Kidneys
Michael Blaivas
INTRODUCTION
Frequently viewed by emergency physicians as part of other ultrasound examinations, ultrasound of the kidneys is often overlooked as a valuable diagnostic tool. With computed tomography (CT) readily available in many institutions, renal ultrasound is often thought of as a second-line modality (1). However, a focused renal ultrasound can give valuable and rapid information at the bedside about renal obstruction. Consequently, once proficient at this exam, the emergency physician has a powerful tool in the evaluation of flank, abdominal, and pelvic pain. Recent years have seen the recognition that excess medical radiation is not only costly, but also dangerous as seen by expected increased future cancer rates among patients receiving multiple imaging studies, including CT, intravenous pyelograms (IVP), and plain radiography. This provides additional strength to arguments for the use of ultrasound by emergency physicians that can be used to gain support from hospital administration for start-up ultrasound programs.
CLINICAL APPLICATIONS
The primary clinical utility of focused renal ultrasound in the emergency setting is for evaluation of acute flank pain, abdominal pain, and hematuria (2). After appropriate training, emergency physicians can learn to identify hydronephrosis and intrarenal stones (3). The detection of hydronephrosis supports a clinical diagnosis of renal colic and possibly ureteral obstruction (4). The presence of bilateral hydronephrosis, in contrast, may be an important clue to a pelvic mass or bladder outlet obstruction such as occurs with benign prostatic hypertrophy, prostate cancer, and bladder cancer (5). The absence of hydronephrosis in the face of acute abdominal pain may, in some cases, lead the clinician to an alternative diagnosis.
Assessment of ureteral jets in the bladder may give additional information regarding ureteral obstruction and its degree. Further, evaluation of the bladder is being emphasized more than ever due to an increased recognition of bladder infection after catheterization. Evaluation of postvoid residual, still a necessary procedure in the emergency department (ED), can be accomplished solely with ultrasound. Additionally, unnecessary catheterization of empty bladders can also be avoided, and is especially problematic in young children who cannot communicate whether their bladders are full or empty.
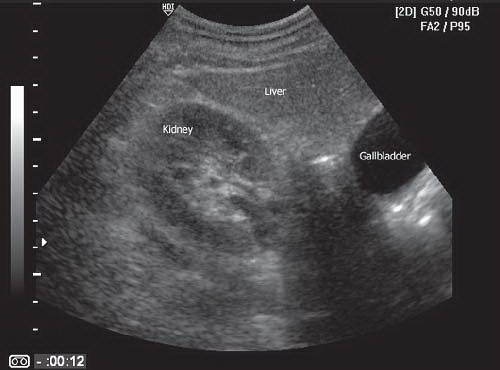
In addition, renal ultrasound may aid the clinician in the initial assessment of acute renal failure to rapidly detect bilateral obstruction, which could lead to salvage of renal function (6). This is especially true in patients who may not be able to provide their own histories or make complaints. Such patients may suffer a bladder outlet obstruction and subsequent renal failure without anyone knowing the patient has any discomfort. The clinical presentation of renal colic, pyelonephritis, biliary colic, and aortic aneurysm may overlap. Thus, the renal ultrasound examination will often flow into evaluation of other structures such as the gallbladder, liver, common bile duct, and aorta to detect other possible etiologies of acute pain. Once proficiency has been achieved, this simple bedside assessment for hydronephrosis can expedite the evaluation and treatment for many patients with complaints of flank and abdominal pain.
IMAGE ACQUISITION
The ability to obtain quality renal images is one of the easier skills to master in emergency sonography (2). Both kidneys are relatively superficial; both are located adjacent to solid viscera (liver, spleen) that provide favorable acoustic windows. In addition, the kidneys are often used as reference structures for other abdominal ultrasound examinations, particularly the trauma or Focused Assessment with Sonography for Trauma (FAST) scan. It is important, nonetheless, to follow the same basic principles of all ultrasound examinations: scan slowly, scan methodically, and image in at least two planes in order to conceptually convert two-dimensional information into three-dimensional mental images.
Patient Preparation
Patients requiring emergency renal ultrasounds are often in considerable pain, especially those with renal colic. In order to obtain an adequate examination, it is essential that pain be controlled. It will be necessary for the patient to cooperate with instructions to position themselves and control their respiratory rate and pattern upon request by the sonographer. Movement by the patient should be minimized if possible, and some renal colic patients cannot remain still enough without analgesia.
The kidneys are best visualized in a fasted and hydrated patient (7). However, this is not always possible in the emergency setting. Bowel gas, ideally absent in the fasted patient, can present considerable interference during a renal ultrasound examination. Hydration status also affects the sonographic appearance of the kidney and bladder. Indeed, the state of hydration can mislead the examiner when attempting to determine the presence or absence of hydronephrosis. A well-hydrated patient may have a dilated renal pelvis that appears similar to mild hydronephrosis (8). A markedly dehydrated patient with obstruction may not demonstrate a dilated renal collecting system (9).
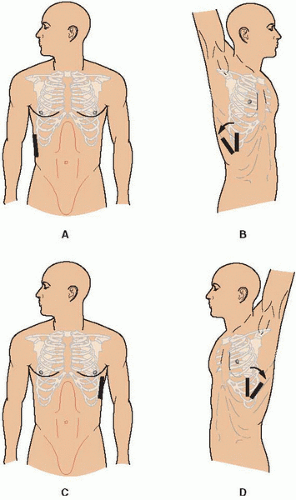
Most sonographers begin with the patient in a supine position similar to that used for general abdominal scans (Figs. 11.1 and 11.2). This position provides the most
intuitive location for anatomical structures when imaged with ultrasound. In order to build a three-dimensional mental image of the kidney from two-dimensional frames, all of the anterior, posterior, superior, inferior, medial, and lateral relationships of the kidney must be understood. Relationships between the liver and the right kidney and between the spleen and the left kidney are easy to conceptualize (Fig. 11.3).
intuitive location for anatomical structures when imaged with ultrasound. In order to build a three-dimensional mental image of the kidney from two-dimensional frames, all of the anterior, posterior, superior, inferior, medial, and lateral relationships of the kidney must be understood. Relationships between the liver and the right kidney and between the spleen and the left kidney are easy to conceptualize (Fig. 11.3).
 FIGURE 11.2. A Patient is Seen in the Supine Position. This is the typical starting point for an emergency ultrasound of the kidneys. |
It is important when using the supine view to have the patient lie as flat as possible. When the head or the trunk is elevated, the kidney tends to tuck under the rib margin, making renal imaging more difficult. In some circumstances, however, adequate visualization is not obtainable from the supine position. In these instances the patient can be moved to alternative positions, such as the right and left lateral decubitus or prone positions (Fig. 11.1B, D). In the decubitus position the kidney of interest is elevated, that is, the left lateral decubitus position is used to visualize the right kidney. This allows for better use of both the liver and the spleen as acoustic windows for kidney visualization. The prone position is rarely utilized, but may be necessary occasionally. In this position, a pillow is placed under the abdomen to use the paraspinal muscles as an acoustic window. Often these positions are utilized in a stepwise fashion to obtain the best view of the kidney.
During the renal ultrasound examination, it may be necessary for patients to hold their breath or vary their respirations. When the patient takes a large breath, the expanding lungs push down the diaphragm and kidney toward the pelvis. This allows more of the kidney to be visualized from an anterior or midaxillary approach. Further, rapid breathing can create so much motion that image quality degrades and interpretation is made more difficult. Therefore, it is often necessary for the patient to hold his/her breath, usually at maximal inspiration, especially if motion-sensitive Doppler ultrasound is utilized during the examination.
Imaging Technique
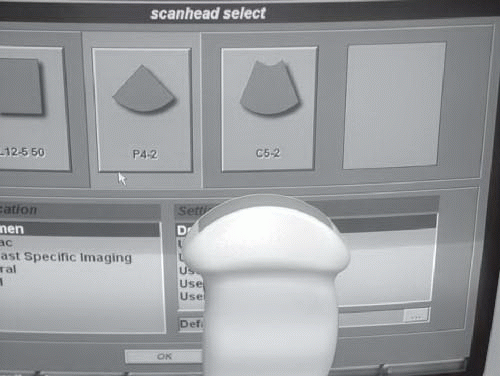
A 3 to 5 MHz curvilinear array transducer commonly used for general abdominal scanning is appropriate for most renal scans as well (Fig. 11.4). This frequency provides a good compromise between adequate penetration and good resolution of renal structures. However, the sonographer should
recognize that small stones that may be encountered in the renal parenchyma might not be visualized at this resolution. Higher frequency transducers, up to 7.5 MHz, may be used if the person is thin or if a small child is being scanned. If a curvilinear array transducer is used, it is important to recognize that only structures directly in line with the footprint of the probe are optimally imaged; thus, structures of interest should be visualized in the central field of the probe. Phased array cardiac probes can be used to image the kidneys as well, but do so better when using an abdominal setting. These transducers perform comparatively well when scanning in between ribs, but tend to give lower quality images than a curvilinear transducer.
recognize that small stones that may be encountered in the renal parenchyma might not be visualized at this resolution. Higher frequency transducers, up to 7.5 MHz, may be used if the person is thin or if a small child is being scanned. If a curvilinear array transducer is used, it is important to recognize that only structures directly in line with the footprint of the probe are optimally imaged; thus, structures of interest should be visualized in the central field of the probe. Phased array cardiac probes can be used to image the kidneys as well, but do so better when using an abdominal setting. These transducers perform comparatively well when scanning in between ribs, but tend to give lower quality images than a curvilinear transducer.
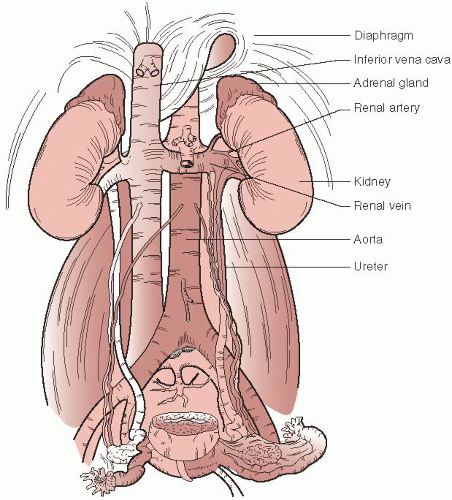 FIGURE 11.3. The Kidneys and Surrounding Structures. Note the relative positions of the aorta, inferior vena cava (IVC), renal vessels, collecting system, and ureters. |
When the standard axillary approach fails to provide a good image, a trans-thoracic approach provides an alternative approach (Fig. 11.5). If the sonographer has a choice, this is when a phased array transducer offers advantages over the curvilinear array transducer; its small footprint facilitates imaging through the narrow rib space, although it offers less definition and a somewhat poorer image quality (Fig. 11.6).
 FIGURE 11.5. The Ultrasound Transducer is Positioned High Over the Patient’s Ribs to Attempt Visualization of the Kidney Through the Intercostal Spaces. |
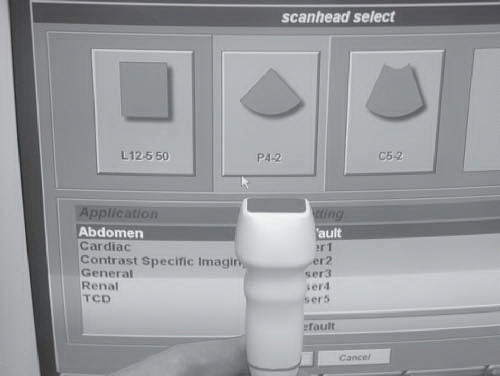 FIGURE 11.6. An Image of a Phased Array Typically Used for Cardiac Ultrasound. But one that can be very useful for imaging the kidneys through tight rib spaces. |
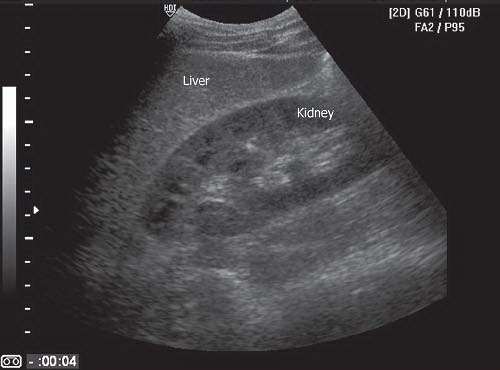
The images required for a renal ultrasound include both the longitudinal and the transverse views through both kidneys (Figs. 11.7 and 11.8). Generally, the contralateral side is imaged first. This is done in order to have a baseline comparison to evaluate the potentially abnormal kidney. Again, each kidney needs to be imaged in at least two planes in entirety and “spot checks” scanning only through a portion of the kidney such as the hilar area are not advisable.
To image the kidney, place the probe below the ribs in the axillary line with the probe indicator at a 12 o’clock position perpendicular to the costal margin (Figs. 11.1A, B and 11.9). Sweep the probe from an anterior to a posterior direction until the kidney is located. It may be necessary in some cases to direct the ultrasound beam cranially, under the costal margin. Once located, rotate the probe until the long axis of the kidney is in full view (Fig. 11.7). In this longitudinal view, the superior pole of the kidney should be on the left side of the ultrasound screen and the inferior pole on the right side of the screen (Fig. 11.10). As the probe is swept in this plane, a three-dimensional construct of the long axis of the kidney can be mentally assembled. In most
cases, the liver or spleen is used as an acoustic window to provide an optimal image of the kidney. A noticeable difference will be appreciated in most cases when the liver or kidney is no longer under the transducer to provide a favorable window. When the transcostal approach is used it is important to position the probe in such a manner as to minimize rib shadowing. It should be noted that the kidneys lie in an oblique orientation relative to the long axis of the body (Fig. 11.3). A true long-axis view of the kidney may require the transducer to be rotated slightly away from the long axis of the body. For the right kidney, the probe indicator more commonly comes to rest at a 10 o’clock position to view the long axis; for the left kidney, the indicator may need to be oriented at 2 o’clock (Figs. 11.1B, D). Once the kidney is visualized, proper images should be based on internal guidelines and not artificial external landmarks. In other words, the image on the screen is matched to a mental image of a standard renal view.
cases, the liver or spleen is used as an acoustic window to provide an optimal image of the kidney. A noticeable difference will be appreciated in most cases when the liver or kidney is no longer under the transducer to provide a favorable window. When the transcostal approach is used it is important to position the probe in such a manner as to minimize rib shadowing. It should be noted that the kidneys lie in an oblique orientation relative to the long axis of the body (Fig. 11.3). A true long-axis view of the kidney may require the transducer to be rotated slightly away from the long axis of the body. For the right kidney, the probe indicator more commonly comes to rest at a 10 o’clock position to view the long axis; for the left kidney, the indicator may need to be oriented at 2 o’clock (Figs. 11.1B, D). Once the kidney is visualized, proper images should be based on internal guidelines and not artificial external landmarks. In other words, the image on the screen is matched to a mental image of a standard renal view.
 FIGURE 11.9. An Ultrasound Transducer is Positioned on the Patient’s Right Side in Preparation for a Renal Scan. |
The transverse position view is obtained by rotating 90 degrees counterclockwise from the longitudinal view (Fig. 11.8). Transverse images of the kidney are made from the cranial to the caudal poles by angling the transducer along the length of the kidney. The hilum (located in the midportion of the kidney) should be imaged to assess the renal artery, vein, and ureter (Fig. 11.11).
The right kidney is usually best imaged near the anterior to mid-axillary line. This kidney is slightly more inferior in location than the left because the right kidney is displaced by the liver. The left kidney is best imaged between the midaxillary line and the posterior axillary line, depending upon the size and location of the spleen (Fig. 11.12).
Once both kidneys are imaged in both the longitudinal and transverse views, comparison views are made. The dual function on the ultrasound allows display of both kidney images on one screen (Fig. 11.13). Similar views of each kidney are obtained. This allows for the comparison of the two kidneys. Labeling of each kidney is essential to prevent confusion.
Before concluding the renal scan, the bladder should also be imaged. The transducer should be placed in the midline just above the pubis and the bladder imaged in two dimensions (Fig. 11.14). The bladder provides additional information that is often relevant to the renal scan. Occasionally, pelvic pathology may be noted that will explain abnormalities detected in the kidneys, such as a dilated (obstructed bladder).
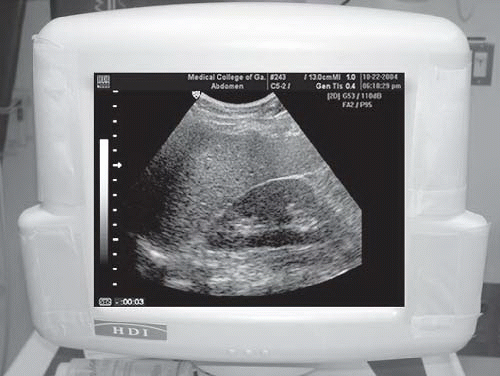
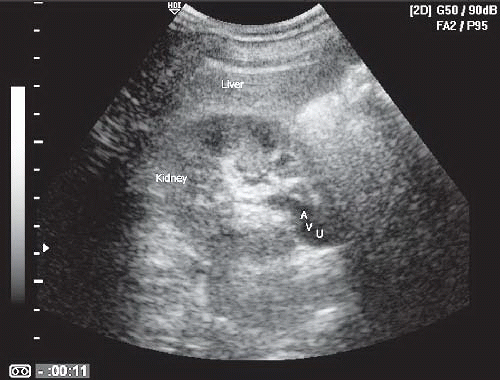 FIGURE 11.11. Short Axis Image of the Right Kidney through the Hilum. The artery (A), vein (V), and ureter (U) are seen exiting the kidney. |
 FIGURE 11.12. The Transducer is Positioned More Posteriorly on the Left Side. This position will be required in many patients. |
NORMAL ULTRASOUND ANATOMY AND LANDMARKS
The kidneys are paired retroperitoneal organs that lie lateral to the aorta and the inferior vena cava and inferior to the diaphragm (Fig. 11.3). The kidneys are bounded by Gerota’s fascia, a tough connective tissue that also surrounds the adrenal glands, renal hila, proximal collecting system, and the perinephric fat. The right kidney is bounded by the liver anteriorly, the liver and diaphragm superiorly, and the psoas and quadratus lumborum muscles posteriorly. The left kidney is bounded by the spleen, large and small bowel, and stomach anteriorly; the diaphragm superiorly; and the psoas and quadratus lumborum muscles posteriorly. Both kidneys lie between the 12th thoracic and the 4th lumbar vertebrae. Usually, the right kidney is located more inferior than the left due to displacement by the liver, but position will vary with changes in posture and respiration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree