdiskal fibrosis and sclerosis as the bone attempts to counteract the increased axial pressure. The sclerotic bone is brittle and can collapse, resulting in tears and clefts and the formation of reparative connective tissue.
Instability with ligamentous loosening caused by the decreased pressure within the nucleus pulposus leads to reactive osseous proliferations, referred to as osteophytes, along the margin of the vertebral body (spondylosis deformans) and possibly to hypertrophy of the ligamenta flava. This process serves to counteract the instability. The same applies to the uncovertebral joints of the cervical spine (uncovertebral osteoarthritis or arthrosis). They prevent lateral displacement of the cervical vertebral bodies. The superiorly projecting uncinate processes are a peculiarity of the cervical spine and, in contrast to the dorsal and lumbar spine, form a vertical articulation. The uncovertebral joints are not synovial joints.
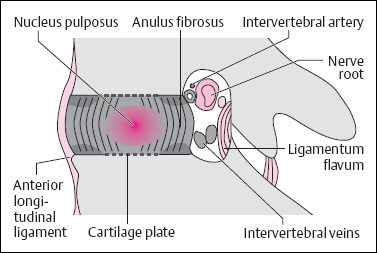
Fig. 9.50 Schematic drawing of the intervertebral disk and intervertebral foramen.
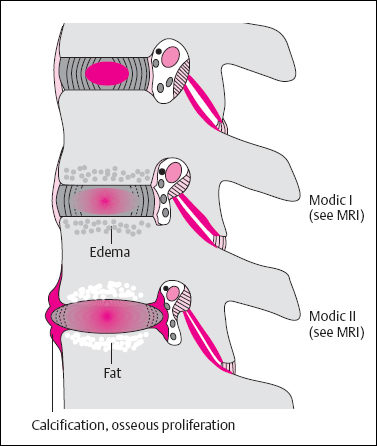
Fig. 9.51 Schematic drawing of disk degeneration, skeletal changes along the disk, and increasing intervertebral degenerative changes. Modified after Gutmann.
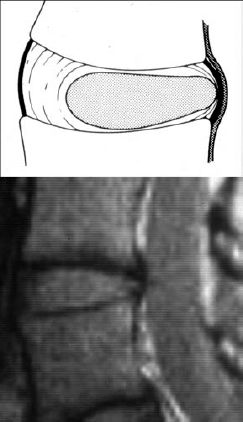
Fig. 9.52 Disk protrusion (GE sequence).
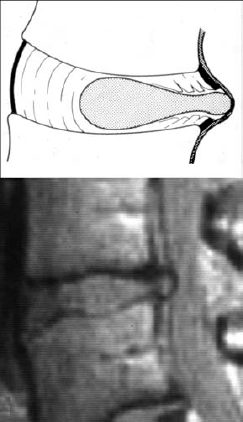
Fig. 9.53 Disk prolapse (GE sequence).
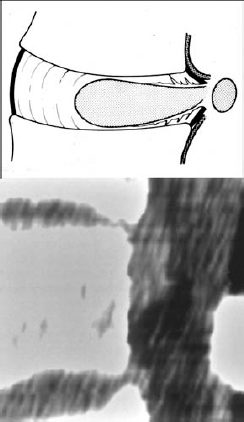
Fig. 9.54 Disk prolapse with interiorly dislocated sequestrum, sagittal CT reconstruction.
c) Changes to the Intervertebral Articulations
The basic pathophysiologic processes are the same as those that occur in other synovial joints. Neck and back pain frequently arise in the intervertebral articulations (synovial irritation, capsular and ligamentous laxity).
Degeneration of these joints is called facet (apophyseal) joint osteoarthritis. The atlanto-occipital and atlan-to-axial joints are also subject to the same process. The pathologic findings correspond to those of osteoarthritis (cartilage damage, subchondral sclerosis, and cyst formation). Characteristic abnormalities are deformed articular surfaces and massive osteophytic overgrowth that can lead to clinically relevant encroachment upon the intervertebral foramina (Figs. 9.55–9.57).
Synovial cysts consist of intraspinal, extradural protrusions of the joint capsule of osteoarthritically deformed intervertebral joints. They are invariably confined to the levels L3-S1 and contain joint fluid or, rarely, gas.
In the lumbar spine, especially at the L4/L5 segment, the degenerative changes can cause anterior gliding of a vertebra relative to its subjacent vertebra (degenerative or pseudospondylolisthesis, Fig. 9.58). This can cause spinal stenosis. In contradistinction, spondylolisthesis is caused by vertebral gliding because of a bilateral defect in the pars interarticularis (spondylolysis). Since in ‘genuine’ spondylolisthesis only the vertebral body glides, and the posterior vertebral arch, together with the spinal process, remains in place, the spinal canal is not narrowed. Etiologically, spondylolisthesis is generally congenital or traumatic (stress fracture).
d) Ligamentous Calcifications and Ossifications
Calcification and ossification of the longitudinal spinal ligaments (anterior and posterior ligaments, ligamentum flavum) are commonly encountered (Figs. 9.59, 9.60). Although this alteration increases after 50 years of age, it has a racial preference (increased incidence of calcifications in the posterior longitudinal ligaments in Asians) and shows quite a variable individual severity, suggesting not only simple ‘degeneration’ but also a genetic disposition. Diffuse idiopathic skeletal hyperostosis (DISH) has pathologic and radiographic findings that are identical to ligamentous calcifications and ossifications of other types, but it is nonetheless considered a distinct entity because of several unique features.
e) Stenosis of the Spinal Canal
In spinal stenosis, a distinction should be made between the central and lateral types. The lateral type involves lateral recess and intervertebral foramen. Congenital spinal canal stenosis is rare, and the acquired form is common.
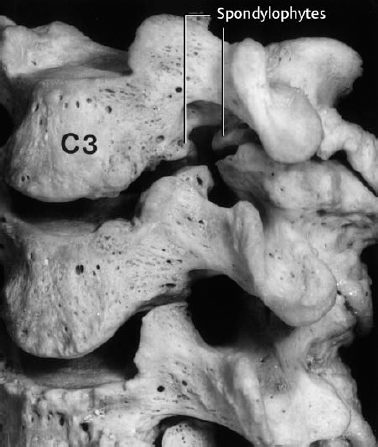
Fig. 9.55 Massive narrowing of the C3-C4 intervertebral foramen by osteophytes of the facet joints and uncovertebral joints.
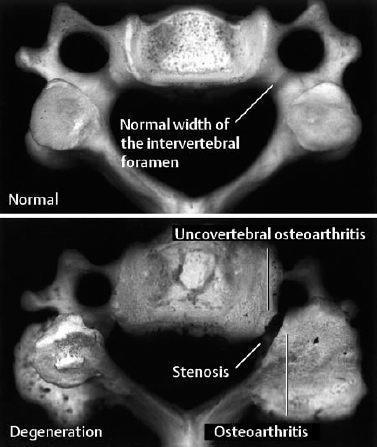
Fig. 9.56 Specimen of a cervical vertebra with uncovertebral and facet joint osteoarthritis, compared with the specimen of a normal cervical vertebra.
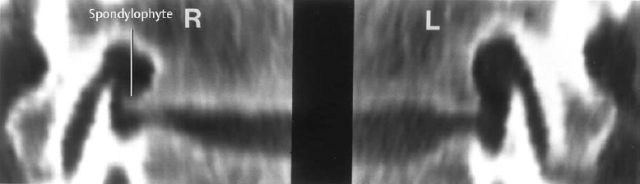
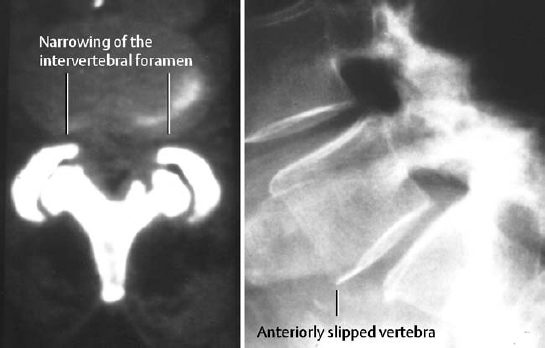
Fig. 9.58 Marked degenerative changes of the facet joints. In addition to narrowing of the intervertebral foramen, there is degenerative anterior slippage of the involved vertebrae (pseudo-spondylolisthesis).
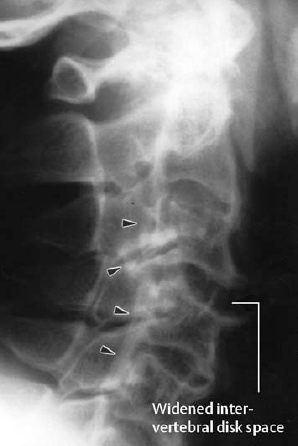
Fig. 9.59 Ossification of the posterior ligaments (arrowheads) with fracture. The fracture is recognized by the discontinuity of the ligament and the widening of the disk space.
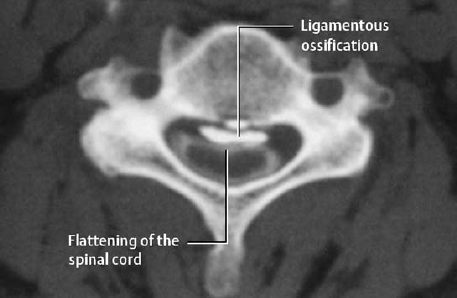
Fig. 9.60 Ossification of the posterior ligament with indentation of the spinal cord (myelo-CT).
- the usually acutely presenting and often recurrent radicular pain syndrome.
Nerve root compression with radicular pain is caused by disk herniations, but also by osseous narrowing of the intervertebral foramina as part of facet joint osteoarthritis and uncovertebral osteoarthritis. The L3 to SI segments are the most frequently involved. In general, the sensory deficits dominate in the form of radicular pain, hypoes-thesia, and possible hypoalgesia. The strictly radicular distribution usually enables a precise clinical determination of the causative level (Table 9.3).
When correlating the radicular symptom complex with the expected radiographic findings, it should be kept in mind that the inferiorly extending lumbar roots begin medial to the cauda equina and then curve laterally to leave the spinal canal through the intervertebral foramen below the corresponding vertebral arch. This means that, for instance, L5 radicular pain can be caused by either a lateral or intraforaminal disk herniation at L5/S1 or a medial disk herniation at L4/L5. In the latter instance, a mixed symptom complex can be, but is not inevitably, present.
 Both skeletal and neurologic symptoms can have quite discrepant clinical and radiographic presentations. The clinical presentation is the deciding factor.
Both skeletal and neurologic symptoms can have quite discrepant clinical and radiographic presentations. The clinical presentation is the deciding factor.
| Root | Sensory impairment | Motor impairment |
|---|---|---|
| L3 | Anterior thigh | Quadriceps (weakened knee jerk) |
| L4 | Anterior lower leg | Quadriceps and tibialis anterior (weakened knee jerk, impaired foot elevation) |
| L5 | Lateral lower leg, extending obliquely to the anterior foot and first toe | Extensor hallucis longus (dorsiflexion of the first toe) |
| S1 | Lateral thigh, posterior lower leg, lateral foot to the fifth toe | Peroneus brevis and triceps (tiptoeing and pronation impaired) |
Disk Degeneration (Chondrosis, Osteochondrosis)
 The evaluation of disk herniation is still the subject of ongoing discussion, but the following conclusions can be drawn so far:
The evaluation of disk herniation is still the subject of ongoing discussion, but the following conclusions can be drawn so far:
- Imaging for the evaluation of ‘back pain’ is frequently applied too uncritically and not selectively enough.
- Diffuse back pain as such is not an indication for indiscriminate imaging.
- Neurologic symptoms are a foremost indication for the use of imaging.
 The basic findings of disk degeneration are (Figs. 9.61, 9.62):
The basic findings of disk degeneration are (Figs. 9.61, 9.62):
- disk-space narrowing (= chondrosis),
- subchondral sclerosis (rarely osteoporosis),
- Schmorl’s nodes,
- spondylophytes,
- vacuum phenomenon,
- calcifications in the disk (nucleus pulposus).
The vacuum phenomenon is caused by the release of nitrogen into the degeneratively altered disk.
Osteochondrosis: The combination of altered ver tebral end plates (band-like sclerosis, contour ir regularities) and narrowed disk space.
The term ‘erosive’ osteochondrosis is used when the end plates show surface irregularities. ‘Serrations’ or contour defects (‘erosions’) are seen radiographically.
In these cases, differentiating this diagnosis from infectious spondylitis is difficult radiographically. A crucial discriminating criterion is the type of accompanying sclerosis: the subdiskal sclerosis is band-like in osteochondrosis and more focal in infectious spondylitis. Moreover, infectious spondylitis lacks other signs of disk degeneration. In cases of suspected infection superimposed on an (erosive) osteochondrosis, MRI is the preferred imaging modality.
Osteochondrosis and facet joint osteoarthritis of the cervical spine cause hypomobility, preferentially located at levels C5 to C7, frequently with hyper-mobility of higher cervical segments.
Hemispheric spondyloschisis: This term coined by Dihlmann describes a hemispheric spongiosal sclerosis in the anterior or middle third of the vertebral body above an intervertebral disk that appears radiographically normal or narrowed. We consider this a special manifestation of the (normally band-like) subchondral sclerosis as frequently seen with disk degeneration. Awareness of this special manifestation is important for the differential diagnosis when the apposing subdiskal end plate fails to show a sclerosis in the presence of a normal disk space. The hemispheric spongiosal sclerosis must be distinguished from increased density caused by infectious spondylodiskitis (use MRI). Osteoblastic metastases (Fig. 9.63) pose difficulty only if the spine shows additional degenerative changes together with a solitary metastatic lesion (rare).

Fig. 9.61 Degenerative changes of the lumbar spine with marginal osteophytes, end-plate sclerosis, and disk-space narrowing. The osseous appositions are most severe where the vertebral bodies show a decrease in height.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Osteoarthritis is a destructive joint disease, primarily caused by damaged cartilage – regardless of the nature of the cartilage damage. Arthritis is a destructive joint disease primarily caused by synovitis – regardless of the nature of the synovitis.
Osteoarthritis is a destructive joint disease, primarily caused by damaged cartilage – regardless of the nature of the cartilage damage. Arthritis is a destructive joint disease primarily caused by synovitis – regardless of the nature of the synovitis. 
 Pathologic alterations at the osseous attachment of tendons, ligaments, and joint capsules are referred to as enthesopathies. They consist both of degenerative-reparative phenomena (fibro-ostosis) and inflammatory reactions (fibro-ostitis). Both processes can lead to hyperostosis with spur formation, as well as to osseous resorption. The corresponding osseous changes in the spine are referred to as syndesmophytes and parasyndesmophytes.
Pathologic alterations at the osseous attachment of tendons, ligaments, and joint capsules are referred to as enthesopathies. They consist both of degenerative-reparative phenomena (fibro-ostosis) and inflammatory reactions (fibro-ostitis). Both processes can lead to hyperostosis with spur formation, as well as to osseous resorption. The corresponding osseous changes in the spine are referred to as syndesmophytes and parasyndesmophytes. 
 Degenerative joint diseases (= osteoarthritis) include many different conditions and often undetermined etiologies. They all have in common that they occur at an older age (in the fifth decade of life or later = primary osteoarthritis) or as secondary osteoarthritis following a pre-existing joint disorder. Secondary osteoarthritis can also occur early in life. Current scientific evidence indicates that primary osteoarthritis and aging are conceptually two separate processes. This is supported by both biochemical and histologic investigations.
Degenerative joint diseases (= osteoarthritis) include many different conditions and often undetermined etiologies. They all have in common that they occur at an older age (in the fifth decade of life or later = primary osteoarthritis) or as secondary osteoarthritis following a pre-existing joint disorder. Secondary osteoarthritis can also occur early in life. Current scientific evidence indicates that primary osteoarthritis and aging are conceptually two separate processes. This is supported by both biochemical and histologic investigations. 
 Atrophic destructive osteoarthritis must be differentiated from Charcot joint: the neuropathic destruction also involves other joints of the affected extremity.
Atrophic destructive osteoarthritis must be differentiated from Charcot joint: the neuropathic destruction also involves other joints of the affected extremity. A basic distinction must be made between – the usually chronic and diffuse ‘back pain’, caused by spondylosis deformans, facet joint osteoarthritis, and uncovertebral osteoarthritis. As with osteoarthritis of peripheral joints, restricted motion and pain on weight bearing dominate the clinical presentation;
A basic distinction must be made between – the usually chronic and diffuse ‘back pain’, caused by spondylosis deformans, facet joint osteoarthritis, and uncovertebral osteoarthritis. As with osteoarthritis of peripheral joints, restricted motion and pain on weight bearing dominate the clinical presentation;