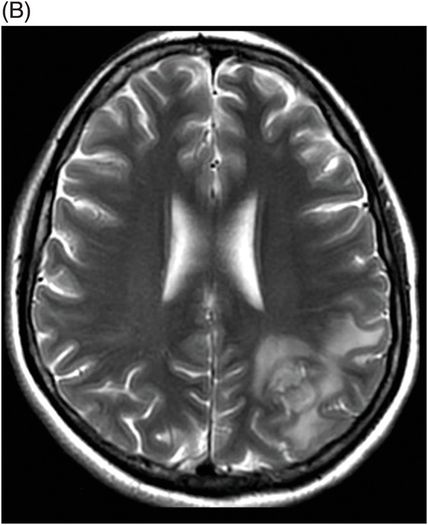
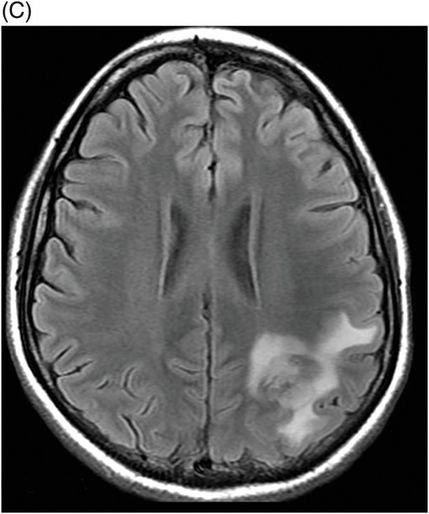
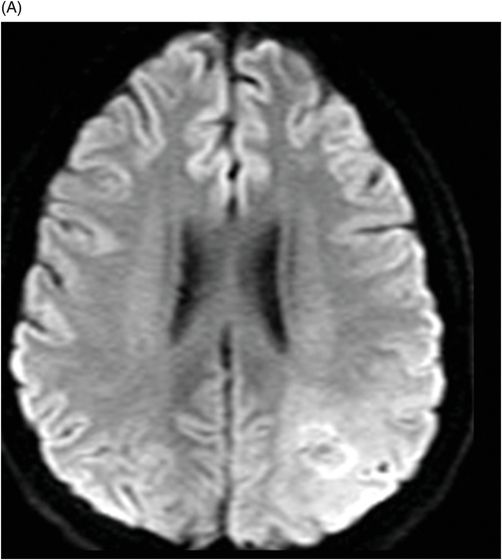
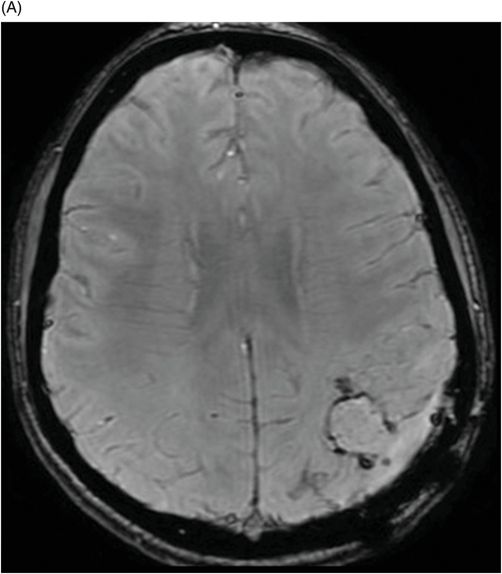
(A) Axial diffusion, (B) Axial SWI, and (C) Axial T1WI through the level of the inferior parietal lobule.
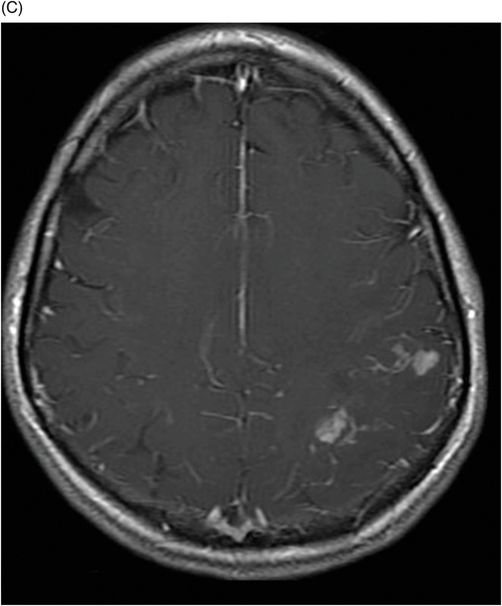
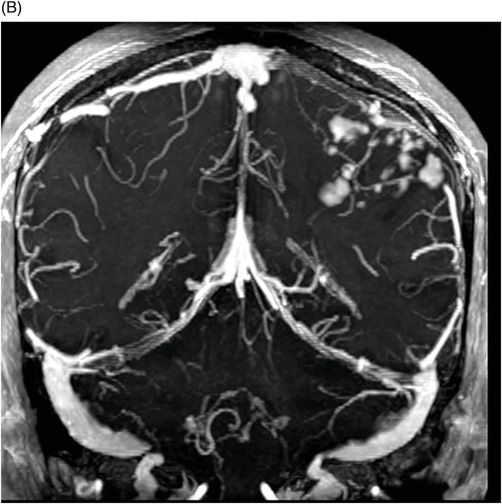
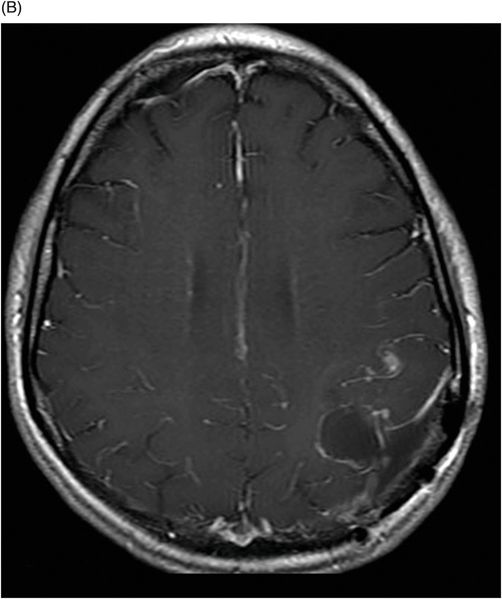
(A) Axial SWI, and (B) Axial T1WI postgadolinium images through the level of the inferior parietal lobule (following surgical biopsy).
Parenchymal Neurosarcoidosis
Primary Diagnosis
Parenchymal neurosarcoidosis
Differential Diagnoses
Lymphoma
Other granulomatous diseases
Meningioangiomatosis and fungal infections
Imaging Findings
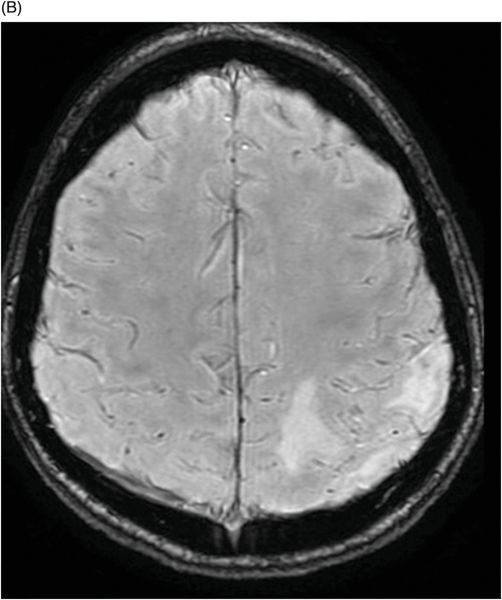
Fig. 54.1: (A) Sagittal T1WI, (B) Axial T2WI, and (C) Axial FLAIR images of the brain demonstrated subcortical signal abnormality at the left inferior parietal lobule associated with vasogenic edema. Fig. 54.2: (A) Axial diffusion, (B) Axial SWI, and (C) Axial T1WI of the brain demonstrated subcortical signal abnormality, with nodular foci of enhancement at the left inferior parietal lobule. Fig. 54.3: Axial SPGR T1WI postgadolinium with multiplanar reconstruction image. (A) Sagittal and (B) Coronal reconstructed images of the brain showed multiple areas of nodular enhancement in the left inferior parietal lobule. Fig. 54.4: (A) Postsurgical, axial SWI, and (B) Axial T1 postgadolinium image showing the surgical cavity.
Discussion
Neurosarcoidosis is a chronic systemic disease of unknown etiology although current opinion favors an immune mechanism. This disorder is characterized by the presence of non-caseating granulomas with proliferation of epithelioid cells in affected organs. Lesions can be seen in the lungs, lymphatic system, eyes, skin, liver, spleen, salivary glands, heart, nervous system, muscles, and bones, although the lungs and the draining mediastinal lymph nodes are the most common sites of involvement.
The clinical manifestations of neurosarcoidosis depend on the site of granuloma involvement and are non-specific. Subacute loss of central vision with retrobulbar pain was the most prevalent symptom, followed by bilateral affection of optic nerves, facial nerve impairment, and hearing loss due to vestibulocochlear pair lesion. Spinal cord involvement may present clinically with lower extremity weakness and other non-specific signs of myelopathy.
The proposed criteria for the diagnosis of neurosarcoidosis are: Definite – Clinical presentation suggestive of neurosarcoidosis with exclusion of other possible diagnoses and the presence of positive nervous system histology; Probable – Clinical syndrome suggestive of neurosarcoidosis with laboratory support for CNS inflammation (elevated level of CSF protein and/or cells, the presence of oligoclonal bands and/or MRI evidence compatible with neurosarcoidosis) and exclusion of alternative diagnoses together with evidence for systemic sarcoidosis (either through positive histology, including Kveim test, and/or at least two indirect indicator from Gallium scan, chest imaging, and serum ACE); Possible – Clinical presentation suggestive of neurosarcoidosis with exclusion of alternative diagnoses where the above criteria are not met.
Neurosarcoidosis has a wide spectrum of imaging findings because of the capacity to involve any part of the nervous system. Most common imaging findings include multiple white matter lesions, focal dural thickening and enhancement, optic nerve enhancement, leptomeningeal involvement including involvement of the other cranial nerves, and intraparenchymal mass lesion with or without involvement around the perivascular spaces. Spinal cord involvement may also occur.
Enhancing parenchymal mass lesions are a frequent finding and characteristically have low sign intensity on T2WI images. Central necrotic component is typically absent in intraparenchymal neurosarcoid granulomas. There is no definite predilection for the intraparenchymal lesions. Mass-like intraparenchymal lesion can occur in any lobe of the brain. However, spread along the prevascular spaces is more common in the basal ganglia. Intraparenchymal lesions are frequently associated with adjacent leptomeningeal affection. The leptomeningeal finding is characterized by diffuse or nodular thickening and enhancement of the leptomeninges. When the leptomeningeal involvement is around the hypothalamus and pituitary infundibulum, patients may present with diabetes insipidus and other hormonal disturbances. Cranial nerve impairment is also very common and is especially prevalent in the optic and facial cranial nerves; imaging findings are enlargement and enhancement on contrast T1-weighted images. Pachymeningeal thickening and enhancement can also occur, such as a vasculitis-like pattern of involvement of the intracranial vasculature. Spinal involvement may present as nodular or diffuse leptomeningeal and dural lesions or intramedullary impairment.
A confident diagnosis of neurosarcoidosis is often difficult, particularly when the clinician is presented with an isolated CNS disorder that is likely to have an inflammatory basis. The nervous system is a relatively uncommon site for the disease to manifest and consequently, investigation to establish a diagnosis has centered on searching for histologic confirmation in other organs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree