This section covers more than 300 laboratory tests. Each test is approached with the following format:
- •
Laboratory test
- •
Normal range in adult patients
- •
Common abnormalities (e.g., positive test, increased or decreased value)
- •
Causes of abnormal result
The normal ranges may differ slightly, depending on the laboratory. The reader should be aware of the “normal range” of the particular laboratory performing the test. Every attempt has been made to present current laboratory test data with emphasis on practical considerations. It’s important to remember that laboratory tests do not make diagnoses; doctors do. As such, any laboratory results should be integrated with the complete clinical picture and radiographic studies (if needed) to make a diagnosis.
ACE Level
Acetone (Serum or Plasma)
Acetylcholine Receptor (AChR) Antibody
Acid Phosphatase (Serum)
Acid Serum Test
Activated Clotting Time (ACT)
Activated Partial Thromboplastin Time (aPTT)
Adrenocorticotropic Hormone (ACTH)
Alanine Aminopeptidase
Alanine Aminotransferase (ALT, formerly serum glutamic-pyruvic transaminase [SGPT])
Albumin (Serum)
Alcohol Dehydrogenase
Aldolase (Serum)
Aldosterone (Plasma)
Alkaline Phosphatase (Serum)
Alpha-1-Antitrypsin (Serum)
Alpha-1-Fetoprotein (Serum)
ALT
Aluminum (Serum)
AMA
Amebiasis Serologic Test
Aminolevulinic Acid (d-ALA) (24-Hour Urine Collection)
Ammonia (Serum)
Amylase (Serum)
Amylase, Urine
Amyloid A Protein (Serum)
ANA
ANCA
Androstenedione (Serum)
Angiotensin II
Angiotensin-Converting Enzyme (ACE) Level
ANH
Anion Gap
Anticardiolipin Antibody (ACA)
Anticoagulant
Antidiuretic Hormone
Anti-DNA
Anti-ds DNA
Anti-Globulin Test, Direct
Anti-Globulin Test, Indirect
Antiglomerular Basement Antibody
Anti-HCV
Antihistone
Antimitochondrial Antibody (AMA)
Antineutrophil Cytoplasmic Antibody (ANCA)
Antinuclear Antibody (ANA)
Antiphospholipid Antibody
Anti-RNP Antibody
Anti-Scl-70
Anti-Smith (Anti-Sm) Antibody
Anti-Smooth Muscle Antibody
Antistreptolysin O Titer (Streptozyme, ASLO Titer)
Antithrombin III
Apolipoprotein A-1 (Apo A-1)
Apolipoprotein B (Apo B)
Arterial Blood Gases
Arthrocentesis Fluid
ASLO Titer
Aspartate Aminotransferase (AST, Serum Glutamic Oxaloacetic Transaminase [SGOT])
Atrial Natriuretic Hormone (ANH)
Basophil Count
Bicarbonate
Bile Acid Breath Test
Bile, Urine
Bilirubin, Direct (Conjugated Bilirubin)
Bilirubin, Indirect (Unconjugated Bilirubin)
Bilirubin, Total
Bilirubin, Urine
Bladder Tumor–Associated Antigen
Bleeding Time (Modified IVY Method)
Blood Volume, Total
Bordetella pertussis Serology
BRCA-1, BRCA-2
Breath Hydrogen Test
B-Type Natriuretic Peptide (BNP)
BUN
C3
C4
CA 15-3
CA 27-29
CA 72-4
CA 125
Calcitonin (Serum)
Calcium (Serum)
Calcium, Urine
Cancer Antigen 15-3 (CA 15-3)
Cancer Antigen 27-29 (CA 27-29)
Cancer Antigen 72-4 (CA 72-4)
Cancer Antigen 125 (CA-125)
Captopril Stimulation Test
Carbamazepine (Tegretol)
Carbohydrate Antigen 19-9
Carbon Dioxide, Partial Pressure
Carbon Monoxide
Carboxyhemoglobin (COHb)
Cardiac Markers (Serum)
Cardiac Troponins
Carcinoembryonic Antigen (CEA)
Cardio-CRP
Carotene (Serum)
Catecholamines, Urine
CBC
CCK
CCK-PZ
CD4 T-Lymphocyte Count (CD4 T-Cells)
CD40 Ligand
CEA
Cerebrospinal Fluid (CSF)
Ceruloplasmin (Serum)
Chlamydia Group Antibody Serologic Test
Chlamydia Trachomatis Polymerase Chain Reaction (PCR)
Chloride (Serum)
Chloride (Sweat)
Chloride, Urine
Cholecystokinin-Pancreozymin (CCK, CCK-PZ)
Cholesterol, Low-Density Lipoprotein
Cholesterol, High-Density Lipoprotein
Cholesterol, Total
Chorionic Gonadotropin (hCG), Human (Serum)
Chymotrypsin
Circulating Anticoagulant (Antiphospholipid Antibody, Lupus Anticoagulant)
CK
Clonidine Suppression Test
Clostridium difficile Toxin Assay (Stool)
CO
Coagulation Factors
Cold Agglutinins Titer
Complement (C3, C4)
Complete Blood Cell (CBC) Count
Conjugated Bilirubin
Coombs, Direct
Coombs, Indirect (Antiglobulin, Indirect)
Copper (Serum)
Copper, Urine
Corticotropin-Releasing Hormone (CRH) Stimulation Test
Cortisol (Plasma)
C-Peptide
CPK
C-Reactive Protein (CRP)
Creatinine Clearance
Creatine Kinase (CK), Creatine Phosphokinase (CPK)
Creatine Kinase Isoenzymes
CK-MB
CK-MM
CK-BB
Creatinine (Serum)
Creatinine, Urine
Cryoglobulins (Serum)
Cryptosporidium Antigen by Enzyme Immunoassay (EIA) (Stool)
CSF
Cystatin C
Cystic Fibrosis Polymerase Chain Reaction (PCR)
Cytomegalovirus by Polymerase Chain Reaction (PCR)
DAT
d-Dimer
Dehydroepiandrosterone Sulfate
Deoxycorticosterone (11-Deoxycorticosterone, DOC), Serum
Dexamethasone Suppression Test, Overnight
Dihydrotestosterone, Serum, Urine
Direct Antiglobulin Test (DAT, Coombs Test, Direct)
Disaccharide Absorption Tests
DOC
Donath-Landsteiner (D-L) Test For Paroxysmal Cold Hemoglobinuria
Digoxin (Lanoxin)
Dilantin
Dopamine
d-Xylose Absorption Test
Electrolytes, Urine
Electrophoresis, Hemoglobin
Electrophoresis, Protein
ENA Complex
Endomysial Antibodies
Eosinophil Count
Epinephrine, Plasma
Epstein-Barr Virus (EBV) Serology
Erythrocyte Sedimentation Rate (ESR) (Westergren)
Erythropoietin (EP)
Estradiol (Serum)
Estrogens, Total
Ethanol (Blood)
Extracf Nuclear Antigen (ENA Complex, Anti-RNP Antibody, Anti-SM, Anti-Smith)
Factor V Leiden
FDP
FENA
Fecal FAT, Qualitative
Fecal FAT, Quantitative (72-Hour Collection)
Fecal Globin Immunochemical Test
Ferritin (Serum)
Fibrin Degradation Product (FDP)
Fibrinogen
5-Hydroxyindole-Acetic Acid, Urine
5′ Nucleotidase
Fluorescent Treponemal Antibody
Folate (Folic Acid)
Follicle-Stimulating Hormone (FSH)
Fractional Excretion of Sodium (FENA)
Free T4
Free Thyroxine Index
FSH
FTA-ABS (Serum)
Furosemide Stimulation Test
Gamma-Glutamyl Transferase (GGT)
Gastrin (Serum)
Gastrin Stimulation Test
Gliadin Antibodies, Immunoglobulin (Ig) A and IgG
Glomerular Basement Membrane Antibody
Glomerular Filtration Rate (GFR)
Glucagon
Glucose, Fasting
Glucose, Postprandial
Glucose Tolerance Test
Glucose-6-Phosphate Dehydrogenase (G6PD) Screen (Blood)
γ-Glutamyl Transferase (GGT)
Glycated (Glycosylated) Hemoglobin (HbA1c)
Glycohemoglobin
Growth Hormone
Growth Hormone–Releasing Hormone (GHRH)
Growth Hormone Suppression Test (After Glucose)
HAM Test (Acid Serum Test)
Haptoglobin (Serum)
HbA1c
HDL
Helicobacter pylori (Serology, Stool Antigen)
Hematocrit
Hemoglobin
Hemoglobin (Hb) Electrophoresis
Hemoglobin, Glycated
Hemoglobin, Glycosylated
Hemoglobin H
Hemoglobin, Urine
Hemosiderin, Urine
Heparin-Induced Thrombocytopenia Antibodies
Hepatitis A Antibody
Hepatitis B Core Antibody
Hepatitis B DNA
Hepatitis Be Antigen (HBeAg) and Antibody
Hepatitis B Surface Antibody
Hepatitis B Surface Antigen (HBsAg)
Hepatitis C Antibody (Anti-HCV)
Hepatitis C RNA
Hepatitis D Antigen and Antibody
Her-2/nue
Herpes Simplex Virus (HSV)
Heterophil Antibody
HFE Screen For Hereditary Hemochromatosis
High-Density Lipoprotein (HDL) Cholesterol
Homocysteine, Plasma
Hs-CRP
HSV
Human Herpes Virus 8 (HHV8)
Human Immunodeficiency Virus Antibody, Type 1 (HIV-1)
Human Papilloma Virus (HPV)
Huntington’s Disease Polymerase Chain Reaction (PCR)
Immune Complex Assay
Immunoglobulin (Ig)
Influenza A and B Tests
INR
Insulin Autoantibodies
Insulin, Free
Insulin-Like Growth Factor I (IGF-1), Serum
Insulin-Like Growth Factor II
International Normalized Ratio (INR)
Intrinsic Factor Antibodies
Iron-Binding Capacity (Total Iron-Binding Capacity [TIBC])
Iron Saturation (% Transferrin Saturation)
Iron, Serum
Lactate (Blood)
Lactate Dehydrogenase (LDH)
Lactate Dehydrogenase (LDH) Isoenzymes
Lactose Tolerance Test (Serum)
Lanoxin
Lap Score
Lead
LDH
LDL
Legionella pneumophila Polymerase Chain Reaction (PCR)
Legionella Titer
Leukocyte Alkaline Phosphatase (LAP)
LH
Lipase
Lipoprotein (A)
Lipoprotein Cholesterol, Low Density
Lipoprotein Cholesterol, High Density
Liver Kidney Microsome Type 1 (LKM1) Antibodies
Low-Density Lipoprotein (LDL) Cholesterol
Lupus Anticoagulant (LA) Test
Luteinizing Hormone (LH), Blood
Lymphocytes
Magnesium (Serum)
Mean Corpuscular Volume (MCV)
Metanephrines, Urine
Methylmalonic Acid, Serum
Mitochondrial Antibody (Antimitochondrial antibody [AMA])
Monocyte Count
Mycoplasma pneumoniae Polymerase Chain Reaction (PCR)
Myelin Basic Protein, Cerebrospinal Fluid
Myoglobin, Urine
Natriuretic Peptide
Neisseria gonorrhoeae Polymerase Chain Reaction (PCR)
Neutrophil Count
Norepinephrine
Osmolality, Serum
Osmolality, Urine
Osmotic Fragility Test
Paracentesis Fluid
Parathyroid Hormone
Parietal Cell Antibodies
Partial Thromboplastin Time (PTT), Activated Partial Thromboplastin Time (aPTT)
Pepsinogen I
PFA
pH, Blood
Phenobarbital
Phenytoin (Dilantin)
Phosphatase, Acid
Phosphatase, Alkaline
Phosphate (Serum)
pH, Urine
Plasminogen
Platelet Aggregation
Platelet Antibodies
Platelet Count
Platelet Function Analysis (PFA) 100 Assay
Potassium (Serum)
Potassium, Urine
Procainamide
Progesterone, Serum
Prolactin
Prostate-Specific Antigen (PSA)
Prostatic Acid Phosphatase
Protein (Serum)
Protein C Assay
Protein Electrophoresis (Serum)
Protein S Assay
Prothrombin Time (PT)
Protoporphyrin (Free Erythrocyte)
PSA
PT
PTT
Rapid Plasma Reagin
RDW
Red Blood Cell Count
Red Blood Cell Distribution Width (RDW)
Red Blood Cell Folate
Red Blood Cell Mass (Volume)
Renin (Serum)
Respiratory Syncytial Virus (RSV) Screen
Reticulocyte Count
Rheumatoid Factor
RNP
RPR
Rotavirus Serology
Schilling Test
Sedimentation Rate
Semen Analysis
SGOT
SGPT
Sickle Cell Test
Smooth Muscle Antibody
Sodium (Serum)
Streptozyme
Sucrose Hemolysis Test (Sugar Water Test)
Sudan III Stain (Qualitative Screening for Fecal Fat)
T3 (Triiodothyronine)
T3 Resin Uptake (T3RU)
T4, Serum T4, and Free (Free Thyroxine)
Serum Free T4
Tegretol
Testosterone
Theophylline
Thiamine
Thoracentesis Fluid
Thrombin Time (TT)
Thyroglobulin
Thyroid Binding Globulin (TBG)
Thyroid Microsomal Antibodies
Thyroid-Stimulating Hormone (TSH)
Thyrotropin (Thyroid-Stimulating Hormone [TSH]) Receptor Antibodies
Thyrotropin-Releasing Hormone (TRH) Stimulation Test
TIBC
Tissue Transglutaminase Antibody
Transferrin
Triglycerides
Triiodothyronine
Troponins, Serum
TSH
TT
Unconjugated Bilirubin
Urea Nitrogen
Uric Acid (Serum)
Urinalysis
Urine Amylase
Urine Bile
Urine Calcium
Urine cAMP
Urine Catecholamines
Urine Chloride
Urine Copper
Urine Cortisol, Free
Urine Creatinine (24-Hour)
Urine Crystals
Urine Eosinophils
Urine 5-Hydroxyindole-Acetic Acid (Urine 5-HIAA)
Urine Glucose (Qualitative)
Urine Hemoglobin, Free
Urine Hemosiderin
Urine Indican
Urine Ketones (Semiquantitative)
Urine Metanephrines
Urine Myoglobin
Urine Nitrite
Urine Occult Blood
Urine Osmolality
Urine pH
Urine Phosphate
Urine Potassium
Urine Protein (Quantitative)
Urine Sodium (Quantitative)
Urine Specific Gravity
Urine Vanillylmandelic Acid (VMA)
Varicella Zoster Virus (VZV) Serologic Testing
Vasoactive Intestinal Peptide (VIP)
Venereal Disease Research Laboratories (VDRL)
VIP
Viscosity (Serum)
Vitamin B 12
Vitamin D, 1,25 Dihydroxy Calciferol, Vitamin D 25(OH)D (25- Hydroxyvitamin D)
Vitamin K
Von Willebrand’s Factor
WBCs
Westergren
White Blood Cell Count
ACE Level
Acetylcholine Receptor (AChR) Antibody
Normal: <0.03 nmol/L
Elevated in: myasthenia gravis. Changes in AChR concentration correlate with the clinical severity of myasthenia gravis after therapy and during therapy with prednisone and immunosuppressants. False-positive AChR antibody results may be found in patients with Eaton-Lambert syndrome.
Acid Phosphatase (Serum)
Normal range: enzymatic, prostatic 0 to 5.5 U/L; enzymatic, total 2 to 12 U/L
Elevated in: carcinoma of prostate, other neoplasms (breast, bone), Paget’s disease of bone, hemolysis, multiple myeloma, osteogenesis imperfecta, malignant invasion of bone, Gaucher’s disease, myeloproliferative disorders, prostatic palpation or surgery, hyperparathyroidism, liver disease, chronic renal failure, idiopathic thrombocytopenic purpura (ITP)
Acid Serum Test
See Ham Test
Activated Partial Thromboplastin Time (aPTT)
See Partial Thromboplastin Time (PTT), Activated Partial Thromboplastin Time (aPTT)
Adrenocorticotropic Hormone (ACTH)
Normal range: 9 to 52 pg/mL
Elevated in: Addison’s disease, ectopic ACTH-producing tumors, congenital adrenal hyperplasia, Nelson’s syndrome, pituitary-dependent Cushing’s disease
Decreased in: secondary adrenocortical insufficiency, hypopituitarism, adrenal adenoma or adrenal carcinoma
Alanine Aminotransferase (ALT, formerly serum glutamic-pyruvic transaminase [SGPT])
Normal range:
Male: 10 to 40 U/L
Female: 8 to 35 U/L
Elevated in: liver disease (e.g., hepatitis, cirrhosis, Reye’s syndrome), alcohol abuse, drug use (e.g., acetaminophen, statins, nonsteroidal antiinflammatory drugs [NSAIDs], antibiotics, anabolic steroids, narcotics, heparin, labetalol, amiodarone, chlorpromazine, phenytoin), hepatic congestion, infectious mononucleosis, liver metastases, myocardial infarction [MI], myocarditis, severe muscle trauma, dermatomyositis or polymyositis, muscular dystrophy, malignancy, renal and pulmonary infarction, convulsions, eclampsia, dehydration (relative increase), ingestion of Chinese herbs
Decreased in: azotemia, advanced malnutrition, chronic renal dialysis, chronic alcoholic liver disease, metronidazole use
Albumin (Serum)
Normal range: 4 to 6 g/dL
Elevated in: dehydration (relative increase), intravenous albumin infusion
Decreased in: liver disease, nephrotic syndrome, poor nutritional status, rapid intravenous hydration, protein-losing enteropathies (inflammatory bowel disease), severe burns, neoplasia, chronic inflammatory diseases, pregnancy, prolonged immobilization, lymphomas, hypervitaminosis A, chronic glomerulonephritis
Aldolase (Serum)
Normal range: 0 to 6 U/L
Elevated in: rhabdomyolysis, dermatomyositis or polymyositis, trichinosis, acute hepatitis and other liver diseases, muscular dystrophy, myocardial infarction, prostatic carcinoma, hemorrhagic pancreatitis, gangrene, delirium tremens, burns
Decreased in: loss of muscle mass, late stages of muscular dystrophy
Aldosterone (Plasma)
Normal range:
Adult supine: 3 to 16 ng/dL
Adult upright: 7 to 30 ng/dL
Adrenal vein: 200 to 800 ng/dL
Elevated in: aldosterone-secreting adenoma, bilateral adrenal hyperplasia, secondary aldosteronism (diuretics, congestive heart failure, laxatives, nephritic syndrome, cirrhosis with ascites, Bartter’s syndrome, pregnancy, starvation). Table 2.1 summarizes use of plasma renin and plasma aldosterone values in the evaluation of hypokalemia or hyperkalemia.
TABLE 2.1
Use of Plasma Renin and Plasma Aldosterone Values to Assess the Basis of Hypokalemia or Hyperkalemia
From Skorecki K, Chertow GM, Marsden PA, et al: Brenner and Rector’s the kidney, ed 10, Philadelphia, Elsevier, 2016.
Renin
Aldosterone
Lesions That Cause Hypokalemia
Adrenal gland:
Primary hyperaldosteronism
Low
High
Glucocorticoid-remediable hyperaldosteronism
Low
High
Kidney:
Renal artery stenosis
High
High
Malignant hypertension
High
High
Renin-secreting tumor
High
High
Liddle’s syndrome
Low
Low
Disorders involving 11β-hydroxysteroid dehydrogenase (HSDH)
Low
Low
Lesions That Cause Hyperkalemia
Adrenal gland:
Addison’s disease
High
Low
Kidney:
Pseudohypoaldosteronism type 1
High
High
Hyporeninemic hypoaldosteronism
Low
Low
Decreased in: Addison’s disease, renin deficiency, Turner’s syndrome, diabetes mellitus, isolated aldosterone deficiency, postacute alcohol intoxication (hangover phase)
Alkaline Phosphatase (Serum)
Normal range: 30 to 120 U/L
Elevated in: biliary obstruction, cirrhosis (particularly primary biliary cirrhosis), liver disease (hepatitis, infiltrative liver diseases, fatty metamorphosis), Paget’s disease of bone, osteitis deformans, rickets, osteomalacia, hypervitaminosis D, hyperparathyroidism, hyperthyroidism, ulcerative colitis, bowel perforation, bone metastases, healing fractures, bone neoplasms, acromegaly, infectious mononucleosis, cytomegalovirus infections, sepsis, pulmonary infarction, hypernephroma, leukemia, myelofibrosis, multiple myeloma, drug therapy (estrogens, albumin, erythromycin and other antibiotics, cholestasis-producing drugs [phenothiazines]), pregnancy, puberty, postmenopausal females. Fig. 2.1 illustrates evaluation of isolated elevation of serum alkaline phosphatase.

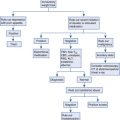
FIG. 2.1
Evaluation of an isolated elevation of the serum alkaline phosphatase level. ACE, angiotensin-converting enzyme; ALP, alkaline phosphatase; AMA, antimitochondrial antibodies; 5 ′ NT , 5′ nucleotidase; ERCP, endoscopic retrograde cholangiopancreatography; MRCP, magnetic resonance cholangiopancreatography; RUQ, right upper quadrant.
From Feldman M, Friedman LS, Brandt LJ: Sleisenger and Fordtran’s gastrointestinal and liver disease , ed 10, Philadelphia, Elsevier, 2016.
Decreased in: hypothyroidism, pernicious anemia, hypophosphatemia, hypervitaminosis D, malnutrition
Alpha-1-Fetoprotein (Serum)
Normal range: 0 to 20 ng/mL
Elevated in: hepatocellular carcinoma (usual values >1000 ng/mL), germinal neoplasms (testis, ovary, mediastinum, retroperitoneum), liver disease (alcoholic cirrhosis, acute hepatitis, chronic active hepatitis), fetal anencephaly, spina bifida, basal cell carcinoma, breast carcinoma, pancreatic carcinoma, gastric carcinoma, retinoblastoma, esophageal atresia
Amylase (Serum)
Normal range: 0 to 130 U/L
Elevated in: acute pancreatitis, macroamylasemia, salivary gland inflammation, mumps, pancreatic neoplasm, abscess, pseudocyst, ascites, perforated peptic ulcer, intestinal obstruction, intestinal infarction, acute cholecystitis, appendicitis, ruptured ectopic pregnancy, peritonitis, burns, diabetic ketoacidosis, renal insufficiency, drug use (morphine), carcinomatosis of lung, esophagus, ovary, acute ethanol ingestion, prostate tumors, post–endoscopic retrograde cholangiopancreatography, bulimia, anorexia nervosa
Decreased in: advanced chronic pancreatitis, hepatic necrosis, cystic fibrosis
Amylase, Urine
See Urine Amylase
Androstenedione (Serum)
Normal range:
Male: 75 to 205 ng/dL
Female: 85 to 275 ng/dL
Elevated in: congenital adrenal hyperplasia, polycystic ovary syndrome, ectopic adrenocorticotropic hormone–producing tumor, Cushing’s syndrome, hirsutism, hyperplasia of ovarian stroma, ovarian neoplasm
Decreased in: ovarian failure, adrenal failure, sickle cell anemia
Angiotensin-Converting Enzyme (ACE) Level
Normal: <40 nmol/mL/min
Elevated in: sarcoidosis, primary biliary cirrhosis, alcoholic liver disease, hyperthyroidism, hyperparathyroidism, diabetes mellitus, amyloidosis, multiple myeloma, lung disease (asbestosis, silicosis, berylliosis, allergic alveolitis, coccidioidomycosis), Gaucher’s disease, leprosy
Decreased in: ACE inhibitor therapy
Anion Gap
Normal range: 9 to 14 mEq/L. The calculation of anion gap is described in Table 2.2 .
TABLE 2.2
The Anion Gap
From Skorecki K, Chertow GM, Marsden PA, et al: Brenner and Rector’s the kidney , ed 10, Philadelphia, Elsevier, 2016.
Anion Gap = Na + − (Cl − + HCO 3 − ) = 9 ± 3 mEq/L (Assumes Normal [Albumin]) ∗
Decreased Anion Gap
Increased Anion Gap
Increased Cations (Not Na + )
Increased Anions (Not Cl − or HCO 3 − )
↑ Ca 2+ , Mg 2+
↑ Albumin
↑ Li +
Alkalosis
↑ Immunoglobulin G
↑ Inorganic anions
Phosphate
Sulfate
Decreased Anions (Not Cl − or HCO 3 − )
Hypoalbuminemia ∗
Acidosis
Laboratory Error
Hyperviscosity
Bromism
↑ Organic anions
l -Lactate
d -Lactate
Ketones
Uremic
↑ Exogenously supplied anions
Toxins
Salicylate
Paraldehyde
Ethylene glycol
Propylene glycol
Methanol
Toluene
Pyroglutamic acid (5-oxoprolene)
↑ Unidentified anions
Other toxins
Uremic
Hyperosmolar, nonketotic states
Myoglobinuric acute kidney injury
Decreased Cations (Not Na + )
↓ Ca 2+ , Mg 2+
∗ For each decline in albumin by 1 g/dL from normal (4.5 g/dL), the anion gap decreases by 2.5 mEq/L.
Elevated in: lactic acidosis, ketoacidosis (diabetic ketoacidosis, alcoholic starvation), uremia (chronic renal failure), ingestion of toxins (paraldehyde, methanol, salicylates, ethylene glycol), hyperosmolar nonketotic coma, antibiotic therapy (carbenicillin)
Decreased in: hypoalbuminemia, severe hypermagnesemia, immunoglobulin G myeloma, lithium toxicity, laboratory error (falsely decreased sodium or overestimation of bicarbonate or chloride), hypercalcemia of parathyroid origin, antibiotic therapy (e.g., polymyxin)
Antidiuretic Hormone
Normal range: mOsm/kg 295 to 300; 4 to 12 pg/mL
Elevated in: syndrome of inappropriate antidiuretic hormone, antipsychotic medication therapy, ectopic antidiuretic hormone from systemic neoplasm, Guillain-Barré, central nervous system infections, brain tumors, nephrogenic diabetes insipidus
Decreased in: central diabetes insipidus, nephritic syndrome, psychogenic polydipsia, demeclocycline, lithium therapy, phenytoin use, alcohol use
Anti-Globulin Test, Indirect
See Coombs, Indirect
Antineutrophil Cytoplasmic Antibody (ANCA)
Positive test:
Cytoplasmic pattern (cANCA): positive in granulomatosis with polyangiitis (Wegener’s granulomatosis)
Perinuclear pattern (pANCA): positive in inflammatory bowel disease, primary biliary cirrhosis, primary sclerosing cholangitis, autoimmune chronic active hepatitis, crescentic glomerulonephritis
Antinuclear Antibody (ANA)
Normal: <1:20 titer
Positive test: systemic lupus erythematosus (more significant if titer > 1:160), drug therapy (phenytoin, ethosuximide, primidone, methyldopa, hydralazine, carbamazepine, penicillin, procainamide, chlorpromazine, griseofulvin, thiazides), chronic active hepatitis, age older than 60 years (particularly age older than 80), rheumatoid arthritis, scleroderma, mixed connective tissue disease, necrotizing vasculitis, Sjögren’s syndrome
Fig. 2.2 describes diagnostic tests and diagnoses to consider from ANA patterns.

Antistreptolysin O Titer (Streptozyme, ASLO Titer)
Normal for adults: <160 Todd units
Elevated in: streptococcal upper airway infection, acute rheumatic fever, acute glomerulonephritis, increased levels of β-lipoprotein (false-positive ASLO test)
Note: A fourfold increase in titer between acute and convalescent specimens is diagnostic of streptococcal upper airway infection regardless of the initial titer.
Antithrombin III
Normal range: 81% to 120% of normal activity; 17 to 30 mg/dL
Elevated in: warfarin drug therapy, post–myocardial infarction
Decreased in: hereditary deficiency of antithrombin III, disseminated intravascular coagulation, pulmonary embolism, cirrhosis, thrombolytic therapy, chronic liver failure, postsurgery, third trimester of pregnancy, oral contraceptive use, nephrotic syndrome, intravenous heparin therapy >3 days, sepsis, acute leukemia, carcinoma, thrombophlebitis
Apolipoprotein A-1 (Apo A-1)
Normal: recommended >120 mg/dL
Elevated in: familial hyperalphalipoproteinemia, statins, niacin, estrogens, weight loss, familial cholesteryl ester transfer protein deficiency
Decreased in: familial hypoalphalipoproteinemia, Tangier disease, diuretic use, androgens, cigarette smoking, hepatocellular disorders, chronic renal failure, nephritic syndrome, coronary heart disease, cholestasis
Apolipoprotein B (Apo B)
Normal: desirable <100 mg/dL, high risk >120 mg/dL
Elevated in: high-saturated-fat diet, high-cholesterol diet, hyper-apobetalipoproteinemia, familial combined hyperlipidemia, anabolic steroids, diuretic use, beta blocker therapy, corticosteroid use, progestin use, diabetes, hypothyroidism, chronic renal failure, liver disease, Cushing’s syndrome, coronary heart disease
Decreased in: statin therapy, niacin, low-cholesterol diet, malnutrition, abetalipoproteinemia, hypobetalipoproteinemia, hyperthyroidism
Arterial Blood Gases
Normal range:
P o 2 : 75 to 100 mm Hg
P co 2 : 35 to 45 mm Hg
<SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='HCO−3′>HCO−3HCO−3
HCO − 3
: 24 to 28 mEq/L
pH: 7.35-7.45
Abnormal values: Acid-base disturbances (see following). Table 2.3 summarizes acid-base abnormalities and appropriate compensatory responses.
TABLE 2.3
Acid-Base Abnormalities and Appropriate Compensatory Responses for Simple Disorders
Adapted from Bidani A, Tauzon DM, Heming TA: Regulation of whole body acid-base balance. In DuBose TD, Hamm LL, [eds]: Acid-base and electrolyte disorders: a companion to Brenner and Rector’s the kidney , Philadelphia, 2002, Saunders, pp. 1-2. From Skorecki K, Chertow GM, Marsden PA, et al: Brenner and Rector’s the kidney , ed 10, Philadelphia, Elsevier, 2016.
Primary Acid-Base Disorders
Primary Defect
Effect on pH
Compensatory Response
Expected Range of Compensation
Limits of Compensation
Respiratory acidosis
Alveolar hypoventilation (↑ P co 2 )
↓
↑ Renal HCO 3 − reabsorption (HCO 3 − ↑)
Acute
Δ [HCO 3 − ] = +1 mEq/L for each ↑ Δ PCO 2 of 10 mm Hg
[HCO 3 − ] = 38 mEq/L
Chronic
Δ [HCO 3 − ] = +4 mEq/L for each ↑ Δ PCO 2 of 10 mm Hg
[HCO 3 − ] = 45 mEq/L
Respiratory alkalosis
Alveolar hyperventilation (↓ P co 2 )
↑
↓ Renal HCO 3 − reabsorption (HCO 3 − ↓)
Acute
Δ [HCO 3 − ] = −2 mEq/L for
each ↓ Δ PCO 2 of 10 mm Hg
[HCO 3 − ] = 18 mEq/L
Chronic
Δ [HCO 3 − ] = −5 mEq/L for each ↓ Δ PCO 2 of 10 mm Hg
[HCO 3 − ] = 15 mEq/L
Metabolic acidosis
Loss of HCO 3 − or gain of H + (↓HCO 3 − )
↓
Alveolar hyperventilation to ↑ pulmonary CO 2 excretion (↓P co 2 )
P co 2 = 1.5[HCO 3 − ] + 8 ± 2
P co 2 = last 2 digits of pH × 100
P co 2 = 15 + [HCO 3 − ]
P co 2 = 15 mm Hg
Metabolic alkalosis
Gain of HCO 3 Δ or loss of H + (↑HCO 3 − )
↑
Alveolar hypoventilation to ↓ pulmonary CO 2 excretion (↑P co 2 )
P co 2 = +0.6 mm Hg for Δ [HCO 3 − ] of 1 mEq/L
P co 2 = 15 + [HCO 3 − ]
P co 2 = 55 mm Hg
P co 2 , carbon dioxide pressure.
- 1.
Metabolic acidosis
- a.
Metabolic acidosis with increased anion gap (AG acidosis)
- i.
Lactic acidosis
- ii.
Ketoacidosis (diabetes mellitus, alcoholic ketoacidosis)
- iii.
Uremia (chronic renal failure)
- iv.
Ingestion of toxins (paraldehyde, methanol, salicylate, ethylene glycol)
- v.
High-fat diet (mild acidosis)
- vi.
Metabolic acidosis with normal AG (hyperchloremic acidosis)
- vii.
Renal tubular acidosis (including acidosis of aldosterone deficiency)
- viii.
Intestinal loss of <SPAN role=presentation tabIndex=0 id=MathJax-Element-2-Frame class=MathJax style="POSITION: relative" data-mathml='HCO−3′>HCO−3HCO−3
HCO − 3
(diarrhea, pancreatic fistula)
- ix.
Carbonic anhydrase inhibitors (e.g., acetazolamide)
- x.
Dilutional acidosis (as a result of rapid infusion of bicarbonate-free isotonic saline)
- xi.
Ingestion of exogenous acids (ammonium chloride, methionine, cystine, calcium chloride)
- xii.
Ileostomy
- xiii.
Ureterosigmoidostomy
- xiv.
Drug therapy: amiloride, triamterene, spironolactone, beta blockers
- i.
- a.
- 2.
Respiratory acidosis
- a.
Pulmonary disease (chronic obstructive pulmonary disease, severe pneumonia, pulmonary edema, interstitial fibrosis)
- b.
Airway obstruction (foreign body, severe bronchospasm, laryngospasm)
- c.
Thoracic cage disorders (pneumothorax, flail chest, kyphoscoliosis)
- d.
Defects in muscles of respiration (myasthenia gravis, hypokalemia, muscular dystrophy)
- e.
Defects in peripheral nervous system (amyotrophic lateral sclerosis, poliomyelitis, Guillain-Barré syndrome, botulism, tetanus, organophosphate poisoning, spinal cord injury)
- f.
Depression of respiratory center (anesthesia, narcotics, sedatives, vertebral artery embolism or thrombosis, increased intracranial pressure)
- g.
Failure of mechanical ventilator
- a.
- 3.
Metabolic alkalosis. Metabolic alkalosis is divided into chloride-responsive (urinary chloride <15 mEq/L) and chloride-resistant forms (urinary chloride level >15 mEq/L).
- a.
Chloride-responsive
- i.
Vomiting
- ii.
Nasogastric suction
- iii.
Diuretics
- iv.
Posthypercapnic alkalosis
- v.
Stool losses (laxative abuse, cystic fibrosis, villous adenoma)
- vi.
Massive blood transfusion
- vii.
Exogenous alkali administration
- i.
- b.
Chloride-resistant
- i.
Hyperadrenocorticoid states (Cushing’s syndrome, primary hyperaldosteronism, secondary mineralocorticoidism [licorice ingestion, chewing tobacco use])
- ii.
Hypomagnesemia
- iii.
Hypokalemia
- iv.
Bartter’s syndrome
- i.
- a.
- 4.
Respiratory alkalosis
- a.
Hypoxemia (pneumonia, pulmonary embolism, atelectasis, high-altitude living)
- b.
Drugs (salicylates, xanthines, progesterone, epinephrine, thyroxine, nicotine)
- c.
Central nervous system disorders (tumor, cerebrovascular accident, trauma, infections)
- d.
Psychogenic hyperventilation (anxiety, hysteria)
- e.
Hepatic encephalopathy
- f.
Gram-negative sepsis
- g.
Hyponatremia
- h.
Sudden recovery from metabolic acidosis
- i.
Assisted ventilation
- a.
Arthrocentesis Fluid
Interpretation of results:
- 1.
Color: Normally it is clear or pale yellow; cloudiness indicates inflammatory process or presence of crystals, cell debris, fibrin, or triglycerides.
- 2.
Viscosity: Normally it has a high viscosity because of hyaluronate; when fluid is placed on a slide, it can be stretched to a string greater than 2 cm in length before separating (low viscosity indicates breakdown of hyaluronate [lysosomal enzymes from leukocytes] or the presence of edema fluid).
- 3.
Mucin clot: Add 1 mL of fluid to 5 mL of a 5% acetic acid solution and allow 1 minute for the clot to form; a firm clot (does not fragment on shaking) is normal and indicates the presence of large molecules of hyaluronic acid (this test is nonspecific and infrequently done).
- 4.
Glucose: Normally glucose approximately equals serum glucose level; a difference of more than 40 mg/dL is suggestive of infection.
- 5.
Protein: Total protein concentration is less than 2.5 g/dL in the normal synovial fluid; it is elevated in inflammatory and septic arthritis.
- 6.
Microscopic examination for crystals
- a.
Gout: monosodium urate crystals
- b.
Pseudogout: calcium pyrophosphate dihydrate crystals
- a.
Table 2.4 describes synovial fluid findings in common disorders.
| Normal | Osteoarthritis | Rheumatoid and Other Inflammatory Arthritis | Septic Arthritis | |
|---|---|---|---|---|
| Gross appearance | Clear | Clear | Opaque | Opaque |
| Volume (mL) | 0–1 | 0–10 | 5–50 | 5–50 |
| Viscosity | High | High | Low | Low |
| Total white cell count/mm 3 | <200 | 200–10,000 | 500–75,000 | >50,000 |
| % Polymorphonuclear cells | <25 | <50 | >50 | >75 |
Aspartate Aminotransferase (AST, Serum Glutamic Oxaloacetic Transaminase [SGOT])
Normal range: 0 to 35 U/L
Elevated in: liver disease (hepatitis, hemochromatosis, cirrhosis, Reye’s syndrome, Wilson’s disease), alcohol abuse, drug therapy (acetaminophen, statins, nonsteroidal antiinflammatory drugs, angiotensin-converting enzyme inhibitors, heparin, labetalol, phenytoin, amiodarone, chlorpromazine), hepatic congestion, infec tious mononucleosis, myocardial infarction, myocarditis, severe muscle trauma, dermatomyositis and polymyositis, muscular dystrophy, malignancy, renal and pulmonary infarction, convulsions, eclampsia
Decreased in: uremia, vitamin B 6 deficiency
Basophil Count
Normal range: 0.4% to 1% of total white blood cells; 40 to 100/mm 3
Elevated in: inflammatory processes, leukemia, polycythemia vera, Hodgkin’s lymphoma, hemolytic anemia, after splenectomy, myeloid metaplasia, myxedema
Decreased in: stress, hypersensitivity reaction, steroids, pregnancy, hyperthyroidism
Bicarbonate
Normal range:
Arterial: 21 to 28 mEq/L
Venous: 22 to 29 mEq/L
Elevated in: metabolic alkalosis, compensated respiratory acidosis, diuretics, corticosteroids, laxative abuse
Decreased in: metabolic acidosis; compensated respiratory alkalosis; acetazolamide, cyclosporine, or cholestyramine use; methanol or ethylene glycol poisoning
Bile, Urine
See Urine Bile
Bilirubin, Total
Normal range: 0 to 1 mg/dL
Elevated in: liver disease (hepatitis, cirrhosis, cholangitis, neoplasm, biliary obstruction, infectious mononucleosis), hereditary disorders (Gilbert’s disease, Dubin-Johnson syndrome), drug therapy (steroids, diphenylhydantoin, phenothiazines, penicillin, erythromycin, clindamycin, captopril, amphotericin B, sulfonamides, azathioprine, isoniazid, 5-aminosalicylic acid, allopurinol, methyldopa, indomethacin, halothane, oral contraceptives, procainamide, tolbutamide, labetalol), hemolysis, pulmonary embolism or infarct, hepatic congestion resulting from congestive heart failure Table 2.5 compares hereditary disorders of bilirubin metabolism and transport.
TABLE 2.5
Hereditary Disorders of Bilirubin Metabolism and Transport
From Feldman M, Friedman LS, Brandt LJ: Sleisenger and Fordtran’s gastrointestinal and liver disease , ed 10, Philadelphia, Elsevier, 2016.
Parameter
Gilbert’s
Type I Crigler-Najjar
Type II Crigler-Najjar
Dubin-Johnson
Rotor’s
Incidence
6%–12%
Very rare
Uncommon
Uncommon
Rare
Gene affected
UGT1A1
UGT1A1
UGT1A1
MRP2
OATP1B1 and OATP1B3
Metabolic defect
↓Bilirubin conjugation
No bilirubin conjugation
↓↓Bilirubin conjugation
Impaired canalicular export of conjugated bilirubin
Impaired canalicular export of conjugated bilirubin
Plasma bilirubin (mg/dL)
≤3 in absence of fasting or hemolysis, almost all unconjugated
Usually >20 (range, 17–50), all unconjugated
Usually <20 (range, 6–45), almost all unconjugated
Usually <7, about half conjugated
Usually <7, about half conjugated
Liver histology
Usually normal, occasional →lipofuscin
Normal
Normal
Coarse pigment in centrilobular hepatocytes
Normal
Other distinguishing features
↓Bilirubin concentration with phenobarbital
No response to phenobarbital
↓Bilirubin concentration with phenobarbital
→Bilirubin concentration with estrogens; →→urinary coproporphyrin I/III ratio
Mild →urinary coproporphyrin I/III ratio
Prognosis
Normal (theoretical risk of selected drug toxicity)
Death in infancy if untreated
Usually normal
Normal (theoretical risk of selected drug toxicity)
Normal (theoretical risk of selected drug toxicity)
Treatment
None
Phototherapy as a bridge to liver transplantation
Phenobarbital for →→bilirubin concentration
Avoid estrogens
None available
MRP2, multidrug resistance–associated protein-2 gene; OATP, organic anion transporter; UGTIA1, bilirubin uridine diphosphate-glucuronyl transferase gene.
Bilirubin, Urine
See Urine Bile
Bladder Tumor–Associated Antigen
Normal: ≤14 U/mL. The test is used to detect bladder cancer recurrence. Sensitivity is 57% to 83% and specificity 68% to 72%.
Elevated in: bladder cancer, renal stones, nephritis, urinary tract infection, hematuria, renal cancer, cystitis, recent bladder or urinary tract trauma
Bleeding Time (Modified IVY Method)
Normal range: 2 to 9.5 minutes
Elevated in: thrombocytopenia, capillary wall abnormalities, platelet abnormalities (Bernard-Soulier disease, Glanzmann’s disease), drug therapy (aspirin, warfarin, antiinflammatory medications, streptokinase, urokinase, dextran, b-lactam antibiotics, moxalactam), disseminated intravascular coagulation, cirrhosis, uremia, myeloproliferative disorders, von Willebrand’s disease
Comments: The bleeding time test as a method to evaluate suspected hemostatic incompetence has been replaced in many laboratories with the platelet function analysis–100 assay. The bleeding time test’s ability to predict excessive bleeding in clinical situations such as surgery or invasive diagnostic procedures is poor. It may play a limited residual role in the evaluation of suspected hereditary disorders of hemostasis.
BRCA-1, BRCA-2
This test involves the detection of carriers of mutations in the gene that are characterized by predisposition to breast and ovarian cancers. Women found to carry the mutation should undergo earlier and more intensive surveillance for breast cancer. Pretest counseling should be provided before genetic testing.
Breath Hydrogen Test
Normal: This test is for bacterial overgrowth. Fasting H 2 excretion is 4.6 ± 5.1, after lactulose challenge, with an early increase of less than 12. Lactulose usually results in a colonic response more than 30 minutes after ingestion.
Elevated in: A high fasting breath H 2 level and an increase of at least 12 ppm within 30 minutes after lactulose challenge are indicative of bacterial overgrowth in the small intestine. The increase must precede the colonic response.
False positives in: accelerated gastric emptying, laxative use
False negatives in: use of antibiotics and patients who are nonhydrogen producers
B-Type Natriuretic Peptide (BNP)
Normal range: up to 100 mg/L. Natriuretic peptides are secreted to regulate fluid volume, blood pressure, and electrolyte balance. They have activity in both the central and peripheral nervous system. In humans the main source of circulatory BNP is the heart ventricles.
Elevated in: heart failure. This test is useful in the emergency department setting to differentiate heart failure patients from those with chronic obstructive pulmonary disease presenting with dyspnea. Levels are also increased in asymptomatic left ventricular dysfunction, arterial and pulmonary hypertension, cardiac hypertrophy, valvular heart disease, arrhythmia, and acute coronary syndrome.
BUN
See Urea Nitrogen
Calcium (Serum)
Normal range: 8.8-10.3 mg/dL
Elevated in:
- 1.
Malignancy: increased bone resorption via osteoclast-activating factors, secretion of pituitary hormone (PTH)–like substances, prostaglandin E 2 , direct erosion by tumor cells, transforming growth factors, colony-stimulating activity. Hypercalcemia is common in the following neoplasms:
- a.
Solid tumors: breast, lung, pancreas, kidneys, ovary
- b.
Hematologic cancers: myeloma, lymphosarcoma, adult T-cell lymphoma, Burkitt’s lymphoma
- a.
- 2.
Hyperparathyroidism: increased bone resorption, gastrointestinal (GI) absorption, and renal absorption. Hyperparathyroidism can be caused by the following conditions:
- a.
Parathyroid hyperplasia, adenoma
- b.
Hyperparathyroidism or renal failure with secondary hyperparathyroidism
- a.
- 3.
Granulomatous disorders: increased GI absorption (e.g., sarcoidosis)
- 4.
Paget’s disease: increased bone resorption, seen only during periods of immobilization
- 5.
Vitamin D intoxication, milk-alkali syndrome, increased GI absorption
- 6.
Thiazides: increased renal absorption
- 7.
Other causes: familial hypocalciuric hypercalcemia, thyrotoxicosis, adrenal insufficiency, prolonged immobilization, vitamin A intoxication, recovery from acute renal failure, lithium administration, pheochromocytoma, disseminated systemic lupus erythematosus
Decreased in:
- 1.
Renal insufficiency: hypocalcemia caused by the following:
- a.
Increased calcium deposits in bone and soft tissue secondary to increased serum PO 4 −3 level
- b.
Decreased production of 1,25-dihydroxyvitamin D
- c.
Excessive loss of 25-OHD (nephrotic syndrome)
- a.
- 2.
Hypoalbuminemia: Each decrease in serum albumin (g/L) will decrease serum calcium by 0.8 mg/dL but will not change free (ionized) calcium
- 3.
Vitamin D deficiency
- a.
Malabsorption (most common cause)
- b.
Inadequate intake
- c.
Decreased production of 1,25-dihydroxyvitamin D (vitamin D–dependent rickets, renal failure)
- d.
Decreased production of 25-OHD (parenchymal liver disease)
- e.
Accelerated 25-OHD catabolism (phenytoin, phenobarbital)
- f.
End organ resistance to 1,25-dihydroxyvitamin D
- a.
- 4.
Hypomagnesemia: hypocalcemia caused by the following:
- a.
Decreased PTH secretion
- b.
Inhibition of PTH effect on bone
- a.
- 5.
Pancreatitis, hyperphosphatemia, osteoblastic metastases: Hypocalcemia is secondary to increased calcium deposits (bone, abdomen).
- 6.
Pseudohypoparathyroidism: autosomal recessive disorder characterized by short stature, shortening of metacarpal bones, obesity, and mental retardation. Hypocalcemia is secondary to congenital end organ resistance to PTH.
- 7.
Idiopathic hypoparathyroidism, surgical removal of parathyroids (e.g., neck surgery)
- 8.
“Hungry bones syndrome”: rapid transfer of calcium from plasma into bones after removal of a parathyroid tumor
- 9.
Sepsis
- 10.
Massive blood transfusion (as a result of EDTA in blood)
Table 2.6 summarizes a differential diagnosis of hypocalcemia based on laboratory evaluation.
| Diagnosis | Plasma Tests | Urine Tests | Comments | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ca | PO 4 | PTH | 25(OH)D | 1,25(OH) 2 D | cAMP | cAMP after PTH | TmP/GFR | TmP/GFR after PTH | Ca | ||
| Hypoparathyroidism | ↓ | ↑ | N/↓ | N | ↓ | ↓ | ↑↑ | ↓ | ↓↓ | N/↓ | Deficiency of PTH |
| Pseudohypoparathyroidism type I | ↓ | ↑ | ↑↑ | N | ↓ | ↓ | NC | ↑ | ↑ | N/↓ | Resistance to PTH; patients may have Albright’s hereditary osteodystrophy and resistance to multiple hormones |
| Type II | ↓ | N | ↑↑ | N | ↓ | ↓ | ↑ | ↑ | ↑ | N/↓ | Renal resistance to cAMP |
| Vitamin D deficiency | ↓ | N/↓ | ↑↑ | ↓↓ | N/↓ | ↑ | ↑ | ↓ | ↓ | ↓↓ | Deficient supply (e.g., nutrition) or absorption (e.g., pancreatic insufficiency) of vitamin D |
| Vitamin D–dependent rickets | |||||||||||
| Type I | ↓ | N/↓ | ↑↑ | N | ↓ | ↑ | ↓ | ↓ | ↓↓ | Deficient activity of renal 25(OH)D-1α-hydroxylase | |
| Type II | ↓ | N/↓ | ↑↑ | N | ↑↑ | ↑ | ↓ | ↓↓ | Resistance to 1,25(OH) 2 D | ||
Calcium, Urine
See Urine Calcium
Cancer Antigen 15-3 (CA 15-3)
Normal: <30 U/mL
Elevated in: approximately 80% of women with metastatic breast cancer. Clinical sensitivity is 0.60, specificity 0.87, positive predictive value 0.91. This test is generally used to predict recurrence of breast cancer and to evaluate response to therapy. May also be elevated in liver cancer, pancreatic cancer, ovarian cancer, and colorectal cancer. Elevations can also occur with benign breast and liver disease.
Cancer Antigen 27-29 (CA 27-29)
Normal: <38 U/mL
Elevated in: approximately 75% of women with metastatic breast cancer. Clinical sensitivity is 0.57, specificity 0.97, positive predictive value 0.83, negative predictive value 0.92. This test is generally used to predict recurrence of breast cancer and to evaluate response to therapy. May also be elevated in liver cancer, pancreatic cancer, ovarian cancer, and colorectal cancer. Elevations can also occur with benign breast and liver disease.
Captopril Stimulation Test
Normal: This test is performed by giving 25 mg captopril orally after overnight fast. The patient should be seated during the test. After captopril administration, aldosterone is less than 15 ng/dL, renin greater than 2 ng Al/mL/hr.
Interpretation: In patients with primary aldosteronism, plasma aldosterone remains high and plasma renin activity remains low after captopril administration.
Carboxyhemoglobin (COHb)
Normal: saturation of hemoglobin <2%; smokers <9% (coma: 50%; death: 80%)
Elevated in: smoking, exposure to smoking, exposure to automobile exhaust fumes, malfunctioning gas-burning appliances
Fig. 2.3 illustrates the effects of oxygen on the dissociation of CO from carboxyhemoglobin.

Cardiac Markers (Serum)
Fig. 2.4 describes typical cardiac marker diagnostic window curves and serum levels after myocardial infarction.

Cardiac Troponins
See Troponins, Serum
Carcinoembryonic Antigen (CEA)
Normal range: nonsmokers: 0 to 2.5 ng/mL; smokers: 0 to 5 ng/mL
Elevated in: Colorectal carcinomas, pancreatic carcinomas, and metastatic disease usually produce higher elevations (>20 ng/mL); carcinomas of the esophagus, stomach, small intestine, liver, breast, ovary, lung, and thyroid usually produce lesser elevations; benign conditions (smoking, inflammatory bowel disease, hypothyroidism, cirrhosis, pancreatitis, infections) usually produce levels less than 10 ng/mL.
CD4 T-Lymphocyte Count (CD4 T-Cells)
Calculated as total white blood cells × % lymphocytes × % lymphocytes stained with CD4.
This test is used primarily to evaluate immune dysfunction in human immunodeficiency virus (HIV) infection and should be measured periodically in all HIV-infected persons. It is useful as a prognostic indicator and as a criterion for initiating prophylaxis for several opportunistic infections that are sequelae of HIV infection. Progressive depletion of CD4 T-lymphocytes is associated with an increased likelihood of clinical complications. Adolescents and adults with HIV are classified as having acquired immune deficiency syndrome (AIDS) if their CD4 lymphocyte count is less than 200/μL or if their CD4 T-lymphocyte percentage is less than 14%. Corticosteroids decrease CD4 T-cell percentage and absolute number.
CD40 Ligand
Normal: <5 mcg/L. CD40 ligand is a soluble protein that is shed from activated leukocytes and platelets and used in risk stratification for acute coronary syndrome.
Elevated in: acute coronary syndrome. Increased CD40 ligand is associated with higher incidence of death or nonfatal myocardial infarction.
Cerebrospinal Fluid (CSF)
Normal range:
Appearance: clear
Glucose: 40 to 70 mg/dL
Protein: 20 to 45 mg/dL
Chloride: 116 to 122 mEq/L
Pressure: 100 to 200 mm H 2 O
Cell count (cells/mm 3 ) and cell type: <6 lymphocytes, no polymorphonucleocytes
Interpretation of results:
- 1.
Appearance of the fluid:
- a.
Clear fluid indicates that results are normal.
- b.
Yellow (xanthochromia) in the supernatant of centrifuged CSF within 1 hour or less after collection is usually the result of previous bleeding (subarachnoid hemorrhage); it may also be caused by increased CSF protein, melanin from meningeal melanosarcomas, or carotenoids.
- c.
Pinkish color is usually the result of a bloody tap; the color generally clears progressively from tubes 1 to 4 (the supernatant is usually crystal clear in traumatic taps).
- d.
Turbidity usually indicates the presence of leukocytes (bleeding introduces approximately 1 WBC/500 red blood cells [RBCs] into the CSF).
- a.
- 2.
CSF pressure: Elevated pressure can be seen with meningitis, meningoencephalitis, pseudotumor cerebri, mass lesions, and intracerebral bleeding.
- 3.
Cell count: In adults the CSF is normally free of cells (although up to 5 mononuclear cells/mm 3 is considered normal); the presence of granulocytes is never normal.
- a.
Neutrophils: These are seen in bacterial meningitis, early viral meningoencephalitis, and early tuberculosis (TB) meningitis.
- b.
Increased lymphocytes are seen in TB meningitis, viral meningoencephalitis, syphilitic meningoencephalitis, and fungal meningitis.
- a.
- 4.
Protein: Serum proteins are generally too large to cross the normal blood-CSF barrier; however, increased CSF protein is seen with meningeal inflammation, traumatic tap, increased CNS synthesis, tissue degeneration, obstruction to CSF circulation, and Guillain-Barré syndrome.
- 5.
Glucose:
- a.
Decreased glucose is seen with bacterial meningitis, TB meningitis, fungal meningitis, subarachnoid hemorrhage, and some cases of viral meningitis.
- b.
A mild increase in CSF glucose can be seen in patients with very elevated serum glucose levels.
- a.
Table 2.7 summarizes characteristic cerebrospinal fluid abnormalities.
| Turbidity and Color | Opening Pressure | WBC Count | Differential Cells | RBC Count | Protein | Glucose | |
|---|---|---|---|---|---|---|---|
| Normal | Clear, colorless | 70–180 mm H 2 O | 0–5 cells/μL 3 | Mononuclear | 0 | <60 mg/dL | > serum |
| Bacterial meningitis | Cloudy, straw colored | ↑ | ↑↑ | PMNs | 0 | ↑↑ | ↓ |
| Viral meningitis | Clear or cloudy, colorless | ↑ | ↑ | Lymphocytes | 0 | ↑ | Normal |
| Fungal and tuberculous meningitis | Cloudy, straw colored | ↑ | ↑ | Lymphocytes | 0 | ↑↑ | ↓↓ |
| Viral encephalitis | Clear or cloudy, straw colored | Normal to ↑ | ↑ | Lymphocytes | 0 (herpes ↑) | Normal to ↑ | Normal |
| Subarachnoid hemorrhage | Cloudy, pink | ↑ | ↑ | PMNs and lymphocytes | ↑↑ | ↑ | Normal (early); ↓ (late) |
| Guillain-Barré syndrome | Clear, yellow | Normal to ↑ | 0-5 cells/μL 3 | Mononuclear | 0 | ↑ | Normal |
Ceruloplasmin (Serum)
Normal range: 20 to 35 mg/dL
Elevated in: pregnancy, estrogen therapy, oral contraceptive use, neoplastic diseases (leukemias, Hodgkin’s lymphoma, carcinomas), inflammatory states, systemic lupus erythematosus, primary biliary cirrhosis, rheumatoid arthritis
Decreased in: Wilson’s disease (values often <10 mg/dL), nephrotic syndrome, advanced liver disease, malabsorption, total parenteral nutrition, Menkes’ syndrome
Chlamydia Group Antibody Serologic Test
Test description: Acute and convalescent sera are drawn 2 to 4 weeks apart. A fourfold increase in titer between acute and convalescent sera is necessary for confirmation. A single titer 1:64 or higher is considered indicative of psittacosis or lymphogranuloma venereum.
Chloride (Serum)
Normal range: 95 to 105 mEq/L
Elevated in: dehydration, sodium loss greater than chloride loss, respiratory alkalosis, excessive infusion of normal saline solution, cystic fibrosis, hyperparathyroidism, renal tubular disease, metabolic acidosis, prolonged diarrhea, acetazolamide administration, diabetes insipidus, ureterosigmoidostomy
Decreased in: vomiting, gastric suction, primary aldosteronism, congestive heart failure, syndrome of inappropriate antidiuretic hormone secretion, Addison’s disease, salt-losing nephritis, continuous infusion of D 5 W, thiazide diuretic administration, diaphoresis, diarrhea, burns, diabetic ketoacidosis
Chloride, Urine
See Urine Chloride
Cholesterol, Total
Normal: generally <200 mg/dL
Elevated in: primary hypercholesterolemia, biliary obstruction, diabetes mellitus, nephrotic syndrome, hypothyroidism, primary biliary cirrhosis, diet high in cholesterol and total and saturated fat, third trimester of pregnancy, drug therapy (steroids, phenothiazines, oral contraceptives)
Decreased in: use of lipid-lowering agents (statins, niacin, ezetimibe, cholestyramine, colesevelam), starvation, malabsorption, abetalipoproteinemia, hyperthyroidism, hepatic failure, carcinoma, infection, inflammation
Chorionic Gonadotropin (hCG), Human (Serum)
Normal, serum:
Male: <0.7 IU/L
Female premenopausal: <0.8 IU/L
Female postmenopausal: <3.3 IU/L
Elevated in: pregnancy, choriocarcinoma, gestational trophoblastic neoplasia (including molar gestations), placental site trophoblastic tumors. Human antimouse antibodies can produce false serum assay for hCG.
The principal use of this test is to diagnose pregnancy. In pregnancy, the concentration of hCG increases significantly during the initial 6 weeks of pregnancy. Peak values approaching 100,000 IU/L occur 60 to 70 days after implantation.
hCG levels generally double every 1 to 3 days. In patients with concentration less than 2000 IU/L, an increase of serum hCG less than 66% after 2 days is suggestive of spontaneous abortion or ruptured ectopic gestation.
Circulating Anticoagulant (Antiphospholipid Antibody, Lupus Anticoagulant)
Normal: negative
Detected in: systemic lupus erythematosus, drug-induced lupus, long-term phenothiazine therapy, multiple myeloma, ulcerative colitis, rheumatoid arthritis, postpartum, hemophilia, neoplasms, chronic inflammatory states, acquired immune deficiency syndrome, nephrotic syndrome
Note : The name is a misnomer because these patients are prone to hypercoagulability and thrombosis.
CK
See Creatine Kinase
Clonidine Suppression Test
Interpretation: Clonidine inhibits neurogenic catecholamine release and will cause a decrease in plasma norepinephrine into the reference interval in hypertensive subjects without pheochromocytoma. The test is performed by giving 4.3 mg clonidine/kg orally after overnight fast. Norepinephrine is measured at 3 hours. Result should be within established reference range and decrease to less than 50% of baseline concentration. Lack of decrease in norepinephrine is suggestive of pheochromocytoma.
Coagulation Factors
Factor reference ranges:
V: >10%
VII: >10%
VIII: 50% to 170%
IX: 60% to 136%
X: >10%
XI: 50% to 150%
XII: >30%
Fig. 2.5 illustrates the blood coagulation pathways.

Complement (C3, C4)
Normal range: C3: 70 to 160 mg/dL; C4: 20 to 40 mg/dL
Abnormal values:
Decreased C3: active systemic lupus erythematosus (SLE), immune complex disease, acute glomerulonephritis, inborn C3 deficiency, membranoproliferative glomerulonephritis, infective endocarditis, serum sickness, autoimmune or chronic active hepatitis
Decreased C4: immune complex disease, active SLE, infective endocarditis, inborn C4 deficiency, hereditary angioedema, hypergammaglobulinemic states, cryoglobulinemic vasculitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree