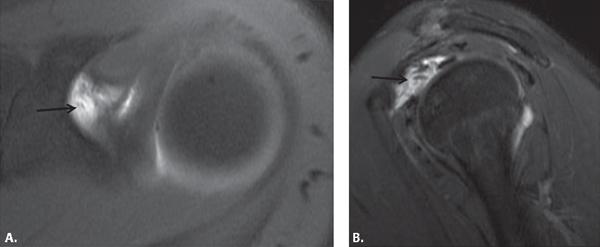
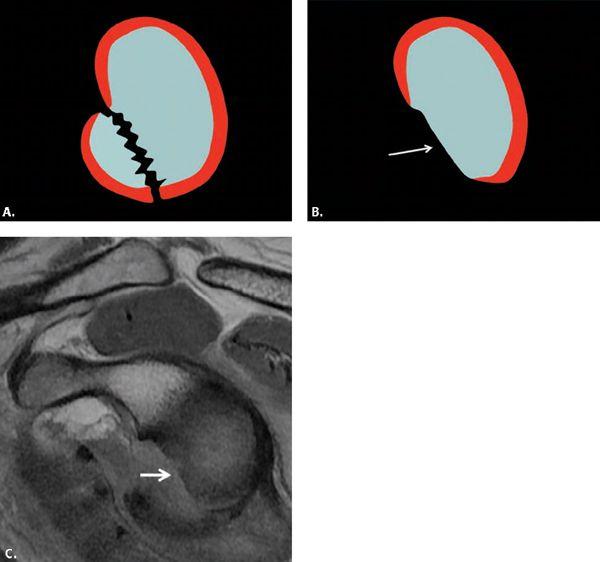
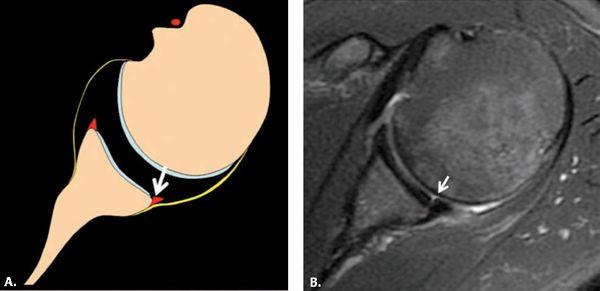
FIGURE 5.35 Glenolabral articular disruption (GLAD) lesion. A: Diagram and (B) axial fat-suppressed T1-weighted MR image from an arthrogram shows an anterior–inferior labral tear with an adjacent cartilage defect consistent with a GLAD lesion (arrow).
FIGURE 5.36 Superior glenohumeral ligament (SGHL) tear seen on (A) axial and (B) sagittal fat-suppressed T1-weighted MR arthrogram images of the shoulder at the level of the coracoid (arrow).
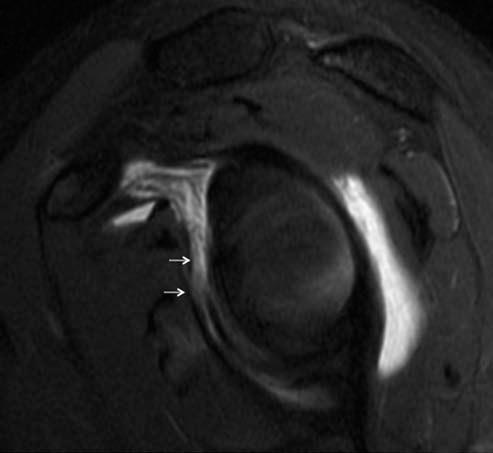
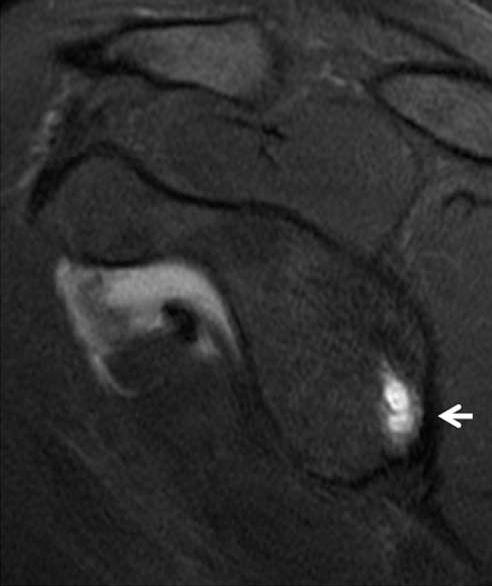
The Hill Sachs lesion manifests as a depression along the posterolateral aspect of the humeral head superiorly in the top 2 cm usually above or at the level of the coracoid (Fig. 5.44). It is seen in approximately 75% of patients with anterior instability. Although most commonly involving the bone, the lesion may just appear in the humeral head cartilage or may produce bone marrow-reactive change without cortical deformation.
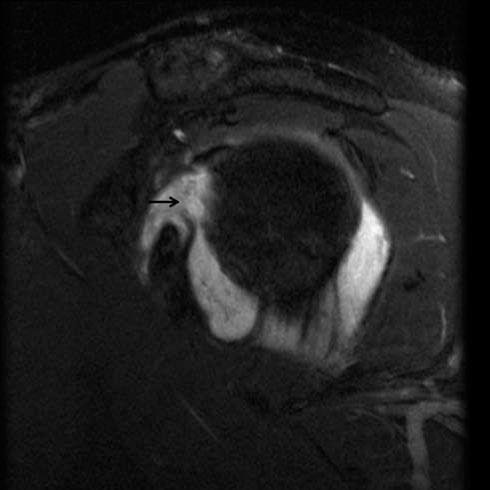
It is important to quantify the amount of bone loss in the area of the Hill Sachs defect. Large defects that are parallel to the anterior glenoid rim can engage when the shoulder goes from external to internal rotation (Fig. 5.45) resulting in recurrent instability and locking, which must be repaired with bone graft.
FIGURE 5.37 A middle glenohumeral ligament (MGHL) tear is seen as proximal discontinuity of the ligament on a sagittal fat-suppressed T2-weighted MR arthrogram (arrow).
FIGURE 5.38 Torn middle glenohumeral ligament (MGHL). The MGHL is torn from its proximal origin on this sagittal fat-suppressed T2-weighted MR image (arrow).
FIGURE 5.39 Middle glenohumeral ligament (MGHL) tear and superior labral anterior posterior (SLAP) lesion (type VII SLAP). A: Axial and (B) coronal fat-suppressed T1-weighted images from an MR arthrogram demonstrate the MGHL tear (black arrow) and the SLAP lesion (white arrow).
On MRI obtained in the acute setting of an anterior dislocation, there often is abnormal signal intensity within the marrow indicative of acute trauma (contusion) (Fig. 5.44) that will not be detected by CT. In Workman et al.’s (83) series, MRI was 97% sensitive, 91% specific, and 94% accurate for detecting Hill Sachs lesions. It was also found to be superior to arthroscopy for detecting Hill Sachs lesions.
One must be careful not to overcall a Hill Sachs lesion when there are cysts or erosions in the same area. Symptomatic cystic change in this area has been seen at the infraspinatus attachment in pitchers. Many other people have asymptomatic cysts or vessels in this location, also called the bare area (85). Also, there is a normal anatomic groove located posterolaterally on the humeral head that should not be confused with a Hill Sachs lesion (86). This groove can be distinguished from the Hill Sachs lesion by its location along the long axis of the humerus. It usually lies at least 20 mm distal to the top of the humeral head, whereas the Hill Sachs lesion is usually located in the first 18 mm of the proximal humeral head. A greater tuberosity fracture might also be confused with a Hill Sachs lesion, but it will present with fracture lines on MRI. The greater tuberosity compression related to posterior–superior glenoid impingement (PSGI) described subsequently may be difficult to distinguish from a Hill Sachs lesion. The history of an absence of prior dislocation and associated abnormalities can aid in distinction between the Hill Sachs lesion and the PSGI lesion on the humeral head.
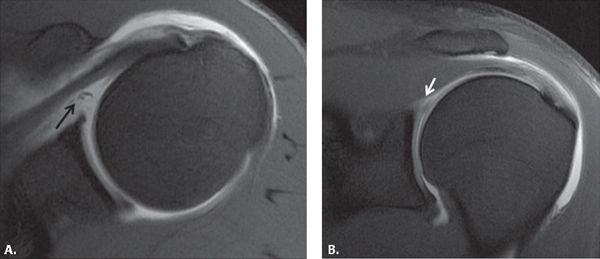
The osseous Bankart lesion results from impaction of the humeral head against the anterior glenoid during anterior dislocation of the humerus (Figs. 5.46 and 5.47). Bony Bankart lesions may be small or large enough to extend above the glenoid equator. Most osseous Bankart lesions are seen on MRI, but small fractures may be missed. The osseous Bankart fracture is well seen on CT as a fragment of bone associated with irregularity of the adjacent glenoid rim. The presence of an osseous Bank-art fracture is an indication for open repair.
The majority of patients with the diagnosis of anterior instability show some bone loss anteriorly. This is probably multifactorial in etiology. The shape of the glenoid fossa is often like a pear with a narrower superior portion compared with the inferior portion. The normally pear-shaped glenoid rim may become deficient inferiorly after anterior dislocation, producing an inverted pear configuration (82, 87) (Fig. 5.48). The inverted pear glenoid usually involves at least 25% to 33% of the width of the inferior glenoid (88). Reduced glenohumeral contact area can increase instability and the likelihood of recurrent dislocation. In patients with a deficient glenoid, a coracoid bone graft is placed in the defect using a nonarthroscopic open technique to restore the normal articular arc of the glenoid, termed the modified Latarjet procedure (89, 90). On MRI, low-signal cortical fragments or glenoid deficiency are seen in all planes, but particularly on sagittal and axial images (Fig. 5.48). CT can also be used to assess anterior glenoid bone loss (88).
Osteochondral defects (OCDs) of the glenoid fossa are not that common, but usually result from acute trauma and have a high association with instability, labral tear, and intra-articular bodies (91). In general, the concave glenoid is not as affected by OCDs as other convex articular surfaces throughout the body such as the femoral condyle or capitellum. The longstanding theory of pathogenesis is traumatic separation of the articular cartilage from the underlying bone with occlusion of a terminal artery that supplies the hyaline cartilage or embolism of an epiphyseal artery leading to osteonecrosis. The most common presentation of an OCD is that of a multiloculated lytic lesion in the subchondral bone beneath the articular cortex that demonstrates fluid signal characteristics on MRI (Fig. 5.49). Sometimes these lytic lesions of the glenoid mimic a tumor and the patients are incorrectly referred to the orthopaedic oncologist, so it is also important to recognize the appearance to make the right diagnosis of OCD and look for instability rather than put the patient through a long and invasive diagnostic workup for tumor or metastases.
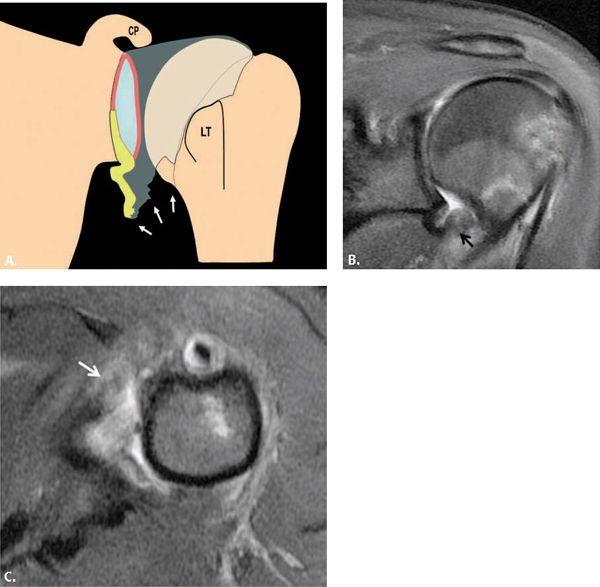
FIGURE 5.40 Humeral avulsion of the inferior glenohumeral ligament (HAGL) lesion. A: Diagram and (B) coronal and (C) axial fat-suppressed T2-weighted MR images of the glenohumeral joint shows disruption of the anterior band of the IGHL at the humeral attachment consistent with a HAGL lesion (arrows). This produces a “J”-shaped IGHL. CP, coracoid process; LT, lesser tuberosity.
Posterior Instability
Posterior labral and capsular tears are much less common than anterior ones, accounting for up to 5% of all cases of shoulder instability (92). Posterior instability is more often encountered in association with atraumatic recurrent posterior multidirectional instability or repetitive microtrauma, but can also be seen with traumatic posterior dislocation, a redundant posterior capsule, osteochondral lesions, and posterior labroligamentous tears. Posterior instability may also occur in the setting of electric shock or seizures, which produce adduction, flexion, and internal rotation of the glenohumeral joint.
Acute posterior shoulder instability typically occurs when posterior force is placed on the arm in adduction, internal rotation, and forward flexion. Overhead-throwing athletes are predisposed to this problem. One study recently concluded that posterior labral injuries are almost 15 times more common in football players than in the general population as a result of various situations in which posterior force is place on the humeral head (93). A fall on an outstretched hand with the arm abducted is another cause of posterior dislocation. Subluxations are more common than dislocations. If a dislocation occurs, it can be subacromial, subglenoid, or subspinous under the scapular spine. The rotator cuff and biceps tendon can rarely become entrapped in the joint.
The patient with posterior shoulder instability has localized pain and/or clicking more often than instability. The shoulder fatigues with activity. A history of pain or instability with the arm in forward flexion, adduction, and internal rotation will bring this to mind, but it can be confused with subacromial impingement. A “jerk” test can suggest posterior instability when the arm is placed at 90 degrees of forward elevation and internal rotation with an applied axial force (94). Sharp pain with or without a posterior clunk or click suggests a positive test result. The Kim test is another alterative method for detecting posterior instability (95). The patient sits with the arm in 90 degrees of abduction and an axial loading force is applied along with a 45-degree upward diagonal elevation of the distal arm.
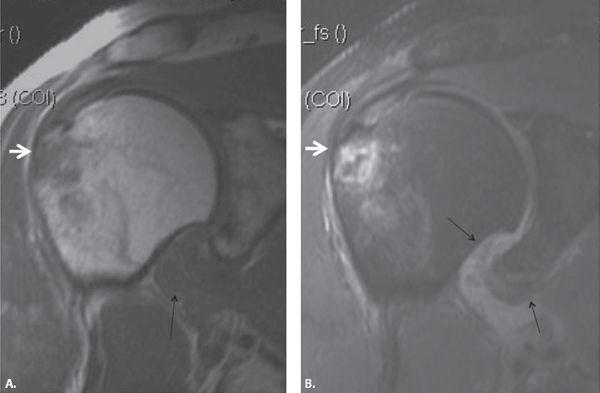
FIGURE 5.41 Floating anterior–inferior glenohumeral ligament (AIGHL). A: Coronal T1-weighted and (B) fat-suppressed T2-weighted images of a shoulder show disruption of the anterior band of the IGHL at the humeral and glenoid attachments with joint fluid extravasating outside of the joint (black arrows). Note the Hill Sachs lesion commonly associated with this lesion (white arrow).
In addition to the clinical findings, the diagnosis of acute posterior shoulder dislocation is commonly missed on radiographs. The anteroposterior view may appear normal, but there can be overlap or widening between the humeral head and glenoid and possibly an anterior humeral compression fracture (reverse Hill Sachs lesion or trough line sign) (Fig. 5.50). A transscapular or axillary view is very helpful to show the posterior subluxation or dislocation in this situation.
The structures that are important for posterior stability include those that support the posterior aspect of the glenohumeral joint: the posterior glenoid rim, labrum, and capsule as well as the rotator cuff and rotator interval. The subscapularis muscle and the rotator interval counterbalance posterior subluxation, aiding in resistance to posterior–inferior humeral translation, and therefore abnormalities of these regions will also be associated with posterior instability (49, 96).
Labral Lesions Associated With Posterior Instability
Posterior instability is associated with lesions of the posterior labrum. In one study of acute traumatic posterior shoulder dislocation evaluated with MRI in 36 patients, 60% of patients had posterocaudal labrocapsular lesions (97). Similar to the anterior labral tears, posterior labral tears present with absence, morphologic distortion, or contrast or fluid extending into the substance of the labrum. Posterior labral tears that are greater than 15 mm in length are significantly associated with posterior instability (98). Although some of the tears may not be classifiable, there are certain types that are as outlined subsequently.
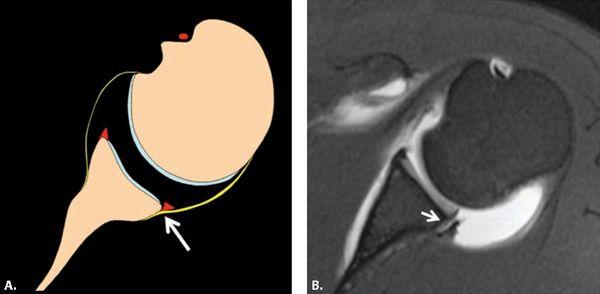
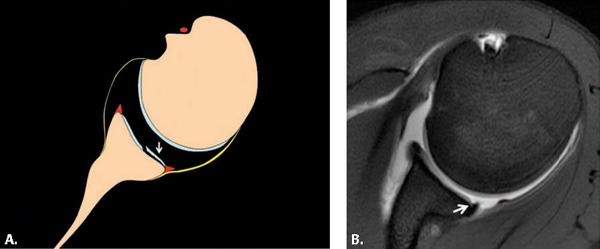
A particular type of posterior labral tear is the posterior labrocapsular periosteal sleeve avulsion injury termed the POLPSA lesion (99, 100) (Fig. 5.51). This lesion is an avulsion of the attachment of the posterior capsule and the periosteum, resulting in a patulous recess posteriorly. It is similar to a posterior Perthes or ALPSA lesion depending on whether it is medially displaced, which if present, would be the ALPSA lesion. POLPSA lesions are seen in association with posterior dislocation or subluxation of the glenohumeral joint and may predispose to recurrent instability. The surgical technique for repairing the POLPSA lesion differs from the reverse Bankart lesion, because the periosteal sleeve must be reduced to reattach the labrum.
FIGURE 5.42 Anterior ligamentous periosteal sleeve avulsion (ALIPSA) lesions. A–B: Two examples of ALIPSA lesions with stripping of the anterior band of the inferior glenohumeral ligament at the glenoid attachment (arrows) on fat-suppressed axial T1-weighted images from MR arthrograms.
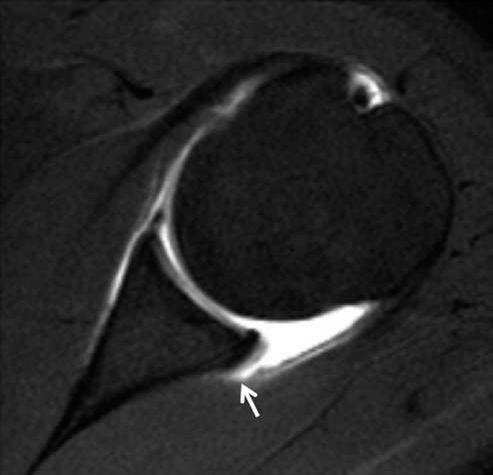
The reverse Bankart lesion and variants are similar to the anterior–inferior labral lesions described previously. These posterior–inferior labral tears are detached from the scapular periosteum without adjacent cartilage damage (101–103) (Fig. 5.52). In these cases, fluid or contrast may extend behind the glenoid posterior to the scapular neck.
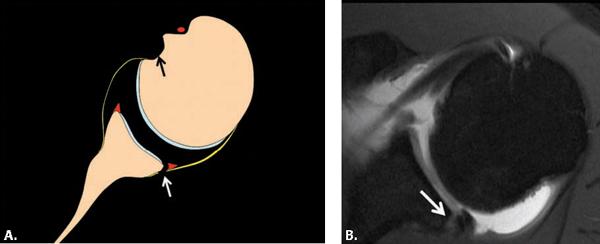
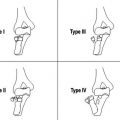
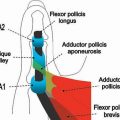
Another lesion of the posterior–inferior labrum is the deep/intrasubstance incomplete detachment that is associated with a defect at the chondrolabral junction. This is termed Kim’s lesion (104) (Fig. 5.53). Kim’s triad includes a marginal crack or chondral erosion, incomplete and concealed avulsion of the posterior inferior labrum, and chondrolabral retroversion (105). There are four types of posterior labral lesions described by Kim. These lesions are produced by a submaximal posterior force of the labrum at the attachment of the posterior band of the IGHL. The labral tears are seen at the posterior–inferior portion, causing detachment of the inner portion without involving the chondrolabral junction. With repetitive posterior subluxation of the humeral head, a shear force on the chondrolabral junction causes a marginal crack. With increased force, the tear along the inner portion can propagate to the surface of the chondrolabral junction and become visible at that location on arthroscopy. The concealed Kim’s lesion can be probed at arthroscopy and, if found, converted to a complete tear and repaired with a suture anchor. This restores the posterior labral height, preventing further posterior instability. Posterior capsular shift toward the superior direction is also performed at the same time. Some patients with Kim’s lesions have additional inferior capsular shift anterior–superiorly and closure of the rotator interval to address multidirectional instability if present.
FIGURE 5.43 Glenoid avulsion of the glenohumeral ligament (GAGL) lesion. This diagram shows avulsion of the anterior band of the inferior glenohumeral ligament with an intact labrum (arrow).
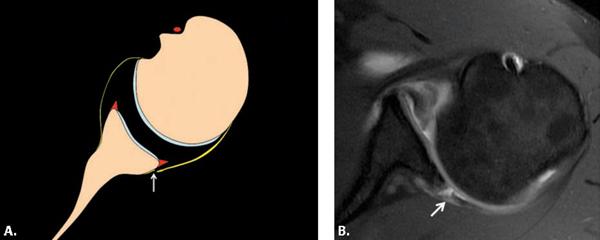
A posterior GLAD lesion involves the posterior inferior glenoid (Fig. 5.54) (106). Focal defects are seen in the articular cartilage between the 7 o’clock and 9 o’clock positions associated with a tear of the labrum. Impaction of an internally rotated humerus on the posterior–inferior glenoid is the suspected etiology for the posterior GLAD lesion.
It is also common to see extensive posterior labral tears associated with tears of other portions of the labrum. This includes types VIII and IX SLAP tears that involve the superior labrum and almost the entire labrum, respectively.
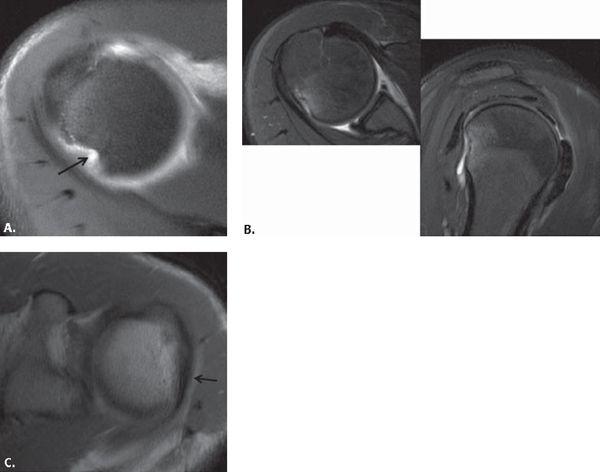
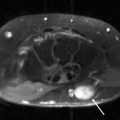
FIGURE 5.44 Hill Sachs lesions. A: An axial fat-suppressed T1-weighted image from an MR arthrogram obtained at the top of the humeral head reveals a wedge-shaped defect (arrow) consistent with a compression fracture from anterior dislocation. B: A smaller defect from an acute anterior dislocation with reactive marrow change is seen in axial and sagittal planes on a fat-suppressed T2-weighted image. C: The Hill Sachs lesion presents with flattening of the lateral humeral head (arrow) on this axial intermediate-weighted image.
Glenohumeral Ligament and Capsular Lesions Associated With Posterior Instability
Posterior capsular laxity is the most common abnormality seen with posterior glenohumeral instability (107) (Fig. 5.55). Methods can be used to calculate the capsular cross-sectional area on MR arthrography as shown recently by Dewing (108). In that study, the posterior capsule was the largest with multidirectional instability and showed an increased area as well with posterior instability. In addition, one may see a reverse GAGL lesion, which is an avulsion of the capsule and synovium at the posterior inferior glenoid rim (103) (Fig. 5.56).
The Bennett lesion is an extracapsular avulsive injury commonly seen along the posterior glenoid rim in 25% of throwing athletes such as baseball pitchers (109). This lesion is characterized by heterotopic ossification near the insertion of the posterior band of the IGHL on the glenoid produced by traction of the inferior glenohumeral ligament during the cocking or follow-through phases of pitching (110, 111) (Fig. 5.57). Although it can be asymptomatic, the Bennett lesion is sometimes associated with posterior labral injury and posterior under-surface tears of the rotator cuff (see the internal impingement and microinstability section of this Chapter). The patient may develop crescentic mineralization adjacent to the posterior–inferior osseous glenoid and sclerosis of the posterior glenoid. The mineralization may occasionally be identified on MRI but is better seen on axillary radiographs and CT. The Bennett lesion is usually low signal intensity or may contain fatty marrow and appear high signal intensity on T1-weighted and non-fat-suppressed images. Occasionally, there may be T2 hyperintensity in the region of the Bennett lesion, which suggests a more acute lesion. If symptoms are not relieved with lidocaine and steroid injections, Bennett lesions can be arthroscopically debrided. One study suggests that the asymptomatic Bennett lesion can be associated with posterior capsular thickening and internal rotation deficit also called glenoid internal rotation deficit disorder (GIRD) discussed in the next section (112). Those authors differentiated the asymptomatic Bennett lesion associated with GIRD from the symptomatic one by observing that painful Bennett lesions were more often associated with excessive motion of the humeral head resulting from posterior laxity at the follow-through phase of throwing.
At the other end of the posterior capsule, where it attaches to the humeral neck, the reverse HAGL (RHAGL) lesion, also called the posterior band inferior glenohumeral ligament avulsion from the humerus lesion, can be seen (113, 114) (Fig. 5.58). This injury has multiple etiologies. One mechanism of injury is a posteriorly directed force on an abducted shoulder and is often associated with posterior labral tears and cystic changes in the greater tuberosity. The RHAGL may also be related to multidirectional and microinstability and is characterized by a lack of attachment of the posterior band of the IGHL on the humerus with extravasation of fluid or contrast into the posterior soft tissues. The RHAGL lesion is important to identify on MRI preoperatively because it can be missed at arthroscopy if no anterior portals are used to look posteriorly (115–117). Also, one may want to do open repair rather than arthroscopic repair to prevent fluid introduced during arthroscopy from leaking out of the back of the shoulder through the capsular rent. Rarely, there can be an osseous avulsion of the posterior band of the inferior glenohumeral ligament from the humeral head, termed the reverse or posterior BHAGL lesion (Fig. 5.59). A floating posterior–inferior glenohumeral ligament with a tear at both ends can also be seen (72, 118).
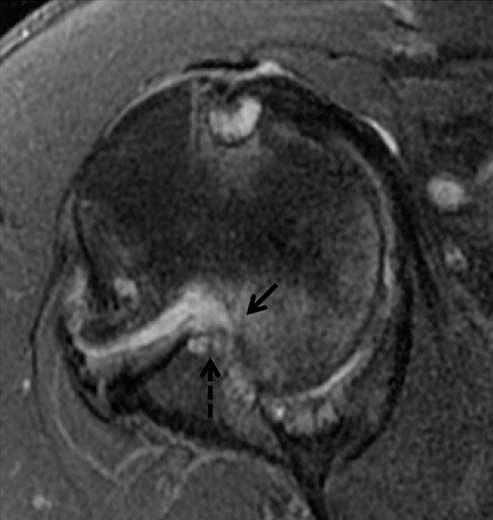
FIGURE 5.45 Engaged Hill Sachs lesion with bony Bankart. The wedge-shaped Hill Sachs lesion (solid arrow) is locked on the deficient anterior inferior rim of the glenoid (dashed arrow) on this axial fat-suppressed T2-weighted image.
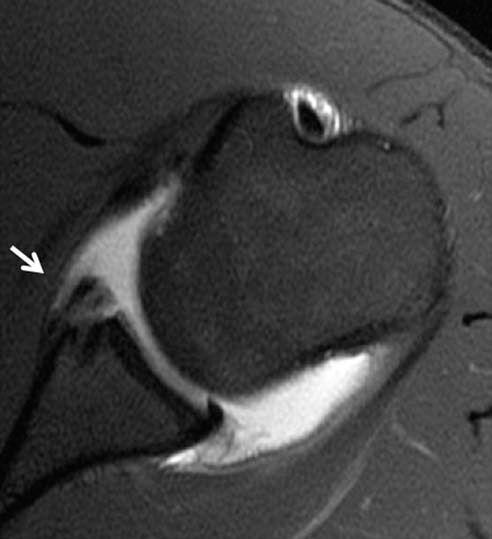
FIGURE 5.46 Osseous Bankart lesion. There is a fracture along the anterior glenoid rim related to prior anterior dislocation consistent with an osseous Bankart lesion on this axial fat-suppressed T1-weighted MR arthrographic image (arrow).
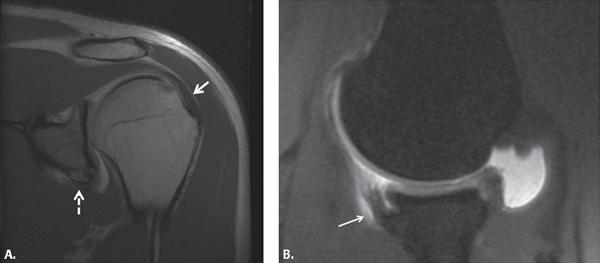
FIGURE 5.47 Old Bony Bankart and Hill Sachs lesion (solid arrow) on (A) coronal T1-weighted and (B) abduction and external rotation fat-suppressed T1-weighted images obtained during MR arthrography. Note the large, irregular fragment reattached to the glenoid (dashed arrow).
FIGURE 5.48 Inverted pear glenoid created by acute or chronic fracture and wear on the anterior glenoid from anterior instability. A: Sagittal diagram of acute fracture and (B) resorption of the anterior inferior glenoid. C: Sagittal T1-weighted image through the glenoid (arrows) demonstrates the loss of the anterior glenoid rim.
Lesions of the rotator interval have also been implicated in posterior and inferior instability of the glenohumeral joint. Stretching or interruption of the capsule of the rotator interval produces increased anterior translation of the humeral head at 60 degrees of flexion. Damage to this region is most commonly associated with enlargement or tearing from a shoulder dislocation; however, some individuals with abnormalities in the rotator interval do not have glenohumeral instability (119).
Osseous Lesions Associated With Posterior Instability
Some of the osseous lesions associated with posterior instability carry the familiar eponyms associated with anterior instability except that the word “reverse” is added to them. A reverse osseous Bankart lesion refers to an impaction fracture of the posterior glenoid resulting from posterior dislocation of the humerus (Fig. 5.60). The reverse Bankart is usually seen after trauma but occasionally with atraumatic posterior or multidirectional instability (107). The reverse osseous glenoid rim fracture was seen in 31% of cases of acute traumatic posterior dislocation in a recent study (97). A reverse Hill Sachs lesion results from an impaction fracture of the anterior medial humeral head, which involves 10% to 30% of the articular surface of the anterior humeral head (Fig. 5.50). Also referred to as a trough or McLaughlin’s fracture, it is seen in up to 86% of cases of acute traumatic posterior dislocation of the shoulder (97). The reverse Hill Sachs lesion is diagnosed when there is loss of the normal convexity of the anteromedial aspect of the humeral head (Fig. 5.61). The defect can be classified as small, medium, or large. A small defect is diagnosed when less than 25% of the articular surface of the humeral head is involved. A medium defect involves between 25% and 50% of the articular surface. A large defect occupies more than 50% of the articular surface (120). A reverse Hill Sachs defect can engage or lock on the posterior glenoid during internal rotation (99) producing posterior subluxation, attrition of the humerus, and a posterior labral tear. Avulsion of the lesser tuberosity may also occur with posterior instability.
FIGURE 5.49 Osteochondral lesion posterior inferior glenoid. Subchondral cysts (arrow) are seen in the glenoid on this sagittal fat-suppressed T2-weighted image from an MR arthrogram.
FIGURE 5.50 Posteriorly dislocated shoulder with trough line sign representing a reverse Hill Sachs lesion (arrow).
The posterior glenoid usually has a pointed posterior margin. Osseous anomalies that affect the posterior glenoid can produce multidirectional and posterior instability. These range from milder posterior glenoid rim deficiency to the denticulate glenoid. Posterior labral tears are common with these alterations in the normal glenoid configuration (121, 122).
A blunted posterior glenoid margin, termed posterior glenoid rim deficiency, is seen in 18% to 25% of individuals. The glenoid shape can be rounded in the configuration of a “lazy J” or triangular in the form of a “delta” (Fig. 5.62). Hyperplasia of the overlying labrum and/or cartilage may compensate for the deficiency, but in some, the deficient posterior glenoid predisposes to or is the result of posterior subluxation (112, 123). A denticulate glenoid is a scapular anomaly that involves hypoplasia of its neck, resulting in a broadened, shallow, and deformed lateral margin of the bone at the glenoid (Fig. 5.63). Bilateral and symmetric glenoid hypoplasia results in incomplete ossification of the lower two thirds of the bony glenoid and scapular neck with a smooth articular surface of the glenoid. Pronounced retroversion is visible. The overlying cartilage and labrum is frequently hypertrophied admixed with fat (122).
FIGURE 5.51 Posterior labrocapsular periosteal sleeve avulsion (POLPSA) lesion. A: Diagram and (B) fat-suppressed axial T1-weighted MR arthrographic image show an avulsion of the posterior labrum with a patulous posterior recess (arrow). The labrum is still attached to scapular periosteum.
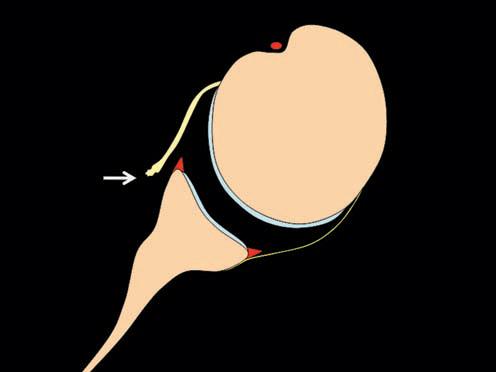
FIGURE 5.52 Posterior (reverse) Bankart lesion. A: Diagram and (B) axial fat-suppressed T1-weighted image from an MR arthrogram shows detachment of the posterior labrum from the glenoid rim with a disrupted scapular periosteal attachment (white arrow). The anterior concavity in the lesser tuberosity seen on this (black arrow) and subsequent diagrams of posterior instability represents a reverse Hill Sachs lesion, which can be seen with posterior instability but is not always seen in association with posterior labrocapsular abnormalities.
The glenoid cavity is normally in 5 to 7 degrees of retroversion relative to the mediolateral axis of the scapula (123) (Fig. 5.7). Increased retroversion has been demonstrated in patients with atraumatic shoulder instability (mean angle, 9.8° 5.9°) (123, 124). Increased retroversion produces loss of containment of the humeral head and may predispose to or be the consequence of posterior subluxation. The retroverted glenoid can be corrected by capsulolabroplasty (105).
Multidirectional Instability
Multidirectional instability represents an atraumatic form of instability that occurs in multiple directions resulting from capsuloligamentous laxity. Many people have joint laxity. A few of these patients have more severe soft tissue connective disorders such as Ehlers-Danlos syndrome. This is a functional instability that typically presents with chronic pain related to repetitive activities such as overhead throwing or swimming. The arm may “go dead” in the process. Sometimes the patient can voluntarily sublux their shoulder. Laxity tests on physical examination will demonstrate the problem.
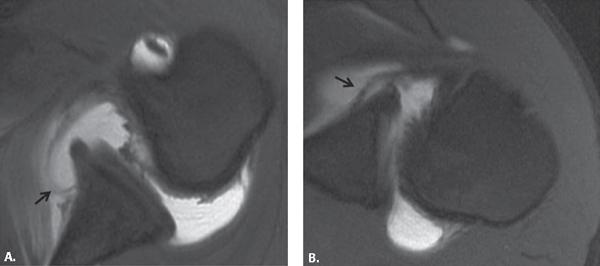
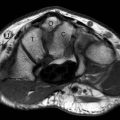
FIGURE 5.53 Kim lesion posterior labrum. A: Diagram and (B) axial fat-suppressed T1-weighted MR image from an MR arthrogram show a defect (marginal crack) at the base of the posterior labrum (arrow).
FIGURE 5.54 Posterior (reverse) glenolabral articular disruption (GLAD) lesion. A: Diagram and (B) axial fat-suppressed T1-weighted MR image shows a posterior glenoid labral tear with involvement of the underlying cartilage (arrow).
Some of the patients with this problem have findings related to instability that were discussed previously, but most just demonstrate a lax capsule, which is a subjective finding and difficult to quantify on MRI. These patients are treated conservatively with physical therapy. If that fails, an inferior capsular shift or arthroscopic plication can be performed.
FIGURE 5.55 Posterior capsular stripping. The capsule extends beyond the glenoid margin (arrow) on this axial fat-suppressed T1-weighted MR arthrographic image.
Additional Abnormalities Associated With Instability
Other abnormalities that can be seen with instability include subluxation or dislocation of the humeral head, fractures of the humeral head, rotator cuff pathology, perilabral cysts, and denervation.
Subluxation and Dislocation
In patients with anterior and posterior instability, there may be excessive anterior or posterior humeral translation, respectively. Multidirectional instability may show either direction. Subluxation or dislocation is well demonstrated on axial MR images. Humeral translation can be calculated on images obtained through the midglenoid level. A line is drawn connecting the anterior and posterior tips of the osseous glenoid fossa. A second, longer line is placed tangential to the ventral surface of the scapular body, bisecting the glenoid line and extending to the humeral head. A marker is also noted for the center of the humeral head. The distance between the tangential scapular line and the center of the humeral head represents the humeral translation distance. When the center of the humeral head is posterior to that line, there is negative humeral translation, resulting in posterior subluxation when the glenoid and humeral head are in contact and dislocation when they are not. When the center of the humeral head is anterior to the line, there is positive translation, resulting in anterior subluxation or dislocation. One study calculated a mean posterior humeral translation distance of −6.2 mm ± 0.8 mm in 12 patients with posterior instability (98). Another one showed a mean distance of −4.8 mm ± 0.75 mm with a range of −1 to −15 mm was significant in posterior instability patients (97). This was not influenced by the presence of intra-articular contrast material from an MR arthrogram. In our experience, provocative maneuvers such as the abduction external rotation positioning of the shoulder has the potential to bring out subtle subluxation that is not seen on routine MR imaging with the arm at the side (Fig. 5.64).
FIGURE 5.56 Posterior (reverse) glenoid avulsion of the glenohumeral ligament (GAGL) lesion. There is disruption of the glenoid attachment of the posterior capsule (arrow) on (A) a diagram and (B) axial fat-suppressed T1-weighted MR arthrographic image (arrows). Note the posterior glenohumeral subluxation in B.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree