Normal Anatomy
Kidneys
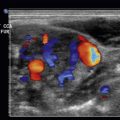
The kidneys are retroperitoneal structures and are surrounded by fascial layers, including Gerota’s fascia. There is direct supply of the renal arteries and veins to the kidney from the abdominal aorta. The right and left renal arteries lie posterior to the renal veins. Their relationship to each other and the surrounding vascularity is shown in Fig. 19.1 . The kidneys consist of the renal parenchyma, which is divided into the outer cortex and the inner medulla. Most of the cortex is peripheral to the medulla, except for the columns of Bertin, which are portions of the cortex that extend between the medullary pyramids. More centrally, the calyces, infundibulum, and renal pyramids are conduits delivering urine to the ureters ( Fig. 19.2 ). The kidneys are approximately 11 cm long in adults, but vary in length from 9 to 12 cm. The renal veins and arteries can be identified with color flow ( ![]() ).
).


Ureters/Bladder
The ureters are small tubules connecting the retroperitoneally located kidneys to the urinary bladder. In most situations, only the proximal ureter, at the ureteropelvic junction, and the distal ureter, at the ureterovesicular junction, are visualized by ultrasound. The bladder lies deep in the pelvis. The bladder is oval in shape with the ureters entering the posterior lateral bladder wall. More distally, the bladder exits through the urethra. The normal bladder wall is approximately 4 to 6 mm in thickness and is smooth, but bladder wall thickness can increase with inadequate bladder filling. In males, the prostate is seen at the bladder base. In females, the uterus is seen deep to the posterior bladder wall. The urethra in the male is divided into the prostatic, membranous, and penile segments. The female urethra is shorter. Neither is well identified with transabdominal imaging.
Normal Ultrasound Findings/Techniques
Kidney
The kidneys can be imaged with the patient supine, using the liver and spleen as acoustic windows. The left kidney is more problematic to image due to the spleen providing a smaller acoustic window compared with the liver. The upper pole of the left kidney is often a “blind spot,” as there is no ideal window for visualization. At times the kidneys, especially the left kidney, may be best visualized with the patient prone. As the superior pole of each kidney is located more medially than the lower pole, the transducer must be angled obliquely to capture the true long axis of the kidney. The kidneys should be scanned in both longitudinal and transverse planes. After longitudinal scanning, the transducer is rotated 90 degrees to the transverse plane, so that both the lower and upper poles of the kidney may be scanned in their entirety. Kidney length typically ranges from 9 to 12 cm, with the right kidney often slightly larger than the left.
The kidneys are usually less echogenic than the liver or spleen. The renal medulla is often hypoechoic compared with the renal cortex, whereas the renal sinus fat is more echogenic than the pyramids. The renal hilum is central and more echogenic than both the cortex and the medulla. The echogenicity is due to the renal sinus fat. The ureter, arteries, and veins are located in the renal hilum. When appropriate settings are used, the entire kidney will fill with color ( Fig. 19.3 ).

Certain anatomic variants of the kidney may mimic a renal mass. The kidneys are usually smooth in contour but may have lobulations. These lobulations, when they occur, are numerous and affect both kidneys. There may be a region of prominent cortex or bulge seen in the midportion of the left kidney. This has been termed a dromedary hump . This “hump” usually appears as a focal bulge in the left side of the kidney, probably secondary to compression by adjacent structures such as the spleen. This “hump” may be mistaken as for mass ( Fig. 19.4 ). Portions of the cortex extending deep between the medullary pyramids as a column of Bertin may be mistaken for a mass as well. Careful scanning and knowledge of the sonographic appearance of the kidneys will help avoid these pitfalls.

Ureter
The proximal ureter is best visualized in a coronal oblique view using the kidney as an acoustic window. The ureter is very difficult to follow to the bladder because of overlying bowel gas. However, the proximal ureter often can be identified at the ureteropelvic junction. More distally, the ureter can be visualized with a full bladder technique, which may be helpful to identify distal ureteric stones or to see anomalies at the ureterovesicular junction, such as an ureterocele. Additionally, the distal ureter may be identified in women with a transvaginal approach. Color flow ultrasound is useful to identify the distal ureters entering the bladder as color “jets,” where the urine enters into the bladder ( Fig. 19.5 ). If these are present, this identifies the ureteric orifice and demonstrates there is no complete ureteric obstruction.

Bladder
The bladder is best evaluated when moderately filled. With underdistention of the bladder, there is suboptimal visualizing of the bladder, bladder masses, or surrounding pelvic structures. Alternatively, an overdistended bladder may cause patient discomfort, which can make scanning difficult. The bladder should be scanned in both the transverse and parasagittal planes. There is constant peristalsis of the ureters as they enter the bladder. Flow of urine from the ureter into the bladder is observed as ureteral “jets” in the bladder with color Doppler ultrasound (see Fig. 19.5 ). Often, a Foley catheter has been placed in acutely ill patients, introducing a small amount of air into the bladder and making visualization of the bladder or its contents difficult or nearly impossible. As noted previously, the bladder even partially filled may be visualized utilizing a transvaginal approach in women.
Acute Flank Pain
There are enumerable etiologies of flank pain. Some of these are listed in Table 19.1 . The renal etiologies can be basically divided into extraparenchymal renal etiologies and renal parenchymal disease. The major causes that may be detected by ultrasound are often extraparenchymal disease, such as hydronephrosis or stone disease. Parenchymal causes of pain include pyelonephritis, abscess, or renal cysts/masses.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other etiologies, such as musculoskeletal pain or local trauma, may require nonsonographic methods for detection. Structures that surround the kidney may be the etiology of flank pain.
Hydronephrosis
Although dilatation of the renal collective system usually implies obstruction, dilatation may be secondary to ureteral reflux. A rare abnormality that results in renal dilatation is diabetes insipidus. Different etiologies of renal collecting system dilatation are listed in Table 19.2 .
|
|
|
|
|
|
|
|
|
The level of obstruction and the etiology of the hydronephrosis can often be diagnosed by sonography. Proximal renal obstruction is most commonly due to stones, but rarely tumors such as a transitional cell carcinoma. If there is ureteric dilatation, then the bladder should always be scanned to potentially diagnose the bladder as the site of obstruction. This is discussed in more detail in the “Bladder” section of the chapter.
There are a variety of different methods of classifying hydronephrosis. In the adult, most hydronephrosis is classified as mild, moderate, or severe ( Figs. 19.6 and 19.7 ). However, in the newborn and pediatric patient, there are other classifications, including that of the Society of Fetal Surgery that grades hydronephrosis from grade 1 to grade 4.

In mild hydronephrosis, there may be more central dilatation of the renal pelvis, with minimal calyceal dilatation. Moderate hydronephrosis in the adult is characterized by more pronounced dilatation of the renal pelvis and progressive dilatation of the calyceal system. The outer cortex is preserved ( Fig. 19.7 , ). Severe hydronephrosis in adults is characterized by more pronounced dilatation of the renal collecting system, as well as marked dilatation of the calyceal system. In these situations, there is distortion of the medullary pyramids and thinning of the renal cortex ( ![]()
![]() ).
).
There are a few pitfalls in the diagnosis of hydronephrosis. These include parapelvic cysts that may mimic hydronephrosis. The cysts are located within the renal pelvis and are fairly smooth walled and rounded or oval. These cysts are fairly localized, except in cases where there are multiple parapelvic cysts, which may mimic hydronephrosis ( Fig. 19.8 ).

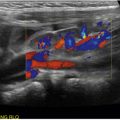
The parapelvic vessels, especially the parapelvic veins, may be mistaken for a dilated renal pelvis. These vessels are easily distinguished from a dilated renal pelvis by use of color flow ultrasound, which clearly demonstrates these are vascular structures ( Fig. 19.8 ).
Finally, there are different degrees of prominence of the renal pelvis, with some patients having an extra renal pelvis. This may be the normal baseline in these patients, and this should not be confused with hydronephrosis. Comparison with prior studies is often helpful for this distinction.
Renal Stones
Renal stones may be obstructive or nonobstructive. Nonobstructive renal stones appear as an echogenic focus in the kidney. Renal stones are usually composed of calcium oxalate or phosphate. If large enough, they cast an acoustic shadow. Shadowing may be better demonstrated by using a higher-frequency transducer and adjusting the focal zone. Stones will also produce a “twinkle” artifact with color Doppler, seen as alternating color posterior to the stone, compared with the more homogenous color flow of veins and arteries ( Fig. 19.9 , ![]() ).
).

Stones may cause obstruction and are a common etiology of flank pain. As discussed previously, obstructing stones associated with hydronephrosis are seen as an echogenic focus with acoustic shadowing. Stones also lodge distally at the ureter–pelvic junction (UPJ). These stones may be seen with transabdominal scanning through the bladder (see Fig. 19.10 ). Color flow is useful to show the “twinkle” artifact of the stone. If there is complete ureteral obstruction, no color “jet” will be seen. With partial obstruction a “jet” is still present ( Fig. 19.10 ). Rarely, on transvaginal ultrasound, distal ureteric stones may be identified.

Pitfalls of Renal Stones
There are mimics of renal stones. These include vascular calcifications that appear as linear, closely spaced reflections. Although less likely to produce acoustic shadowing, if severe enough, shadowing may be observed with vascular calcifications. Renal sinus fat is more diffuse and should not be confused with renal stones. Usually, the renal medulla is hypoechoic to the renal cortex. However, with renal nephrocalcinosis, the medulla appears to be diffusely echogenic and should not be confused with renal stones, which are a more focal process.
Pyelonephritis
Patients with acute flank pain may be suffering from renal obstruction, but if there is pyuria, or evidence of infection, pyelonephritis may be considered. Acute pyelonephritis is an infection of the renal parenchyma and collecting system most commonly secondary to lower urinary tract infection. The etiology is usually a bacterial infection from Escherichia coli . With mild pyelonephritis, the kidney may appear sonographically normal. There may be some perinephric fluid, renal enlargement, and decreased visualization of the renal sinus fat. Focal pyelonephritis may result in areas of decreased or increased echogenicity ( Fig. 19.11 , ![]()
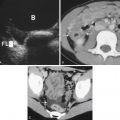
![]() ). There also may be decreased distinction of the renal medulla and cortex. In these situations there may be swelling of a portion of the renal parenchyma, resulting in a differentiation from the rest of the renal parenchyma. This region is usually avascular ( ). With treatment of pyelonephritis, the kidney will eventually appear normal. Contrast-enhanced computed tomography (CT) is more sensitive than ultrasound in demonstrating focal pyelonephritis. Contrast-enhanced ultrasound shows promise in the detection of pyelonephritis. Eventually, these focal areas of pyelonephritis can resolve or develop into renal abscesses. These are usually hypoechoic and avascular areas within the kidney ( Fig. 19.12 ). Color flow may demonstrate surrounding hyperemia. Contrast-enhanced CT or contrast-enhanced ultrasound may be helpful to better identify focal pyelonephritis or a focal renal abscess (see Fig. 19.12 ).
). There also may be decreased distinction of the renal medulla and cortex. In these situations there may be swelling of a portion of the renal parenchyma, resulting in a differentiation from the rest of the renal parenchyma. This region is usually avascular ( ). With treatment of pyelonephritis, the kidney will eventually appear normal. Contrast-enhanced computed tomography (CT) is more sensitive than ultrasound in demonstrating focal pyelonephritis. Contrast-enhanced ultrasound shows promise in the detection of pyelonephritis. Eventually, these focal areas of pyelonephritis can resolve or develop into renal abscesses. These are usually hypoechoic and avascular areas within the kidney ( Fig. 19.12 ). Color flow may demonstrate surrounding hyperemia. Contrast-enhanced CT or contrast-enhanced ultrasound may be helpful to better identify focal pyelonephritis or a focal renal abscess (see Fig. 19.12 ).