Larynx
The mucosal surface of the larynx is well evaluated by laryngoscopy, with the role of imaging to determine deep tumor extent and tumor margins. The epiglottis has an upper free margin and is attached inferiorly to the thyroid cartilage. The hyoid bone is the ceiling from which the larynx is suspended. The largest of the laryngeal cartilages is the thyroid cartilage consisting of an anterior body, two small superior horns (cornua), and two large posterior horns. The thyrohyoid membrane extends from the hyoid bone superiorly to the superior cornua inferiorly. Inferior to the thyroid cartilage is the cricoid cartilage, which resembles a “signet” ring that faces posteriorly. The inferior margin of the cricoid cartilage is the junction between the larynx and trachea. The cricothyroid membrane closes the gap between the cricoid and the thyroid cartilages. The arytenoid cartilages articulate superolaterally with the cricoid posteriorly. The thyroarytenoid (vocalis) muscles attaches to the lower anterior surface of the arytenoid, forming the bulk of the true vocal cord. The true cord is inferior to the false cord, with the glottis defined as the horizontal space between the true and false vocal cords.
The valleculae are the small bilateral recesses between the tongue base and free margin of the epiglottis. The aryepiglottic folds lie above the false vocal cords, and form the lateral margins of the vestibule (the supraglottic airspace), extending from the arytenoid cartilages to the free margin of the epiglottis. The pyriform sinuses are lateral to the aryepiglottic folds, being mucosal recesses between the thyroid cartilage and the aryepiglottic folds. The ventricles are the lateral recesses between the true and false cords. The anterior commissure lies in the midline between the true vocal cords anteriorly, and, on thin section CT at this level, air should directly abut the thyroid cartilage. In a Valsalva maneuver, the patient attempts to exhale against a closed glottis, with the true cords adducted. In quiet respiration, the true cords will be slightly abducted but not completely effaced.
Innervation of the larynx is by the recurrent laryngeal nerve (RLN). These paired nerves emerge from the vagus nerve with different courses. The right RLN arises at the level of, and loops under, the subclavian artery while the left arises at the level of the aortopulmonary window and loops under the aorta. The nerves then ascend in the tracheoesophageal grooves. Supraglottic lymphatics drain to upper jugular nodes and subglottic lymphatics drain to paratracheal and pretracheal nodes and then, eventually, to lower jugular nodes.
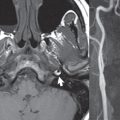
A Zenker diverticulum is a posterior outpouching of the pharyngeal wall just above the cricopharyngeus muscle (thus just above the esophagus). The cricopharyngeus muscle is often prominent, with the diagnosis of a Zenker diverticulum typically made on the basis of a barium swallow.
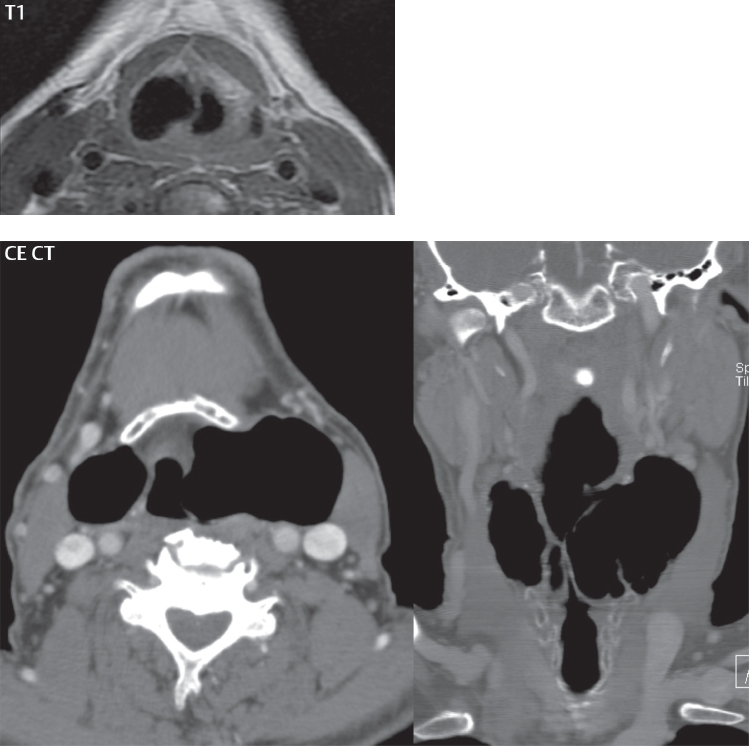
A laryngocele is a dilatation of the laryngeal ventricle. They are typically air-filled but may be fluid-filled in which case they are termed saccular cysts. The classic acquired laryngocele was seen in glassblowers and trumpet players, due to constant increased pressure in the larynx with forced expiration. They may also be caused by an obstructing tumor. A laryngocele may be internal (confined within the larynx) ( Fig. 2.98 ) or external (extending through the thyrohyoid membrane).
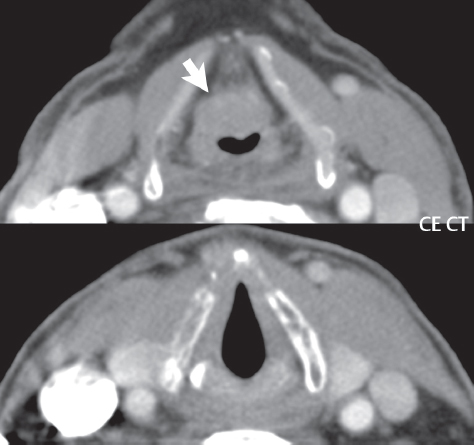
Foreign bodies can result from ingestion or aspiration. A foreign body may initially lodge in the pyriform sinus, from which point it can migrate into the larynx ( Fig. 2.99 ).

Ninety-five percent of all malignancies of the larynx are squamous cell carcinoma. These tumors arise on the mucosal surface, with deep lesion extent relative to precise landmarks not possible to be assessed by endoscopy, thus the role of imaging. Smoking and heavy consumption of alcohol are important risk factors. Treatment options include several voice sparing operations, typically coupled with radiation therapy ( Fig. 2.100 ). The supraglottic region includes the false vocal cords, aryepiglottic folds, preepiglottic and paraglottic spaces, and epiglottis. In a supraglottic laryngectomy (which is voice sparing), the larynx above the ventricle is removed, with the resection line made through the ventricle. The key to feasibility is inferior tumor extension ( Fig. 2.101 ) and tumor must be clearly separated from the anterior commissure. Part of one arytenoid can be removed, but the thyroid cartilage cannot be involved by tumor. Lymph node involvement with supraglottic tumor is common. Tumors of the true vocal cord (glottic carcinomas) present early, due to a change in voice (early vocal cord paralysis), with lymph node involvement uncommon. Contraindications to surgery, specifically hemilaryngectomy (unilateral removal of the true and false cords, and thyroid ala—an operation which is also voice sparing), include extension across the anterior commissure, subglottic extension, involvement of the cricoarytenoid joint, and thyroid cartilage invasion. Cartilage involvement is best identified on MR by the demonstration of cartilage enhancement. Tumors of the subglottic larynx (inferior surface of true vocal cords to cricoid cartilage) are least common, often presenting as T4 lesions (defined by invasion of the thyroid cartilage and/or extension beyond the larynx). Cricoid invasion is common. Large lesions require total laryngectomy and radiation therapy.

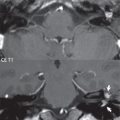
In unilateral vocal cord paralysis the affected vocal cord rests in a paramedian position. Etiologies outside of the larynx include malignancy involving the vagus or recurrent laryngeal nerves, and iatrogenic injury (prior surgery, especially thyroid).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree