How to Image the Knee
See the protocols for knee MRI at the end of this chapter.
MRI of the knee is the most frequently requested MRI joint study in musculoskeletal radiology. The reasons for this are simple: it works, and so referring physicians request it. MRI provides a comprehensive examination of the knee, giving surgeons information they cannot obtain clinically or noninvasively. It also provides a road map for a surgeon performing arthroscopic or open surgery. It has proved to be very accurate, with sensitivity and specificity 90% to 95% for the menisci and close to 100% for the cruciate ligaments. This chapter shows how that kind of accuracy can be obtained.
- •
Coils and patient position: There are many ways to image the knee adequately, with different centers having differing imaging protocols based solely on personal preferences. We not only give which recipes work but also, more importantly, stress what should not be used. As with all joint imaging, a dedicated surface coil must be used. Most centers have a knee coil of some sort, and one seems to work as well as another. (At a cost of $10,000-$20,000 each, they should work well!) A small field of view should be used to maximize resolution. Generally, we use 14 to 16 cm, depending on the size of the patient. Slice thickness can be 3 to 5 mm, with 4 mm being the standard in most centers. A small interslice gap (0.4 mm) is used to reduce cross talk, unless volume imaging is employed. Having slice thickness less than 4 mm does not seem to increase accuracy and leads to more images to interpret, or information overload. A matrix of 256 × 192 or 256 × 256 is standard, with neither being better than the other. We try to have the knee in about 5 degrees of external rotation so that the anterior cruciate ligament (ACL) is orthogonal to the sagittal plane of imaging. This is typically the position of the knee in the relaxed state, and no effort at externally rotating the knee needs to be made in most patients.
- •
Pulse sequences: The menisci are best evaluated using sagittal images. It is necessary to have a short TE to see meniscal tears effectively. This can be in the form of conventional spin echo T1W, proton density, or gradient echo sequences. It has been shown conclusively that fast spin echo (FSE)–proton density (PD) images are unacceptable. Although there seems to be conflicting data on this subject, with several articles touting FSE-PD, and others condemning it, we strongly believe that many meniscal tears are missed using FSE-PD sequences. We compared conventional proton density sequences and FSE-PD sequences in 216 consecutive knees and found that the FSE-PD examination missed 42 tears that were seen on the conventional proton density sequences ( Fig. 15-1 ). Our overall sensitivity for interpreting the menisci using conventional proton density sequences is 90% to 95%; using FSE-PD, our sensitivity was 80%. Why is there such a difference in our results and in those of other investigators? In fact, there is not much difference. If one calculates the sensitivity for meniscal tears in the articles published on this subject, one would find that every publication has a sensitivity of around 80%. It seems all of the articles have the same results; however, the conclusions differ. It makes no sense to us to sacrifice accuracy in finding meniscus tears for the small decrease in imaging time that fast spin echo sequences give. The savings in time do not allow enough of a savings to increase patient throughput, and even if it did, it would not justify missing about 10% of the meniscal tears, which is exactly what happens with FSE-PD sequences. This may change with 3T imaging, but that remains to be seen. For evaluating the menisci, we use a 4-mm-thick sagittal spin echo–proton density sequence that has fat suppression. Fat suppression makes a more esthetic-looking image when looking at the menisci ( Fig. 15-2 ). It increases the range of signal in the menisci and makes tears more conspicuous than without fat suppression. It has not been shown that it increases accuracy (in side-to-side comparison of hundreds of cases with and without fat suppression, we have found no examples of tears seen on one sequence and not on the other). Nevertheless, it gives the reader more confidence and makes for a pretty image, which is not all bad. We also use a 4-mm-thick sagittal FSE-T2W image with fat suppression, which is excellent for examining the cruciate ligaments, cartilage, and bones. A sagittal conventional spin echo–T2W image would suffice similarly, but does not have the same high signal-to-noise ratio or resolution as fast spin echo and takes more time. A STIR image also would suffice. A gradient echo sagittal image (volume or single slice) would do nicely for the cartilage and cruciates, but is unacceptable for examining the bones. Some centers use sagittal gradient echo to replace the T1W and the T2W image in the sagittal plane. This is a considerable time-saving technique. The marrow signal is examined with a marrow-sensitive sequence in the coronal or axial planes. The coronal plane is used to examine the collateral ligaments and serves as another plane to examine the cruciate ligaments if doubt exists on the sagittal plane. The coronal plane also is used to inspect the cartilage. It has not been shown to be a useful plane for the menisci. It is rare to see a meniscus tear on the coronal plane that is not seen on the sagittal images. We compiled the results of more than 200 consecutive knees in which we repeated our meniscussensitive sagittal sequence in the coronal plane and interpreted the coronal images separately from the sagittal images. In more than 400 menisci (two menisci/knee, >200 knees) we had only two menisci in which we saw tears that were not seen on the sagittal images. Arthroscopy was done on one meniscus, and no tear was found. We believe that a meniscus-sensitive sequence is unnecessary in the coronal plane. The coronal plane should have some sort of T2W image. If fast spin echo sequences are employed, fat suppression is recommended. It can be difficult to differentiate fat from fluid on high field strength magnets with fast spin echo. It is important to determine if fluid lies between the medial meniscus and the medial collateral ligament (MCL) to diagnose a meniscocapsular separation. A small fat pad often separates these structures and can be mistaken for fluid unless fat suppression is used. For many years, the coronal plane images were solely T1W. It took us years to realize that little, if any, information was gained using this sequence, but gradually we all moved to coronal T2W images. Only in hindsight do we see how foolish we were not to question why we were using T1W images in the coronal plane when we never saw any abnormalities. Most of us used T1W images in the coronal plane because everyone else did. (Talk about the emperor’s new clothes!) The axial plane also should be imaged with some sort of T2 sequence. As in the coronal plane, nothing is gained using a T1W image, and much can be overlooked. This is the best plane to examine the patellar cartilage. The trochlear cartilage also is well seen on this sequence. Medial patellar plicae are best seen in this plane. A second (or third) look at the cruciate ligaments can be made on the axial images, and, similarly, the collateral ligaments can be reinspected. A knee protocol that works well consists of three planes of FSE-T2W images with fat suppression and a sagittal sequence that is conventional proton density with fat suppression. That’s right, fat suppression on all four sequences, leaving us open to missing the dreaded lipoma of the knee. In 3 years of monitoring our accuracy using our MRI interpretations against the arthroscopy reports, we are satisfied that this is a solid imaging protocol that allows us a high accuracy for menisci, cruciate ligaments, collateral ligaments, and cartilage.

Figure 15-1
Meniscus tear not seen with fast spin echo sequence. A , Sagittal conventional spin echo–proton density (TR/TE 2000/20) image with fat suppression shows an oblique tear of the posterior horn of the medial meniscus ( arrow ). B , Sagittal fast spin echo–proton density (TR/TE 3000/16; ETL 4) image with fat suppression prospectively was called normal .

Figure 15-2
Use of fat suppression for the meniscus. A , Sagittal conventional spin echo–T1W image of the lateral meniscus without fat suppression shows most of the signal emanating from the marrow in the femur and tibia. B , The same sequence with fat suppression shows the meniscus to better advantage because of the suppression of signal from the marrow.
- •
Contrast: There is no place for gadolinium in routine imaging of the knee. MR arthrography has been advocated as useful in the postoperative knee to help differentiate between a repaired meniscus and a torn meniscus, but we have little experience with this.
Normal and Abnormal
MENISCI
Normal
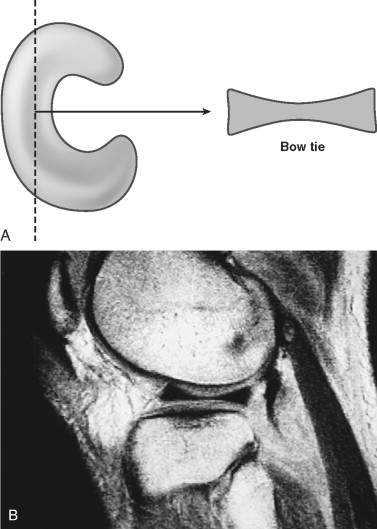
The menisci in the knee are C-shaped, fibrocartilaginous structures that are thick peripherally and thin centrally. A sagittal slice through the body segment should show the meniscus as an elongated rectangle or a bow tie, depending on how peripheral the sagittal slice is ( Fig. 15-3 ). The medial and the lateral menisci should have two contiguous images of the body of the meniscus if 4- or 5-mm-thick slices are obtained. Three or four sagittal images should be seen through the anterior and posterior horns of the menisci ( Fig. 15-4 ), with the posterior horn of the medial meniscus usually larger than the anterior horn. The anterior and posterior horns of the lateral meniscus are equal in size. The posterior horn of either meniscus should never be smaller than the anterior horn if it is normal.

The normal meniscus is devoid of signal on all imaging sequences, with the exception of children and young adults, who typically have some intermediate to high signal in the posterior horns near the meniscal attachment to the capsule. This signal represents normal vascularity and should not be misinterpreted as meniscus degeneration. The vascularity of the meniscus is greatest near the periphery and is almost nonexistent near the free edge. Peripheral tears can be repaired, whereas more central tears cannot.
Abnormal
Several grading schemes for abnormal meniscus signal have been developed. They are not generally in widespread use because the only abnormal signal that has any real significance is that which disrupts the articular surface of a meniscus, representing a tear. Any signal that does not disrupt an articular surface, with one exception, which is covered in detail subsequently, is intrasubstance or myxoid degeneration ( Fig. 15-5 ). Presumably, myxoid degeneration is a result of aging or wear and tear, but its cause is unknown. It is not a source of symptoms, does not always lead to meniscus tears, and is not treated clinically or surgically. Why mention it? If myxoid degeneration is prominent, it can be mentioned so that anyone else looking at the study would know we saw it, but judged the signal not to be a tear, rather than thinking it was simply overlooked. Also, if it is especially prominent, there is a possibility that it might represent a meniscal cyst. Meniscal cysts are discussed in more detail later.

Tears
If high signal clearly disrupts an articular surface of the meniscus, it is an easy call: it is a torn meniscus. If high signal comes close to the articular surface, but does not quite reach the articular surface, it is an easy call: it is not a tear, it is intrasubstance degeneration. It is not always that clear-cut. In many cases, it is too close to call. In these situations, do the same thing radiologists do all the time—hedge. We are not being facetious. If you tell your orthopedic surgeons that when you call a tear or when you call no tear they can count on a correct diagnosis in more than 90% of the cases, they will find MRI examinations and your readings to be very helpful. You will be able to give a definitive diagnosis in about 90% of cases. You should explain that about 10% of the time you will be unable to discern definitely if the meniscus is torn or not. In those cases, the clinical examination is paramount. If the patient gets better with conservative care, it was probably not a torn meniscus. If the patient does not improve, the surgeon may decide to perform an arthroscopic procedure, in which case you would have told the surgeon where to look for a possible meniscus tear. It seems that 10% is the hedge rate for the menisci.
It has been shown that sensitivity for meniscal tears decreases considerably if there is an associated ACL tear. There are several reasons for this. First, the meniscal tears that seem to occur when the ACL is torn are located in two places: the posterior horn of the lateral meniscus and in the periphery of the menisci (medial and lateral menisci). These are not the usual locations for meniscus tears and consequently often are overlooked. Also, several pitfalls occur in the posterior horn of the lateral meniscus that can be confused with meniscal tears, all of which are mentioned later in this chapter. Suffice it to say that when the ACL is torn, a close inspection should be done for a peripheral tear or for a tear in the posterior horn of the lateral meniscus.
Oblique or Horizontal Tears.
There are many types of meniscal tears ( Box 15-1 ). The most common is an oblique or horizontal tear (these are synonymous terms; some surgeons prefer one term over the other, and others use them interchangeably) that affects the undersurface of the posterior horn of the medial meniscus ( Fig. 15-6 ). These commonly are degenerative in nature, rather than as a result of trauma.
- •
Oblique or horizontal
- •
Vertical
- •
Flap
- •
Bucket handle
- •
- •
Peripheral
- •
Medially flipped flap tear
- •
Radial (parrot beak tear)
- •
Meniscocapsular separation

Bucket-Handle Tears.
Vertical longitudinal tears ( Fig. 15-7 ) make up the common bucket-handle tear that occurs in about 10% of meniscal tears. The normal meniscus has a body width of about 9 mm, which is seen on two consecutive sagittal images as a single slab of meniscal tissue that has a shape similar to a bow tie. When the inner edge of the meniscus displaces, a bucket-handle tear is easily diagnosed by noting only one instead of the normal two body segments present on the outermost sagittal images through the meniscus ( Fig. 15-8 ). This is called the absent bow tie sign because the body segments normally have a bow tie appearance on the sagittal images. A displaced meniscal fragment should always be found, most often in the intercondylar notch ( Fig. 15-9 ). A careful search for a fragment should be made when only one body segment is seen on the sagittal images. The displaced meniscal fragment can lie in front of the posterior cruciate ligament (PCL), which is called a double PCL sign ( Fig. 15-10 ). The displaced fragment also may flip over the anterior horn of the affected meniscus, which is called an anterior flipped meniscus sign ( Fig. 15-11 ). In any case, the absent bow tie sign is a very sensitive sign for a bucket-handle tear.





Although our original publication on the absent bow tie sign had a 97% sensitivity, a subsequent publication of ours showed a sensitivity of around 90%. Another publication looked at all the MRI signs for a bucket-handle tear and reported only a 71% sensitivity for the absent bow tie sign. Nevertheless, it was the most reliable sign for detecting bucket-handle tears. Also, in the prospective reading of their 74 cases of bucket-handle tears, the investigators had only a 46% sensitivity (using the absent bow tie sign increased their sensitivity from 46% to 71%). We now rely on the absent bow tie sign only if we can identify the displaced meniscal fragment.
Radial or Free Edge Tears.
The absent bow tie sign also is positive in free edge tears (also called radial tears or parrot beak tears ). Free edge tears are common and are an unusual source of symptoms, unless they are large. The absent bow tie sign is useful in recognizing these tears. They are easily differentiated from bucket-handle tears because the second body segment, or bow tie, has only a small gap, rather than the large gap seen in bucket-handle tears ( Fig. 15-12 ), and no displaced fragment is present. An investigation of about 200 knees that underwent arthroscopy by a single surgeon showed a 15% incidence of radial tears. In that report we described three basic appearances of radial tears: (1) ghost, (2) cleft, and (3) truncated triangle. A ghost meniscus is seen when a radial tear has completely traversed the meniscus ( Fig. 15-13 ). The MRI slice is parallel to the tear, and partial volume averaging of the adjacent meniscal tissue creates an intermediate or gray signal. This is a severe type of meniscal tear and results in profound loss of the “hoop-stress” or springlike resistance of the meniscus. The meniscus usually extrudes off of the tibia ( Fig. 15-14 ), and osteoarthritis ensues because of the lack of cushioning or protective effect of the meniscus with axial loading.



A cleft is the most reliable sign for a radial tear and is seen when the MRI slice is perpendicular to the tear (see Fig. 15-12 ). When the MRI slice is parallel to the same tear with a cleft, it results in a truncated triangle ( Fig. 15-15 ). A radial tear usually, but not always, will have two of the signs, depending on the orientation of the tear to the imaging plane. At surgery, the free edge of a meniscus with a radial tear is treated with débridement and smoothing.

Medial Flipped Meniscus.
A meniscus tear that can be seen with MRI but can be overlooked at arthroscopy is a flap tear of the medial meniscus with the flap of meniscus flipped into the medial gutter underneath the meniscus. It can be missed at surgery if the surgeon fails to probe the medial gutter and deliver the flipped fragment. These are common tears and should be considered when the body segments look thinner than normal or have a piece of meniscus missing from the undersurface ( Fig. 15-16 ). The medial flipped fragment can be seen on the coronal images lying just below and medial to the medial meniscus.

Description of Meniscal Tears.
When a meniscal tear is identified and characterized as to which type (see Box 15-1 ), additional descriptors should include location (anterior horn, posterior horn, body); extent of the tear (which meniscal surface and length); and associated findings such as meniscal cyst, discoid meniscus, or displaced fragments or flaps.
Cysts
Meniscal cysts occasionally are seen that involve a meniscus without the meniscus having a tear that extends to the articular surface. With weight bearing, the fluid in the cyst can be expressed into the adjacent soft tissues, where it is called a parameniscal cyst ( Fig. 15-17 ). It is important to advise the surgeon of the presence of such a cyst because without a meniscal tear the cyst can be missed at arthroscopy. Also, many surgeons decompress a meniscal cyst that does not have a meniscal tear by an extra-articular approach, rather than via arthroscopy. Most meniscal cysts do not exhibit marked high signal with T2W images, but the parameniscal component usually is very high in signal. When the cyst is confined to the meniscus, the signal resembles intrasubstance degeneration, only it is much more pronounced ( Fig. 15-18 ). If a mass effect makes the meniscus appear swollen, it is an easy diagnosis; otherwise, it is a difficult call.


These cases are handled by suggesting a meniscal cyst versus severe intrasubstance degeneration—at least the surgeon is aware of the possibility of a meniscal cyst. A meniscal cyst often is noticed first by seeing on the most medial or lateral sagittal images through the body of the meniscus that the normal bow tie appearance has a horizontal stripe, which represents the collapsed meniscal cyst ( Fig. 15-19 ). This often is called a horizontal cleavage tear , but that term is inappropriate because a true meniscal tear is not always present.

Discoid Meniscus
If more than two body segments are present on the sagittal images, a discoid meniscus should be considered ( Fig. 15-20 ). A discoid meniscus is most likely a congenital (although some insist it is acquired) malformation of the meniscus in which the meniscus, in the most extreme form, is disk-shaped rather than C-shaped. Most discoid menisci are not completely disk-shaped, but have a wider than normal body of the meniscus. The lateral meniscus is most commonly affected, with an incidence reported of around 3%, whereas the medial meniscus is uncommonly affected. Often a discoid meniscus is enlarged and affects the anterior or posterior horns of the meniscus asymmetrically. In such a case, the anterior or posterior horn is much larger than its counterpart. Although often encountered incidentally, discoid menisci are more prone to undergo cystic degeneration with subsequent tears than a normal meniscus. Even without cystic changes or a tear, a discoid meniscus can cause symptoms and require surgery.

A discoid meniscus that can cause symptoms without being torn is a Wrisberg variant of a discoid lateral meniscus. This is a discoid meniscus that lacks attachments to the capsule via the normal struts or fascicles and lacks attachment to the tibia via the coronary or meniscotibial ligaments at the posterior horn of the meniscus ( Fig. 15-21 ). This allows the posterior horn to sublux or fold into the joint with knee flexion, akin to a rug sliding or folding up on a slippery floor if it is not attached. In a Wrisberg variant of a discoid lateral meniscus, the only attachment to the posterior horn is the Wrisberg ligament—hence the name. It is important to inspect every discoid lateral meniscus closely for the normal struts or fascicles that surround the popliteus tendon and attach the meniscus to the capsule. If recognized, the surgeon can reattach the meniscus to the capsule and the tibia, rather than performing a meniscectomy. These are typically seen in children, and a meniscectomy at an early age leads to advanced osteoarthritis.

It is extremely valuable to recognize the normal bow tie appearance of the body segments in the medial and the lateral menisci as seen on sagittal images on every examination. Many of the aforementioned abnormalities can be recognized easily by noting the absence of the normal two body segments. These include the bucket-handle tear, radial tear, medially flipped flap tear, and meniscal cyst ( Box 15-2 ). A discoid meniscus exhibits more than two body segments. Our routine search pattern on sagittal images includes a close inspection of the body segments to be certain there are two, and only two, bow ties that are not deformed in any way. Exceptions to this expectation would include a large patient (Shaquille O’Neal would undoubtedly have three or four bow ties), or very thin slices (the two bow tie rule applies only to slice thicknesses of 4 or 5 mm), and, as mentioned previously, a discoid meniscus.
- •
Bucket-handle tear
- •
Radial tear
- •
Medially flipped flap tear
- •
Meniscal cyst
Exceptions to the two bow tie rule that can mimic a bucket-handle tear ( Box 15-3 ) can be seen in children or small adults in whom the menisci are small—only one bow tie is seen, but this is followed by only two or three images showing the anterior and posterior horns, rather than the usual three or four images; also, it occurs in both menisci. Simultaneous medial and lateral bucket-handle tears are rare. Another exception is in the postoperative knee where the free edge of the meniscus has been débrided. To recognize this situation, we have every patient fill out a form before the MRI examination that asks about prior surgery. The two bow tie rule can be broken if severe osteoarthritis is present or in older patients (>65 years old). These patients can wear down the free edge of the meniscus, leaving a very thin body segment that can be confused with a bucket-handle tear. None of these exceptions to the two bow tie rule would have a displaced meniscus as would a bucket-handle tear.
- •
Children or small adults
- •
Postoperative
- •
Severe osteoarthritis
- •
Older patients (>65 years old)
Pitfalls
A few pitfalls involving the menisci warrant mention.
Transverse Ligament.
An easy pitfall to recognize is the insertion of the transverse ligament on the anterior horns of the menisci. The transverse ligament runs across the anterior aspect of the knee in Hoffa’s fat pad from the anterior horn of the medial meniscus to the anterior horn of the lateral meniscus. Its function is unknown, and it is not present in every knee. At its insertion on the anterior horn of the lateral meniscus, it often has the appearance of a meniscus tear ( Fig. 15-22 ). It can reliably be differentiated from a tear by following it across the knee in Hoffa’s fat pad on sequential sagittal images. It uncommonly causes a similar pseudotear appearance on the medial meniscus.

Speckled Anterior Horn Lateral Meniscus.
The anterior horn of the lateral meniscus occasionally has a speckled appearance, which can resemble a macerated or torn anterior horn ( Fig. 15-23 ). This appearance is caused by fibers of the ACL inserting into the meniscus. It is reported to be seen in 60% of normal patients.

Meniscofemoral Ligament Insertion.
The posterior horn of the lateral meniscus has several pitfalls that mimic tears. Insertion of the meniscofemoral ligament of Humphry or Wrisberg can give the appearance of a meniscal tear ( Fig. 15-24 ). A meniscofemoral ligament is present in about 75% of knees. It originates on the medial femoral condyle and runs obliquely across the knee in the intercondylar notch ( Fig. 15-25 ), anterior (ligament of Humphry) or posterior (ligament of Wrisberg) to the PCL ( Fig. 15-26 ), and inserts into the posterior horn of the lateral meniscus. When considering a pseudotear from the insertion of one of the meniscofemoral ligaments, one needs to follow the ligament through the intercondylar notch to the PCL on sequential sagittal images. In 2% to 3% of knees, both ligaments (Humphry and Wrisberg) are present. The function of the meniscofemoral ligament has not been clearly established, and no injury to it has been described.