Discussion
As you looked at this film, you noticed, of course, the endotracheal tube malpositioned in the left mainstem bronchus. You also noticed the lack of definition of the left heart border and the increased density in the perihilar regions. You recognize that the endotracheal tube is occluding the lingular segment of the left upper lobe, indicating left upper lobe collapse, resulting in obliteration of the left heart border. The endotracheal tube was moved back into its proper position, approximately 4 cm above the carina, and the lingular segment of the left upper lobe reaerated.
This 68-year-old patient is now 3 days post cardiac bypass surgery and is doing very well. This film was taken after the patient had been extubated.
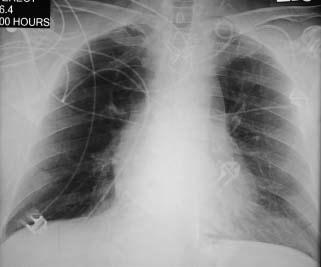
Discussion
The patient is doing extremely well and aerating well without an effusion. You do notice the coiling of the left subclavian central line. Approximately 30% of all lines inserted are in poor position and need to be replaced.
This patient suddenly lost consciousness while visiting his wife in the hospital. He was brought to the emergency department, where it was discovered that he was in ventricular fibrillation, and he was resuscitated. He was then transferred to the cardiac catheterization laboratory.
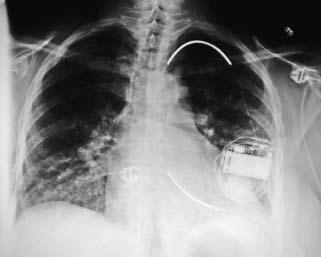
Discussion
This patient had what type of device inserted? You notice the somewhat peculiar position of the intraventricular cardiac defibrillator (ICD). First, it is worth remembering the characteristic appearance of this device. Note how it differs from a pacemaker. The distal end is thicker with a serrated area. Proximally, another wider serrated area, approximately 3 in. in length, is seen. These are the defibrillator parts of the ICD. In this patient, however, note the position of the device. What ventricle should this be in? It should be in the right ventricle, and here, in the haste and confusion surrounding this patient’s care, it was unfortunately inserted in the arterial side, so that the ICD is in the apex of the left ventricle.
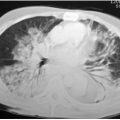
This 60-year-old female arrived in the hospital with a large right pleural effusion, which was tapped and discovered to be tuberculosis. A chest tube was placed to drain the effusion. The chest tube was not functioning well, and a portable film was obtained.

Discussion
In this film you can immediately identify the reason the chest tube is not functional. It is not in the pleural space but rather in the subcutaneous tissues. There is, on careful observation, some air in the subcutaneous tissue. Again note the large right effusion with compressive atelectasis. A central line is into the superior vena cava.
This 77-year-old patient presented to the emergency department in shock, with severe chest pain, having sustained a large anterolateral myocardial infarct. He was admitted to the ICU, where a Swan-Ganz catheter was placed. His wedge pressure was recorded during the night as 17 mm Hg, and you arrived in the morning to see this film.

Discussion
The portable film reveals considerable cardiomegaly, and a SwanGanz catheter that was introduced via the right internal jugular route. Did you notice anything abnormal about the Swan-Ganz catheter? Of course, the catheter is placed too far peripherally into the right lower lobe pulmonary artery. Proper position should be in the right main pulmonary artery. In addition, if you look carefully at the tip, you can see that the balloon is still inflated. The balloon was inflated and was not deflated after the wedge pressure was obtained. A pulmonary infarct developed distal to the position of the catheter in the right lower lobe. There are two feared complications with the SwanGanz catheter, and this is one of them. In addition to thrombosis, there is always the danger that inflating the balloon at the tip of the Swan-Ganz catheter may cause a small pulmonary artery to rupture, and the patient will develop intrapulmonary hemorrhage.
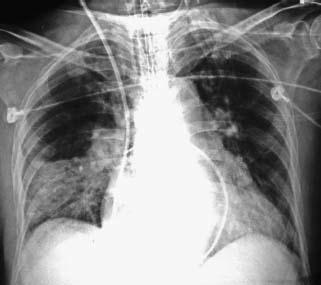
On this film, taken later, the catheter has been withdrawn into a normal position in the right main pulmonary artery, but the area of infarction is still seen.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree