KEY FACTS
Imaging
- •
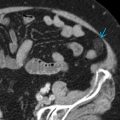
Hepatic venous stenosis
- ○
Color Doppler
- –
May see focal turbulent flow at stenosis and stenotic jet
- –
- ○
Spectral Doppler
- –
Elevated velocity at site of stenosis or < 10 cm/s away from site of stenosis
- –
Loss of normal triphasic waveform
- □
Most commonly monophasic in appearance
- □
- –
May see secondary slow portal vein velocity
- –
- ○
Angiography
- –
Pressure gradient > 5 mm Hg across stenosis
- –
- ○
- •
Hepatic venous thrombosis
- ○
Direct visualization of thrombus in hepatic vein (HV) or lack of detectable flow with color, power, or spectral Doppler
- ○
Pathology
- •
HV or inferior vena cava (IVC) stenosis results in outflow obstruction of liver
- •
Immediate posttransplant period: Kinking of vessel
- •
Delayed presentation: Intimal hyperplasia
Clinical Issues
- •
HV stenosis occurs in < 1% of liver transplants, 2-10% of liver transplants when piggyback technique used
- •
Right lobe liver graft from living donor has higher risk of developing venous congestion because of inadequate venous drainage
- •
Clinical presentation: Lower extremity edema, Budd-Chiari syndrome, ascites
- •
Treatment
- ○
Stenosis may be treated with balloon-expandable stents or angioplasty
- ○
Thrombosis may require surgery or retransplant
- ○
Scanning Tips
- •
Color Doppler box should always include HV and its IVC confluence because stenoses often occur at the junction
- •
Obtain HV spectral Doppler tracings within 3 cm of junction with IVC
- •
If area of aliasing is identified, obtain spectral Doppler with angle correction through the region