KEY FACTS
Imaging
- •
Hepatic artery stenosis
- ○
Elevated peak systolic velocity at anastomosis > 200-250 cm/s
- ○
Parvus tardus waveforms in intrahepatic arteries
- –
Acceleration time > 0.08 s
- –
Resistive index < 0.5
- –
- ○
- •
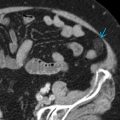
Hepatic artery thrombosis
- ○
No detectable flow in hepatic artery with color or spectral Doppler
- ○
May see “collateral transformation of hepatic artery”
- –
Tortuous collateral arteries in porta hepatis and parvus tardus intrahepatic arterial waveforms
- –
- ○
Pathology
- •
Hepatic artery stenosis
- ○
Stenosis occurs at anastomosis
- ○
Usually occurs at > 3 months post transplant
- ○
- •
Hepatic artery thrombosis
- ○
May occur < 15 days or years after transplant
- ○
Risk factors: Difference in hepatic artery caliber between donor and recipient, prolonged graft ischemia time, ABO blood group incompatibility, CMV infection, acute or chronic rejection, hypercoagulable state, sepsis
- ○
Clinical Issues
- •
Hepatic artery stenosis
- ○
May be related to injury at time of surgery or disruption of vasa vasorum with ischemia of hepatic artery
- ○
- •
Hepatic artery thrombosis
- ○
Most common immediate vascular complication (2-12%)
- ○
Complete occlusion of hepatic artery in early transplant period leads to liver failure
- –
Up to 75% of patients with hepatic artery thrombosis require retransplantation
- –
- ○
Biliary ducts in liver transplants supplied only by artery
- –
Hepatic artery thrombosis can result in biliary ischemia, bilomas, bile lakes
- –
- ○
Scanning Tips
- •
Due to patient body habitus, overlying gas or overlying surgical changes, HA may be difficult to visualize; different scanning positions (supine or LLD), different scanning windows (intercostal or subcostal), and different transducers (lower frequency transducer for large body habitus) may help
- •
If parvus tardus waveforms are seen, ensure that PW scale setting is not too high, which can mimic parvus tardus waveforms