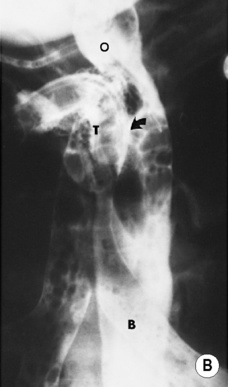
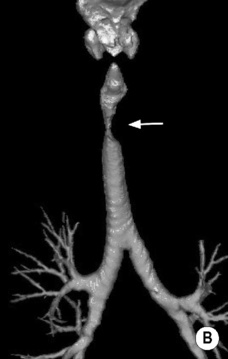
• The immediate subglottic trachea has a normal diameter but expands as it passes to the carina (and continuing into the major bronchi) • It is often associated with tracheal diverticulosis, recurrent lower respiratory tract infections and bronchiectasis
Large airway disease
TRACHEAL DISORDERS
POST-TRAUMATIC STRICTURES
TRACHEAL DISORDERS
AMYLOIDOSIS
TRACHEOBRONCHOMEGALY (MOUNIER–KUHN DISEASE)
Definition
 atrophic mucosa prolapses between the cartilage rings giving the trachea a corrugated outline (this may become exaggerated to form sacculations)
atrophic mucosa prolapses between the cartilage rings giving the trachea a corrugated outline (this may become exaggerated to form sacculations)

 it typically involves the trachea above the level of the thoracic inlet
it typically involves the trachea above the level of the thoracic inlet it involves 1.5–2.5cm of tracheal wall
it involves 1.5–2.5cm of tracheal wall
 it is also seen with TB, rhinoscleroma and necrotizing invasive aspergillosis
it is also seen with TB, rhinoscleroma and necrotizing invasive aspergillosis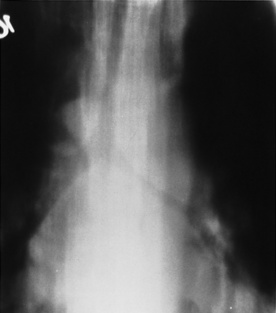
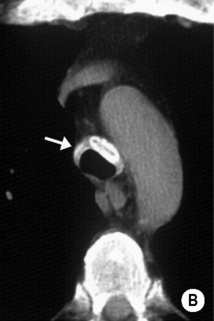
 it is characterized by gas within a cavitated hilar or mediastinal lymphadenopathy
it is characterized by gas within a cavitated hilar or mediastinal lymphadenopathy infection and trauma are other causes
infection and trauma are other causes
 a smoothly marginated intraluminal polyp (hamartomas and lipomas may demonstrate fat attenuation)
a smoothly marginated intraluminal polyp (hamartomas and lipomas may demonstrate fat attenuation) it is often sessile and eccentric resulting in asymmetrical luminal narrowing
it is often sessile and eccentric resulting in asymmetrical luminal narrowing  can be polypoid and mostly intraluminal (with mediastinal extension seen in 30–40%)
can be polypoid and mostly intraluminal (with mediastinal extension seen in 30–40%)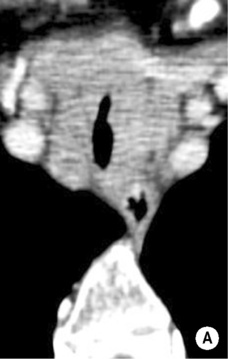
 it usually involves the larynx – occasionally extension into the trachea and proximal bronchi is seen
it usually involves the larynx – occasionally extension into the trachea and proximal bronchi is seen although benign it may undergo transformation to a squamous cell carcinoma
although benign it may undergo transformation to a squamous cell carcinoma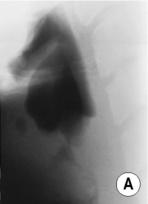

 It is seen in association with tracheobronchomegaly, COPD, relapsing polychondritis and following trauma
It is seen in association with tracheobronchomegaly, COPD, relapsing polychondritis and following trauma a coronal tracheal diameter significantly larger than the sagittal diameter (producing a lunate configuration)
a coronal tracheal diameter significantly larger than the sagittal diameter (producing a lunate configuration)
 nodular or polypoid lesions may be seen on the inner airway contour
nodular or polypoid lesions may be seen on the inner airway contour  luminal stenosis may affect any main, lobar or segmental bronchus
luminal stenosis may affect any main, lobar or segmental bronchus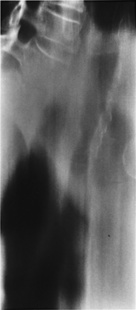
 usually there is a symmetrical subglottic stenosis – with disease progression the distal trachea and bronchi may become involved
usually there is a symmetrical subglottic stenosis – with disease progression the distal trachea and bronchi may become involved early sparing of the posterior tracheal wall (circumferential involvement with advanced disease)
early sparing of the posterior tracheal wall (circumferential involvement with advanced disease)  the trachea may become flaccid with considerable collapse at expiration
the trachea may become flaccid with considerable collapse at expiration  fibrotic cartilaginous ring destruction may cause stenosis
fibrotic cartilaginous ring destruction may cause stenosis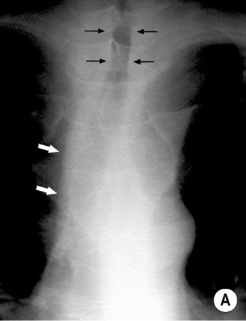
 dystrophic calcification or ossification is frequently present
dystrophic calcification or ossification is frequently present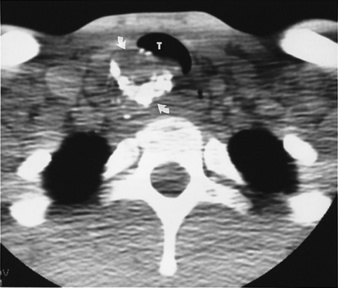
 the narrowing usually affects the whole intrathoracic trachea (with an abrupt return to a normal calibre at the thoracic inlet)
the narrowing usually affects the whole intrathoracic trachea (with an abrupt return to a normal calibre at the thoracic inlet)  frequently there is calcification of the tracheal cartilage rings
frequently there is calcification of the tracheal cartilage rings
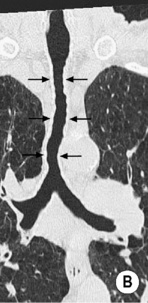
 diameters > 2.4 and 2.3cm for the right and left main bronchi, respectively
diameters > 2.4 and 2.3cm for the right and left main bronchi, respectively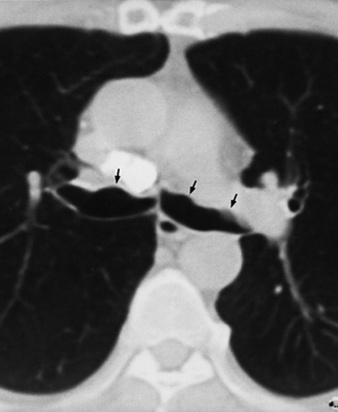
 the nodules contain heterotopic bone, cartilage and calcified acellular protein matrix with normal overlying bronchial mucosa
the nodules contain heterotopic bone, cartilage and calcified acellular protein matrix with normal overlying bronchial mucosa  M>F (usually > 50 years old)
M>F (usually > 50 years old) nodules may protrude from the anterior and lateral luminal walls into the lumen (usually with foci of calcification)
nodules may protrude from the anterior and lateral luminal walls into the lumen (usually with foci of calcification)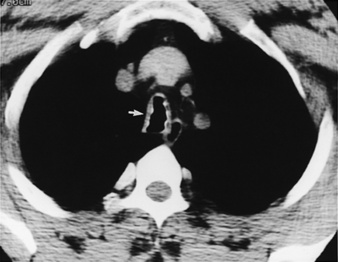
 the mechanisms include:
the mechanisms include:

 sputum
sputum  haemoptysis
haemoptysis  digital clubbing
digital clubbing overinflation is often present with generalized disease (atelectasis can be seen with localized forms)
overinflation is often present with generalized disease (atelectasis can be seen with localized forms)  thickened bronchial walls:
thickened bronchial walls:






