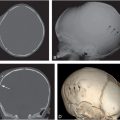
Figure 3.1 Soft tissue injury: early demonstration with scintigraphy. A, Anteroposterial (AP) view of the left femur in an abused infant with a swollen left thigh and a history of minor trauma. There is increased density and indistinct fat planes in the thigh. A classic metaphyseal lesion (CML) is noted distally (arrows). B, A posterior view of a bone scan taken four days later demonstrates marked soft tissue uptake in the proximal thigh. C, A follow-up view of the left femur 10 days later demonstrates extensive soft tissue ossification and subperiosteal new bone formation (SPNBF) surrounding the femoral shaft. (Courtesy of Andrew Schwartz MD.)
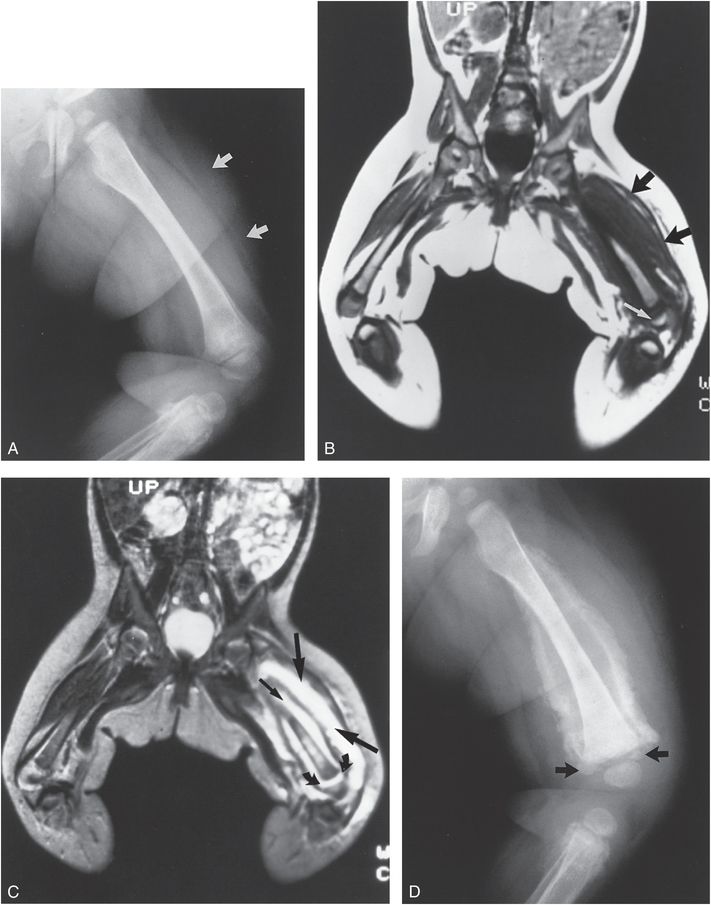
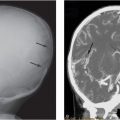
Figure 3.2 Soft tissue injury: early demonstration with MRI. A, Frog-lateral view of the left femur in an abused infant with a swollen thigh. Note the increased soft tissue density and indistinct fat planes in the thigh (arrows). B, T1WI of the lower extremities shows diffuse enlargement of soft tissues isointense with muscle (black arrows). Note the distal femoral epiphyseal separation (white arrow). C, T2WI demonstrates a high signal intensity corresponding to fluid within the muscle planes (large straight arrows), as well as fluid conforming to a subperiosteal location (small straight arrow). High intensity fluid extends from the subperiosteal region into the physeal fracture site (curved arrows). D, A follow-up view of the femur demonstrates massive subperiosteal new bone forming peripherally, sparing the more central regions. Ossification extends into the physeal fracture (arrows). A proximal tibial injury is also noted. (Courtesy of Nancy Genieser MD.)
Figure 3.3 Inflicted injury simulating tumor. AP view of the hips and pelvis in an eight-month-old abused infant reveals exuberant callus formation (white arrows) about the proximal shaft of the left femur. A biopsy of this lesion was interpreted as osteogenic sarcoma, but additional radiographs revealed other evidence of abuse. Careful assessment reveals widening of the physis (black arrow), indicating a physeal injury. (From Galleno H, Oppenheim WL. The battered child syndrome revisited. Clin Orthop. 1982;162:11–19.)
Swischuk described an unusual case of cortical irregularity, subperiosteal new bone formation (SPNBF), and myositis ossificans around the lesser trochanter in a two-year-old abused child with associated spinal cord injury (46). He believed that these findings were related to avulsion of the iliopsoas muscle insertion. Rarely, soft tissue foreign bodies such as sewing needles may be identified in an abused child (see Chapter 23) (47).
The proximal femur
Early reports suggested that the proximal femur is the most common location for inflicted femoral injury (14, 15). Later larger studies have shown that fractures of the proximal femur are much less common than those involving the mid and distal portions (23, 24, 37, 41, 42, 48, 49). This tendency is conspicuous in infants where classic metaphyseal lesions (CMLs) are common in the distal femur, but unusual proximally (50, 51).
Physeal injuries and epiphyseal separations
Of all long bone fractures due to child abuse, none is more likely to be associated with significant long-term orthopedic consequences than injury to the proximal femoral physis. The fracture is usually indistinguishable from that occurring as a result of obstetric injury (see Chapter 11), and for this reason, examination of this birth injury provides an understanding of the morphologic alterations and likely mechanisms at work with the abusive physeal fracture. Descriptions of this injury and its consequences predate the radiologic literature and have been the subject of many publications. In 1907, Elmslie delivered a lecture to the Royal College of Surgeons of England entitled “Injury and deformity of the epiphysis of the head of the femur (Coxa vara)”(52). He summarized the previous 18 years of discussions on the subject of coxa vara and indicated that birth trauma could result in physeal injury, with consequent decrease in the neck shaft angle.
By 1944, 21 cases of traumatic separation of the upper femoral epiphysis due to birth injury had been recorded. Kennedy pointed out that all but one fracture reported in the literature occurred during breech presentation and extraction, or version and breech extraction (53). There was frequent mention of a difficult or prolonged delivery and of the application of strong traction to the legs. Kennedy emphasized that because the proximal femoral epiphysis was not ossified at birth, the findings were often mistaken for a traumatic subluxation of the hip, a rare occurrence in infancy (53). Only with serial radiographs was it apparent that the ossification center of the femoral head was situated within the acetabulum, and that the fundamental alteration was a traumatic separation of the epiphysis from the metaphysis.
In 1969, Blockey emphasized that many cases of so-called congenital coxa vara were in fact secondary to trauma (54). His four cases clearly established the role of injury in the development of coxa vara, and he speculated about the role of child abuse in this lesion. Although many articles have illustrated proximal femoral epiphyseal separations with subsequent development of coxa vara, the potential confusion of this traumatic injury with a very uncommon congenital/developmental condition has not been emphasized (12, 14–16, 55–67).
Ogden and colleagues studied proximal femoral epiphyseal separations in six neonates, concluding that injuries related to delivery (five cases) and child abuse (two cases) were essentially identical (Fig. 3.4) (68). They also created neonatal epiphyseal separations in six stillborn human cadavers. The fracture was produced by sudden compression or traction applied to the distal femur until an audible snap was heard (Fig. 3.4A). Histologic examination usually revealed disruption of the hypertrophying cartilage cells as classically described in a Salter–Harris (SH) type I fracture (69). Interestingly, however, the fracture was noted to propagate into the primary spongiosa of the metaphysis in one case (Fig. 3.4B). In general, periosteal disruption occurred anteriorly but was maintained posteriorly, allowing the displaced metaphysis to “buttonhole” through the tear. Maintenance of the posterior attachment of the periosteum is critical for providing intrinsic stability to the fracture, minimizing the amount of residual deformity.
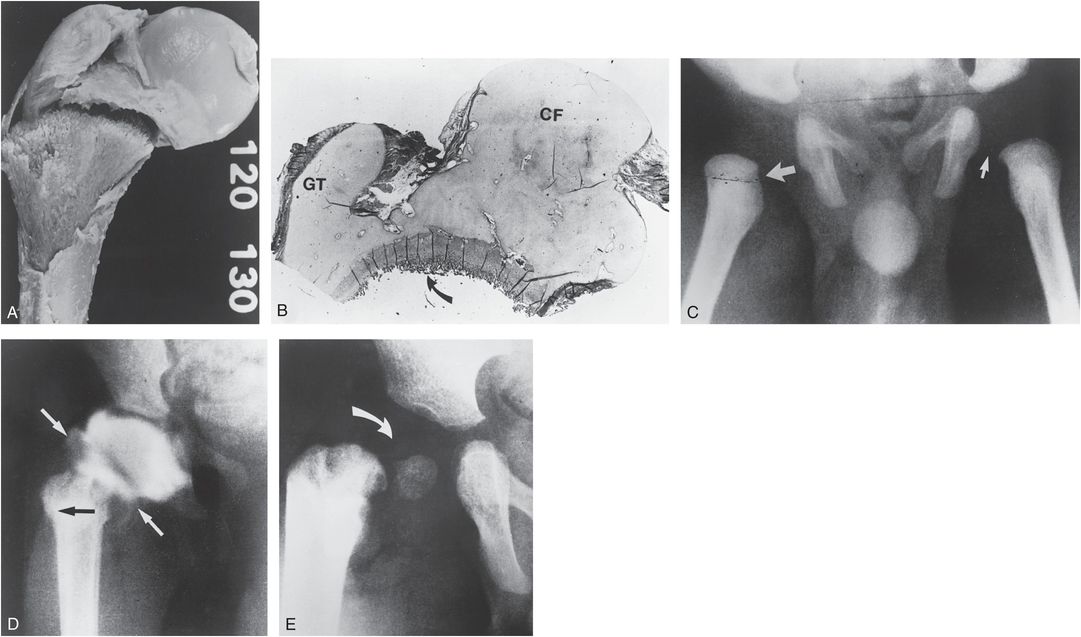
Figure 3.4 A, Experimentally produced proximal femoral physeal fracture in a stillborn human. A transverse fracture has occurred across the entire physeal–metaphyseal interface. The cartilaginous femoral head and greater trochanter (GT) have migrated medially with respect to the neck, resulting in a varus deformity. B, Histologic section reveals a fracture fragment that encompasses the capital femur (CF) and GT. Although the plane of the fracture is somewhat variable, its principal disruption is at the COJ (arrow). C, AP view of the hips in a five-week-old abused infant. There is lateral displacement of the right femoral neck (large arrow) compared with the normal left side (small arrow). The normal acetabular development argues against developmental dysplasia of the hip (DDH). D, Right hip arthrogram reveals a normally positioned femoral head. The metaphysis (black arrow) is laterally displaced secondary to a fracture through the physeal–metaphyseal junction. Note the confinement of contrast material within the joint, indicating maintenance of capsular attachments (white arrows). E, At eight months of age, coxa vara deformity is present (arrow). The femoral head is somewhat dysplastic but seated within the acetabular cavity. Despite valgus osteotomy, coxa vara persisted. (From Ogden JA, Lee KE, Rudicel SA, Pelker RR. Proximal femoral epiphysiolysis in the neonate. J Pediatr Orthop. 1984;4:285–92.)
Despite the rich literature on the subject of epiphyseal separations related to birth trauma, only modest attention has been given to the occurrence of proximal femoral physeal injuries in the context of abuse. Early examples are illustrated in Silverman’s classic 1953 article on “unrecognized skeletal trauma” where he stressed the need to differentiate the injury from hip dislocation (14). One of Silverman’s cases progressed to coxa vara. Jones et al. presented two cases and reviewed the subject of proximal femoral physeal injuries in the setting of abuse and stressed Silverman’s assertion that the injury could be confused with a hip dislocation (70). Although it is evident that proximal femoral epiphyseal separations are uncommon, they may not be as rare as the paucity of reports implies. When recognized as abusive fractures, these injuries tend to occur with multiple, often dramatic injuries elsewhere (see below).
Radiographically, a fracture of the unossified proximal femur can be diagnosed initially only if displacement of the femoral shaft with respect to the acetabulum has occurred. If the capital femoral epiphysis is unossified, differentiation between a fracture separation and developmental dysplasia of the hip (DDH) cannot be made with certainty (Fig. 3.4C). A normal-appearing acetabulum weighs against DDH. In the past, arthrography was performed in these cases, with contrast material defining a normally positioned, unossified femoral head (Fig. 3.4D). Sonography and MRI (see Fig. 3.6B) obviate the need for arthrography in most cases. Varying degrees of coxa vara can develop (Fig. 3.4E) and valgus osteotomy may be required.
When the femoral head is ossified and substantial displacement is present, the diagnosis is simplified. Typically, the femoral neck migrates laterally and proximally, with resultant varus deformity. Mild cases show only slight lateral displacement of the femoral shaft, which is best appreciated on a frog-lateral projection (Fig. 3.5). A useful sign for detecting minor differences in the position of the femoral heads with respect to the metaphyses can be created by drawing a line through the medullary cavities of the shafts of the femurs. These lines should intersect the femoral heads at identical sites. If there is asymmetry, the more medially displaced epiphysis with respect to the line indicates the side of injury (Fig. 3.5B). In more severe cases with greater epiphyseal ossification, the femoral head will be tilted and grossly displaced (Fig. 3.6A). MRI permits assessment of the unossified portions of the femoral head and acetabular cartilage (Fig. 3.6B).
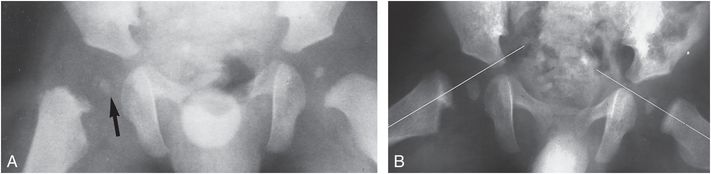
Figure 3.5 Proximal femoral physeal fracture. A, AP view of the hips in a young abused infant shows medial displacement of the femoral head with respect to the neck (arrow). Femoral heads are similar in size, and acetabular development is normal. B, A follow-up frog-lateral view demonstrates persistent displacement. A line drawn through the long axis of the femur intersects the femoral head on the left but not on the right.
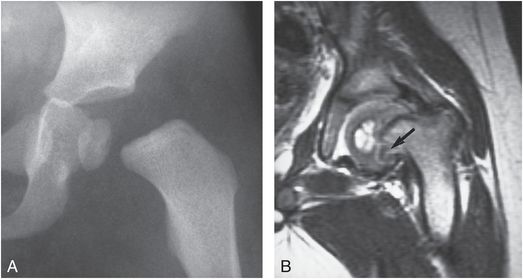
Figure 3.6 Proximal femoral epiphyseal separation. A, AP view of the hips in a 20-month-old abused child shows medial displacement and tilting of the left proximal femoral epiphysis. B, T2-weighted MRI, 2 months later shows varus deformity and remodeling of the femur. Note the persistent medial metaphyseal defect (arrow) with cartilage signal intensity. (Courtesy of Mike Thomason MD.)
With healing, the nature of the underlying anatomic alteration becomes apparent. This repair may display several patterns, depending on the degree of displacement, periosteal disruption, and the age of the patient. The extent of ossification of the femoral neck and head increases with patient age, and since the fracture occurs at the level of the physis, the site of injury will also vary with the patient’s age (Fig. 3.7). In infancy, the fracture occurs in the distal portion of the femoral neck. With healing, irregular ossification develops within the femoral neck, with associated varus deformity (Fig. 3.8).
Figure 3.7 Ossification pattern of the proximal femur. At birth (upper left) the femoral head, the greater trochanter (GT), and much of the femoral neck are composed of cartilage. The fracture at this age occurs through the lower portion of the femoral neck (arrows). With increasing age, the fracture is more proximally situated. In the older child (lower right) the fracture will occur in the subcapital region (arrows).
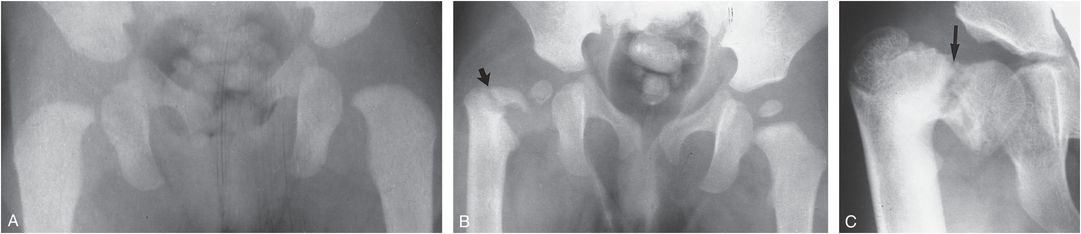
Figure 3.8 Post-traumatic coxa vara. A, AP view of the hips in a five-month-old infant shows normal femoral–acetabular relationships. B, AP view of the hips two years later after presumed abuse demonstrates right coxa vara deformity with a femoral neck fracture just above the GT (arrow). Sclerosis about the fracture site is evident and the femoral neck is dysplastic. C, At age seven years, the fracture line has healed, but there is severe coxa vara deformity. Sclerosis and irregularity are noted about the physis (arrow). (From Blockey NJ. Observations on infantile coxa vara. J Bone Joint Surg Br. 1969;51:106–11.)
When epiphyseal separation occurs in the older infant and child, the fracture will lie in the subcapital region. At the site of fracture, a persistent radiolucent line may be noted between the irregular new bone formation within the femoral neck and the more normal-appearing bone in the intertrochanteric region. This vertical lucency may persist for years, migrating distally with growth of the femoral neck, until bony union occurs (54). SPNBF may be minimal or absent, in which case the lesion may be erroneously considered congenital rather than traumatic. When exuberant callus formation occurs and typical displacements are present, the traumatic nature of this lesion is evident (Figs. 3.3, 3.9).
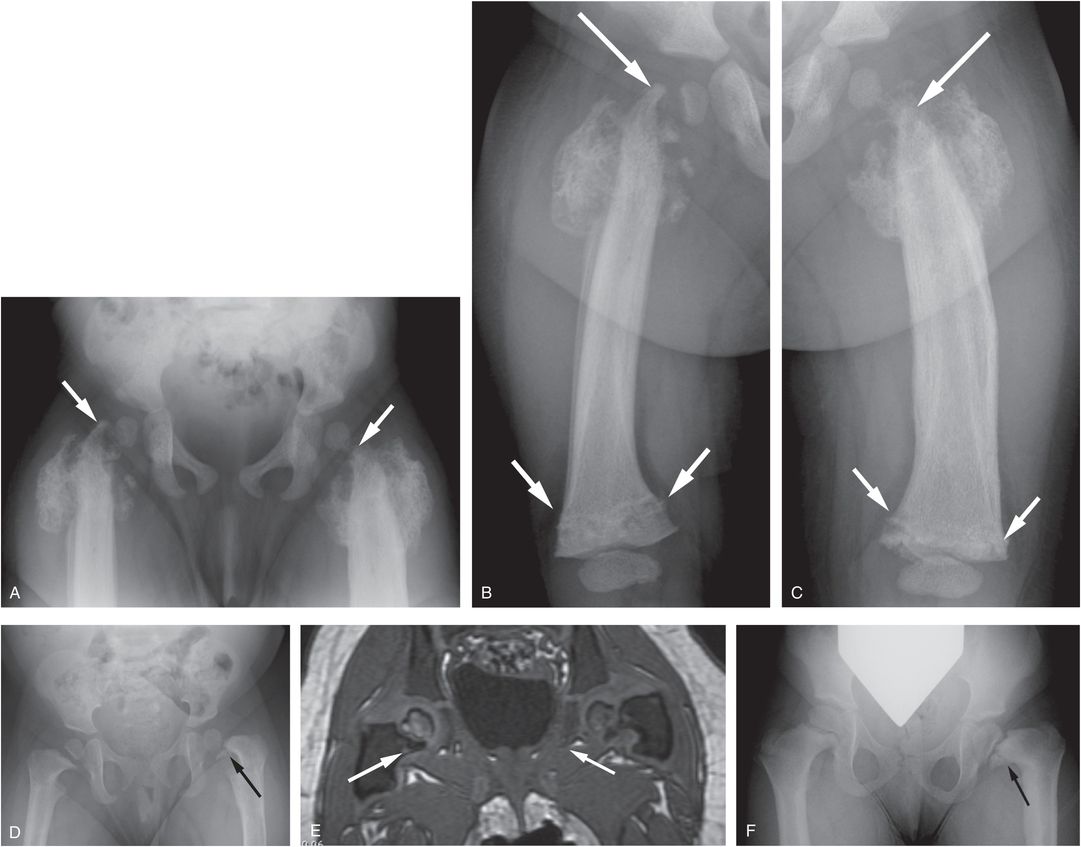
Figure 3.9 Bilateral proximal femoral epiphyseal separations. A seven-month-old infant with failure to thrive and unwillingness to bear weight. (See same patient in Figs. 3.52, 21.66.) The SS revealed numerous osseous injuries including CMLs, spine injury, and a skull fracture. AP view of the pelvis (A) and oblique views of both femurs (B, C) demonstrate bilateral epiphyseal separations with varus deformity, greater on the right. There is extensive callus/SPNBF. The femoral necks have a whittled appearance (large arrows), most evident in image C. Also note the bilateral healing distal femoral CMLs (small arrows). Follow-up radiograph at 14 months (D) shows progressive coxa vara deformity with modeling disturbance, particularly on the left. A persistent cleft is noted extending across the medial metaphysis on the left (arrow). E, Coronal gradient echo MRI at 30 months of age shows bilateral medial femoral neck clefts (arrows) with signal intensity similar to cartilage. F, AP radiograph at 3 years 9 months shows only mild residual coxa vara on the right, but persistent deformity and metaphyseal cleft on the left (arrow).
With repetitive injury and repair the femoral neck will be resorbed and remodeled with a whittled appearance (Fig. 3.9A–C). The ensuing growth disturbance may result in substantial shortening and/or bowing of the extremity. Bilateral involvement occurs, and despite the resultant coxa vara deformity, MR may show patency of the proximal femoral physis. However, a cleft of cartilaginous signal intensity can persist corresponding to the band of radiolucency in the medial metaphysis (Figs. 3.6, 3.9D–F). A similar metaphyseal cleft can be seen in the milder forms of metaphyseal dysplasia (see Chapter 7). Although avascular necrosis of the femoral head is a well-described complication of physeal injuries in older children, this has not been a notable finding with inflicted proximal femoral physeal injuries.
The CML
In contrast to the distal femur, the CML is rare in the proximal femur. In our study of 64 CMLs in 31 infant fatalities, no lesions were noted in the proximal femur (50). Overall, the proximal femur accounts for only about 2.5% of all CMLs encountered in living children (51). Clearly, the proximal femoral metaphysis is relatively resistant to this inflicted injury in infancy.
An early sign that suggests a CML is a radiolucent line within the metaphysis (Fig. 3.10). In the context of other indications of inflicted injury, this nonspecific finding may add further support to the diagnosis of abuse. If the lucency is unilateral, it is even more suggestive of injury. The CML may be manifest as a corner fracture along the medial aspect of the neck or a bucket handle pattern (Fig. 3.11). This variable appearance relates to projection, the extent and age of injury. This is well demonstrated in Fig. 3.12, where a variety of patterns are displayed depending on the radiographic projection and the plane of the computed tomography (CT) reformats.

Figure 3.10 Proximal femoral metaphyseal lucency in a five-month-old abused infant. Unilateral subphyseal metaphyseal lucency is noted on the right (arrow). Although a nonspecific finding, the unilaterality raises suspicion of a CML. Multiple CMLs and rib fractures were noted on SS.
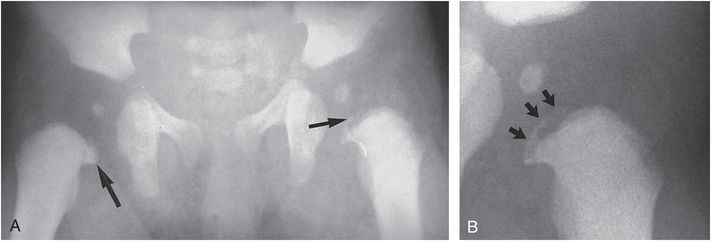
Figure 3.11 Proximal femoral CML. A, AP view of the hips in a three-month-old abused infant demonstrates bilateral CMLs. On the right there is a corner fracture pattern (large arrow). On the left there is a bucket handle fracture pattern (small arrow). B, Coned-down view of the left hip shows the bucket handle pattern to advantage (arrows). This infant died of inflicted head injury. (Courtesy of Mike Thomason MD.)
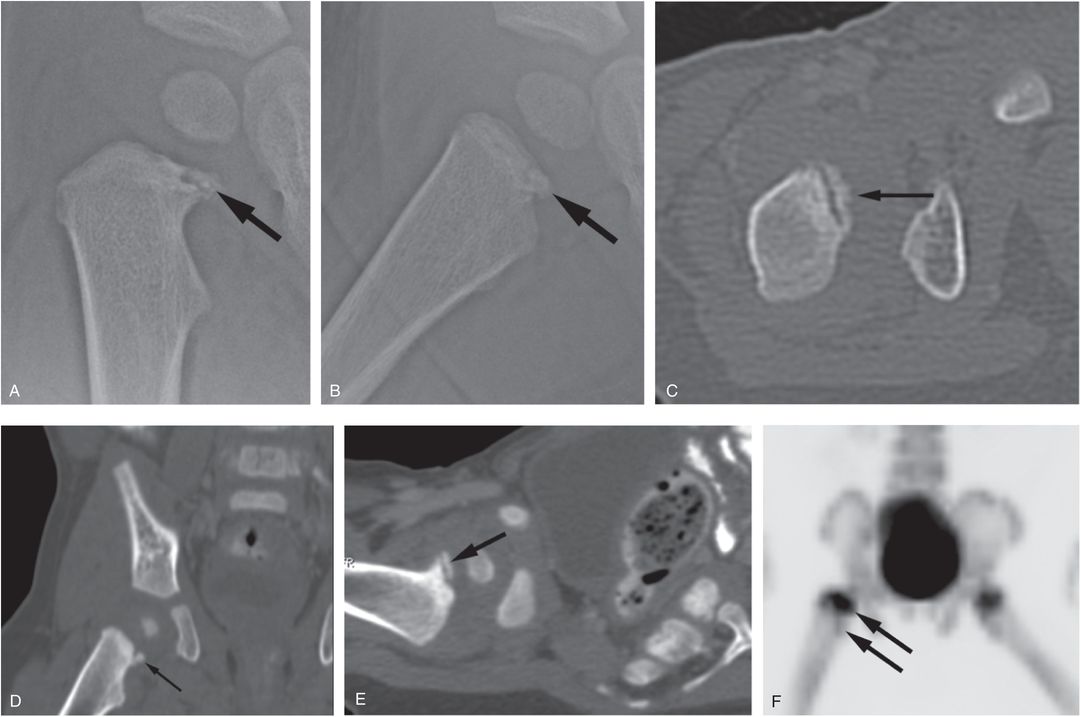
Figure 3.12 Proximal femoral CML. An eight-month-old infant with unexplained facial bruising and elevated liver transaminases. Abdominal CT revealed a liver laceration (see same patient in Fig. 5.44), and the SS showed multiple CMLs and rib fractures. AP (A) and frog-lateral (B) views of the right hip demonstrate a CML involving the anteromedial aspect of the proximal femur (arrows). Axial image of the right hip (C) from the abdominal CT with coronal (D) and axial oblique (E) reformats display the fracture fragment in a variety of patterns (arrows). F, Anterior maximum intensity projection (MIP) 18F-NaF PET image of the pelvis shows increased tracer uptake in the right proximal femoral epiphysis and metaphysis (arrows) as compared with the left side.
Scintigraphy tends to be relatively insensitive to CMLs, but bone scans done with 18F-NaF positron emission tomography (PET) show promise of greater sensitivity in the detection of CMLs, as noted in Fig. 3.12E (44). As with CMLs at other sites, the injury may not be visible initially and a follow-up radiograph will be required for documentation (Fig. 3.13).
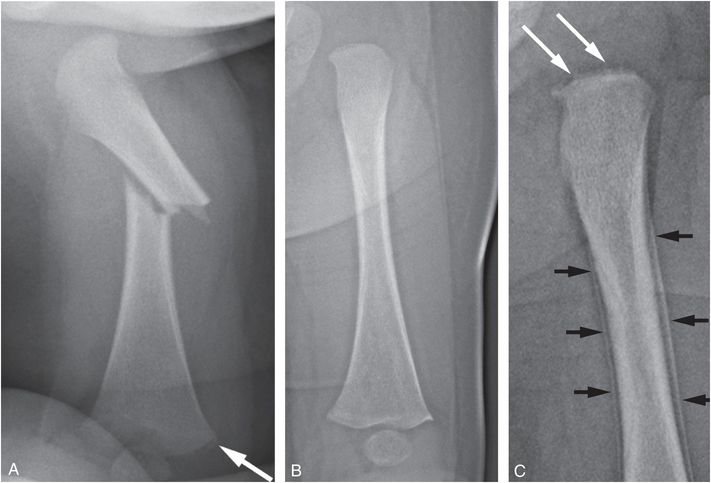
Figure 3.13 Follow-up radiograph documents injury not visible initially. A two-month-old infant brought to outside ER after parent reportedly sat on the infant and heard a “pop.” The infant began to cry with apparent pain in the right leg. Facial bruising was noted on physical exam. A, AP radiograph of the right femur on admission demonstrates an oblique fracture of the mid diaphysis and a CML of the distal metaphysis (arrow). B, Initial AP view of the left femur is normal. C, AP view of the proximal left femur two weeks later shows a bucket handle fracture pattern (large white arrows) as well as SPNBF along the proximal femoral shaft (small black arrows). A proximal humeral CML was also present.
It should be evident from the preceding discussion that it may be impossible to distinguish an acute CML from an epiphyseal separation, particularly if the femoral head is not yet ossified or if there is minimal epiphyseal displacement. It appears that there is a continuum between these two injury patterns. Such is the case with proximal humeral CMLs, where histologic material shows a tendency for the metaphyseal fracture line to meander into the physis (see Chapter 4). It is likely that more modest proximal femoral injuries are restricted to the metaphysis, healing quickly without out deformity; more severe forces result in a SH injury, which can lead to a physeal growth disturbance and coxa vara deformity. It is clear that the proximal femur is an uncommon site for CMLs, but when present, these fractures are usually associated with other skeletal injuries, reinforcing the requirement for thorough global skeletal assessment in such cases.
Femoral neck and trochanteric regions
As is the case with accidental injuries, most inflicted fractures of the femoral shaft involve the middle and distal thirds (41, 42). Fractures of the femoral neck and trochanteric regions are typically seen in older children who are victims of high-energy accidental traumatic events, usually motor vehicle collisions (1, 35, 36, 49, 71). Thus, a fracture of the femoral neck, intertrochanteric or subtrochanteric region, in any normal child with a history of a minor fall should undergo careful scrutiny.
Fractures in the regions of the trochanters may be difficult to identify radiographically. The hips are usually flexed and externally rotated and the fracture line often courses at an obliquity to the radiographic projection (Fig. 3.14). Even when the hip is well positioned for a high-detail radiograph, the fracture may be subtle when acute (Fig. 3.15). Since these high-energy injuries are generally clinically evident, lesser fractures may be unrecognized unless a systematic assessment is carried out. Scintigraphy and whole-body MRI (WB-MRI) complement the radiographic SS in selected cases (Figs. 3.14, 3.15).

Figure 3.14 Intertrochanteric fracture and contralateral distal femoral SH type II injuries. A three-month-old infant transferred with widespread skeletal injuries, including long bone shaft fractures, CMLs, and rib fractures of varying ages. (Same patient shown in Fig. 4.26.) A, Frog-lateral view of the hips demonstrates a zone of trabecular irregularity extending across the intertrochanteric region (black arrows). There are subtle cortical disruptions along the margins of the femoral neck (white arrows). B, Lateral view of the femur in a harness shows a discrete fracture line extending across the intertrochanteric region (arrows). Four days later, coronal STIR whole body MRI (WB-MRI) (C) and dedicated coronal STIR image of the left femur (D) demonstrate an angulated and displaced intertrochanteric femur fracture (large arrows) with extensive surrounding soft tissue fluid signal extending to the knee (small arrows). E, Magnified view of the right leg region shown in C demonstrates abnormal fluid signal within the distal thigh (large arrows) and possible widening of the distal right femoral physis (small arrow). F, Corresponding lateral radiograph demonstrates a SH type II fracture of the distal right femur (arrows). G, AP radiograph of the right femur two weeks later shows extensive SPNBF cloaking the shaft extending to the distal physis (arrows). H, Frog-lateral view of the hips on the same day shows mature callus surrounding the left intertrochanteric fracture (arrows).
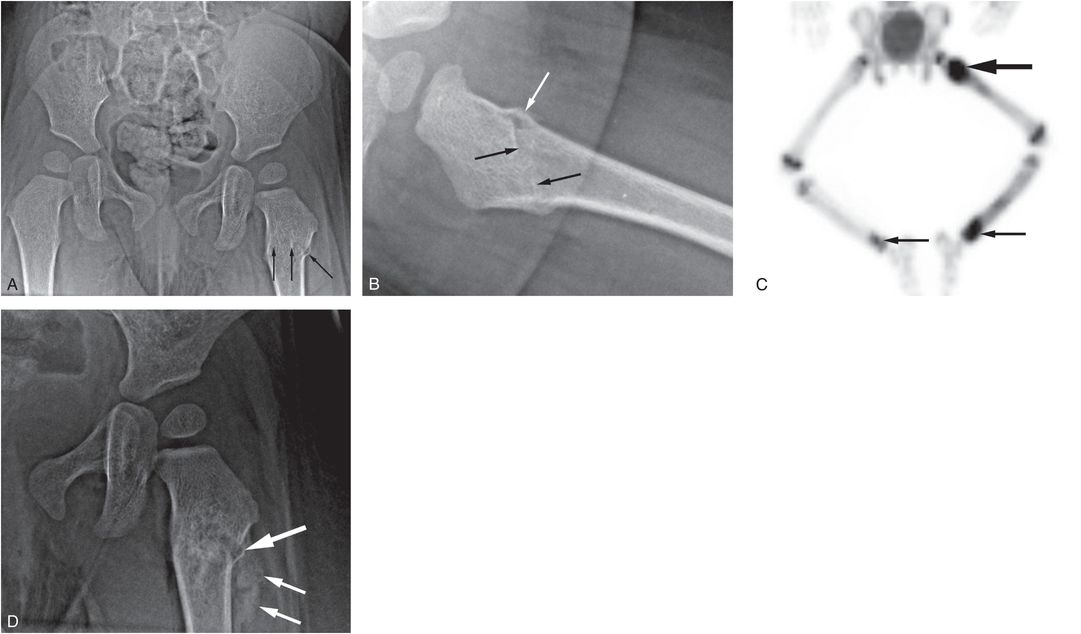
Figure 3.15 Intertrochanteric fracture. A one-year-old boy not moving his left arm and unwilling to stand the morning after he was allegedly thrown from the crib by a three-year-old child. SS showed multiple extremity, rib, clavicle, and skull fractures. A, AP view of the pelvis shows trabecular irregularity and cortical disruption in the left intertrochanteric region (arrows). B, Frog-lateral view shows disruption of the anterior cortex (white arrow) and an abnormal bone density projecting in the medullary cavity (black arrows) consistent with overlapping fracture margins. C, Anterior MIP 18F-NaF PET bone scan image demonstrates intense activity at the fracture site (large arrow), as well as other areas of increased tracer uptake (small arrows). D, AP view of the left hip two weeks later shows early callus/SPNBF (small arrows) and a small laterally situated comminuted fragment (large arrow). (Same patient is shown in Figs. 3.69, 4.19, 5.40, 17.13.)
Diaphysis
In contrast to proximal femoral epiphyseal separations and CMLs, which are characteristic of abuse, fractures of the femoral diaphysis are low-specificity injuries. Much has been made of the value of a spiral or oblique femoral fracture pattern as a strong predictor of abuse. This subject has been discussed in general in the preceding chapter, and with specific regard to the femur, the literature fails to confirm this concept (6, 20, 22, 25–27, 29, 31, 38, 41, 42, 48, 72–76). Rather than pointing to inflicted or accidental trauma, a spiral or oblique pattern implies application of a torsional force via the distal portion of the extremity (Fig. 3.16) (77).

Figure 3.16 Femoral spiral/oblique fracture. A, AP view of the left femur in a two-year-old abused child shows a spiral fracture pattern (arrows). B, Lateral view demonstrates an oblique fracture pattern. The pattern depends on radiographic projection.
Attempts to distinguish an oblique from a spiral fracture pattern can be futile because a fracture may show a spiral pattern in one view and an oblique pattern in another (Fig. 3.16). Transverse and mildly oblique shaft fractures can occur with direct blows, but in infancy, they more likely result from bending forces, as the leg is grabbed or forcefully manipulated or as the infant is swung, slammed, or thrown (see Fig. 3.13) (77). Angular deformity may be dramatic (Fig. 3.17). Despite impressive radiographic findings, scintigraphy may show no increased tracer activity acutely (Fig. 3.18; see same patient in Fig. 5.35).
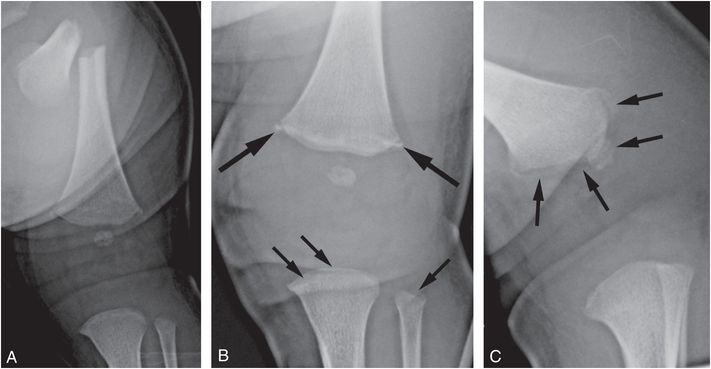
Figure 3.17 Severely angulated femoral shaft fracture. A three-week-old male infant transferred from an outside hospital (OSH) with a left femur fracture, bilateral subconjunctival hemorrhages, and multiple bruises on face, abdomen, and back. The mother heard crying and found infant with his left leg twisted between crib railings with noticeable deformity, prompting visit to OSH where radiographs revealed a fracture of the left femur. A, AP radiograph of the left femur reveals a severely angulated transverse mid-shaft fracture. Cone-down AP (B) and oblique (C) radiographs of the left knee demonstrate a CML with a corner facture pattern on the frontal projection and a bucket handle pattern on the oblique view (large arrows). Proximal tibial and fibular CMLs are also evident (small arrows in B). (See clavicular fracture in the same patient in Fig. 5.49.)
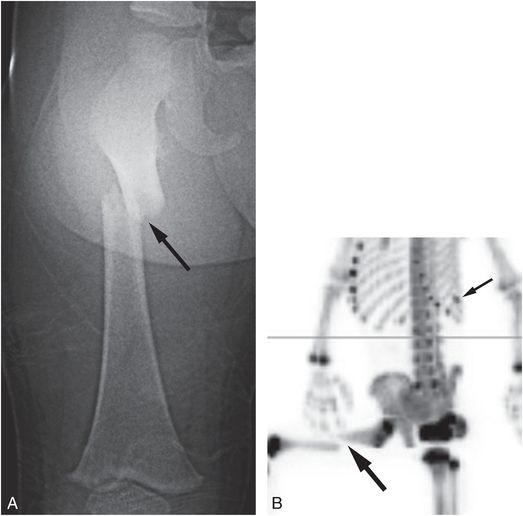
Figure 3.18 Acute transverse femoral shaft fracture without radiotracer uptake. A 20-month-old child with fussiness and right thigh swelling after an unwitnessed fall from a bed. (See same patient in Fig. 5.35.) There was facial bruising, elevated liver enzymes, and a solitary rib fracture. A, AP view of the right femur demonstrates a displaced angulated transverse fracture of the proximal diaphysis (arrow). B, Oblique MIP 18F-NaF PET image demonstrates discontinuity of the signal related to the fracture (large arrow), but no increased marginal tracer uptake. Note the solitary rib fracture (small arrow).
Comminuted fractures are unusual, and aside from implying greater or more complex forces than other shaft fracture patterns, they are nonspecific injuries (Fig. 3.19) (78). When there are multiple comminuted fracture components, an apparent intramedullary radiolucency at the fracture site may suggest a pathologic fracture through a lytic lesion, such as Langerhans cell histiocytosis. Follow-up imaging will resolve the issue. Although waiting until later out-of-cast imaging is possible, it may unduly delay a confident diagnosis. Initial advanced imaging can provide the assurance that the appearance relates to gross displacement of otherwise normal bony fragments, rather than an underlying destructive lesion (Fig. 3.19).
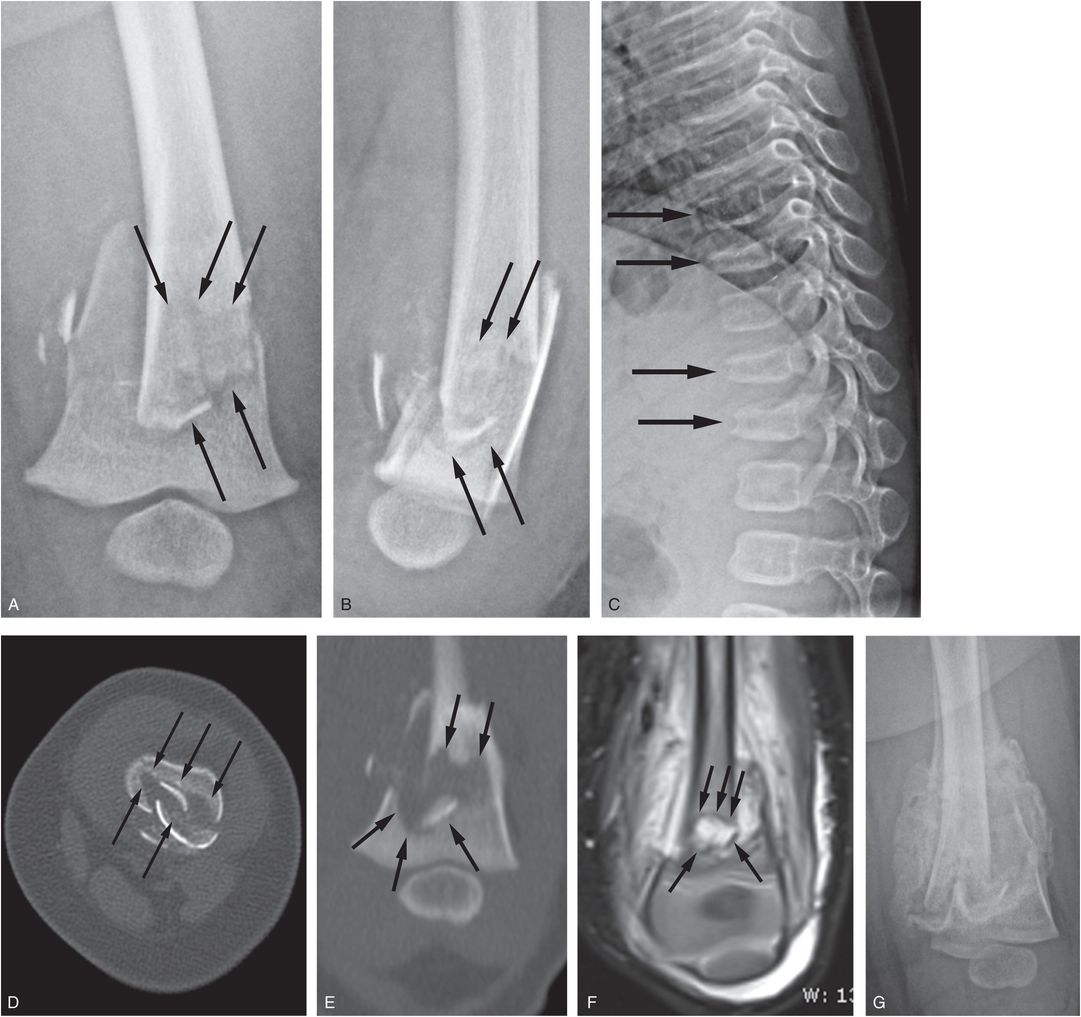
Figure 3.19 Comminuted femoral shaft fracture with features suggesting an underlying lytic lesion. A four-month-old infant with one day of fussiness and left thigh swelling without a history of trauma. Radiographs revealed a left femur fracture. AP (A) and lateral (B) views of the left femur from the SS reveal a displaced comminuted fracture of the distal femoral metadiaphysis. There is the suggestion of an underlying intramedullary lucency raising concerns of a pathologic fracture (arrows). C, Lateral view of the thoracic spine shows compression fractures of T8, T9, T11, and T12 (arrows). The SS was otherwise normal and the differential diagnosis rested between abusive trauma and an underlying neoplastic process, such as Langerhans cell histiocytosis. D, E, Axial and coronal reformats of the femoral CT show a geographically marginated intramedullary lucency (arrows), but it is not clear if this simply reflects the bony defects related to the displaced fracture fragments or a geographic zone of bone destruction from an underlying process. F, Coronal STIR MRI shows fluid signal within the fracture plane (arrows) with extensive soft tissue edema hemorrhage. There is relatively normal marrow signal surrounding the fracture site, making an underlying neoplastic process unlikely. The 18F-NaF PET study showed no evidence of a disseminated neoplasm, but did reveal an ischial avulsion fracture that was confirmed on the MRI and follow-up SS. (See same patient in Fig. 3.106.) G, Three weeks later, there is robust callus formation without signs of underlying lesion. (From Bixby SD, Wilson C, Barber I, Kleinman PK. Ischial apophyseal fracture in an abused infant. Pediatr Radiol. 2014;44(9):1175–8.)
Occasionally, femoral shaft injuries are manifest as subtle nondisplaced hairline fractures, similar to the “toddler’s” pattern common in the tibial shaft. The child may present with a limp and tenderness which is difficult to localize. Another uncommon injury is the cortical buckle or torus fracture, a lesion that tends to involve the thinner cortices of infants (Fig. 3.20).
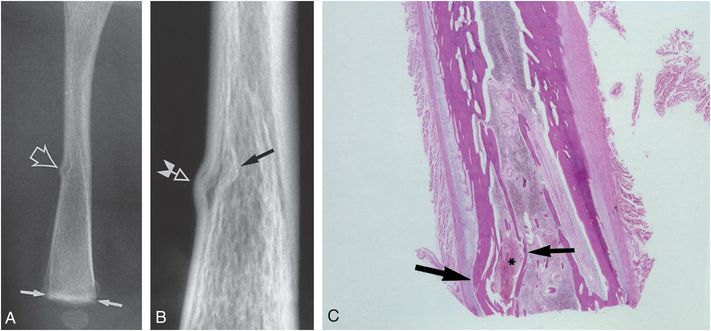
Figure 3.20 Buckle fracture of the femoral shaft. A, Lateral view of the right femur in a one-month-old fatally abused infant shows a buckle fracture of the anterior cortex (large arrow). A suggestion of a metaphyseal injury is present distally (small arrows). B, Specimen radiograph shows buckling of the cortex (white arrow) as well as the endosteal surface (black arrow). C, Corresponding photomicrograph demonstrates buckling of the cortex (large arrow), hemorrhage (*), and buckling of the endosteal surface (small arrow).
The subject of bilateral femoral shaft fractures associated with abuse has received little attention in the literature (Fig. 3.21) (41). Their presence implies greater or more complex forces than those entailed in customary household accidents. Regardless of radiologic pattern, bilaterality of femoral shaft fractures should heighten concerns of abuse in any young child with a history of a simple low-energy traumatic event. Bilateral femoral shaft fractures may be associated with florid injuries of the lower extremities, including CMLs (Fig. 3.22).

Figure 3.21 Bilateral femoral shaft fractures. A three-month-old infant transferred for bilateral femur fractures diagnosed at an OSH. The baby was reportedly co-sleeping in bed when the parent awoke and found the crying baby pinned on his back under the parent, with the infant’s legs behind its head. AP view of the pelvis and hips demonstrates bilateral oblique fractures of the proximal femoral shafts. The right-sided fracture extends to the femoral neck. There were multiple rib fractures and a distal tibial CML.
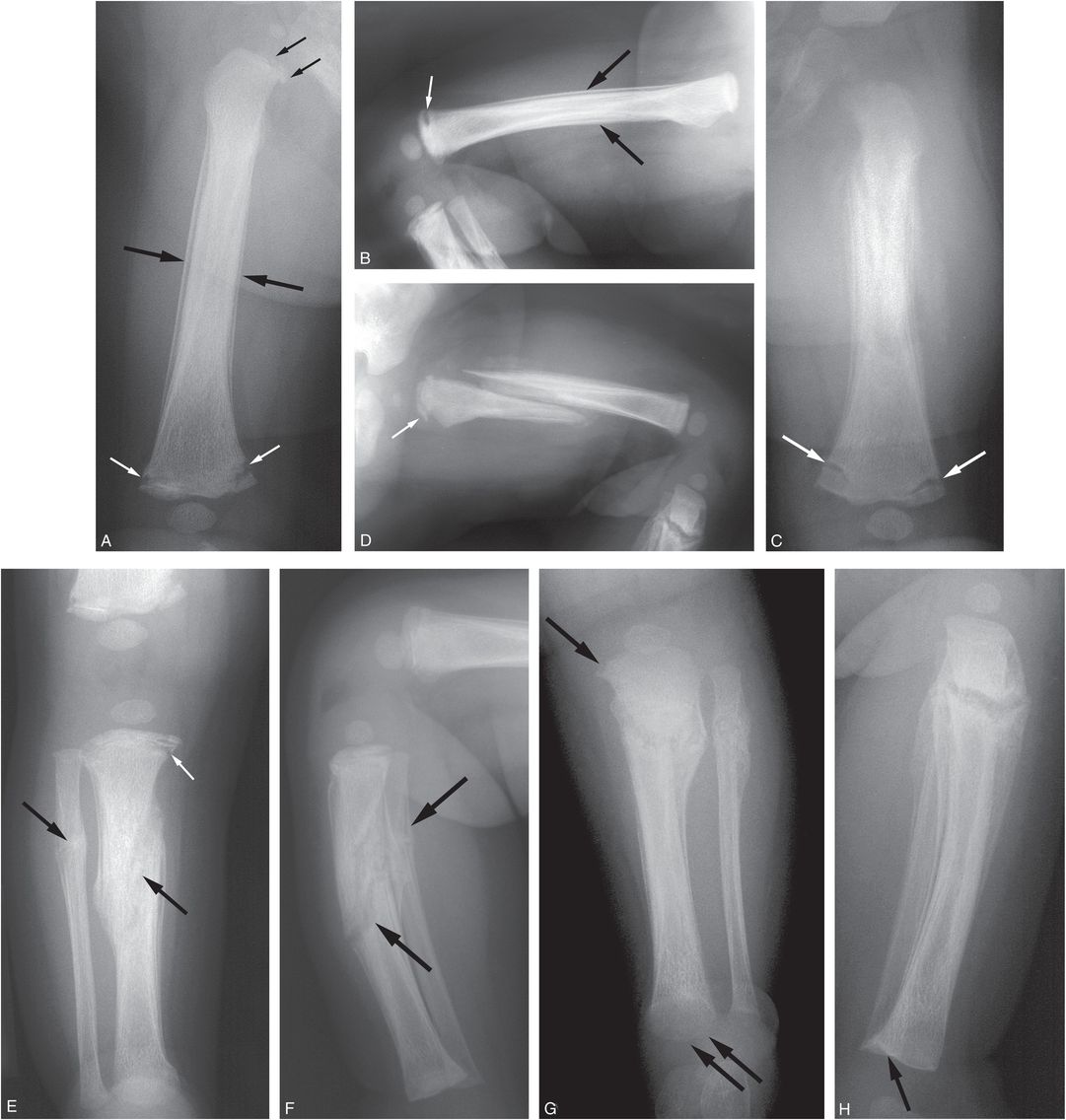
Figure 3.22 Bilateral femoral shaft fractures with florid lower extremity injuries. A four-month-old infant not moving left leg. Mother reported that boyfriend struck the leg several days earlier. The infant was transferred after multiple fractures were identified on SS done elsewhere. AP (A) and lateral (B) views of the right femur demonstrate SPNBF and medullary sclerosis centered at the mid diaphysis (large black arrows) consistent with a healing nondisplaced fracture. A discrete fracture line is not definitely seen. There is a healing CML in the distal femur (white arrows) and a more subtle CML proximally (small black arrows). AP (C) and lateral (D) radiographs of the left femur demonstrate a healing grossly displaced oblique proximal femoral shaft fracture. Again, a healing distal CML and less conspicuous proximal femoral CML are noted (arrows). AP (E) and lateral (F) views of the right lower leg show a healing oblique fracture of the mid tibial shaft and an adjacent healing fibular fracture (large arrows). There is a healing proximal tibial CML (small arrow). AP (G) and lateral (H) views of the left lower leg demonstrate a healing oblique fracture of the proximal tibial shaft as well as proximal and distal tibial CMLs (arrows). Note that the fracture line, of the right proximal tibial CML in part E is further from the physis than the CML on the left in part G implying that it is an older injury that has migrated further down the metaphysis with healing and tibial growth.
Patterns of healing shaft fractures are variable. When there is displacement/comminution and hemorrhage, there will be robust callus formation which can appear and evolve quickly in young infants (Fig. 3.19). This can be accentuated with continued injury due to lack of immobilization because of failure to seek attention (Fig. 3.22C,D). With nondisplaced fractures there may be only modest SPNBF that can obscure the underlying fracture line. Subtle intramedullary sclerosis may provide greater confidence of traumatic injury (Fig. 3.22A,B). Shaft fractures, if untreated, usually heal spontaneously with variable deformity. Malalignment of the fracture site may lead to angular deformity. As rotation is often present at the fracture site, a substantial torsional deformity may develop. If there is excessive overriding, a shortened extremity will develop. If there is no overriding, an actual increase in extremity length may ensue secondary to hyperemia and increased longitudinal growth at the physes.
In the young infant, symmetric SPNBF frequently occurs as a normal finding (see Chapter 12) and can be difficult to distinguish from a traumatic process. Occasionally, an acute fracture may occur through an area of pre-existing diffuse SPNBF. This pattern may be mistaken for a healing shaft fracture (Fig. 3.23) (79).
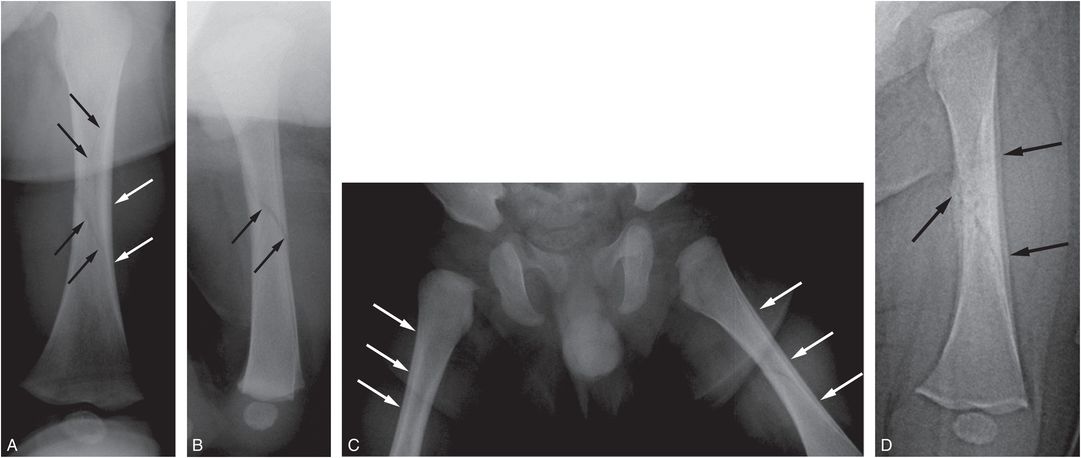
Figure 3.23 Acute fracture through physiologic SPNBF. A three-month-old infant transferred from an outside facility with a fractured femur. The parent pushed and tried to twist the leg to fit it into pajamas and felt a snap. AP (A) and lateral (B) radiographs of the left femur demonstrate a spiral fracture of the left femoral diaphysis (black arrows). There is smooth SPNBF along the femoral shaft (white arrows). C, AP view of the hips and proximal femurs shows symmetric SPNBF bilaterally (arrows). D, AP view of the left femur 17 days later shows callus formation along the medial aspect of the spiral fracture and conspicuous SPNBF laterally (arrows). The findings are most consistent with an acute fracture through physiologic SPNBF.
Despite the common occurrence of abusive femoral shaft fractures, these nonspecific injuries pose significant diagnostic challenges clinically and on imaging grounds. As discussed elsewhere global skeletal screening is appropriate with all unexplained femoral shaft fractures in otherwise normal nonambulatory children. Although this is usually accomplished with SS, scintigraphy plays a role in two situations. When there is a strong clinical concern for abuse, and the initial survey is normal, scintigraphy may provide critical early information that may have an immediate impact on child protection actions (Fig. 3.24). The other situation is more practical – when a femoral fracture in a toddler has been treated with Spica cast application before the remainder of the skeleton has been imaged. In such cases, a bone scan will be a reasonable substitute for a SS (see Fig. 3.15). This practice should be discouraged in infants because scintigraphy is insensitive to CMLs, and in appropriate cases, it may be prudent to remove the Spica cast in order to perform a SS. If the child has been put in a harness for a femoral fracture, this should be carefully removed and a SS should be performed.

Figure 3.24 Complementary roles of radiography and scintigraphy. A five-month-old infant with a swollen leg and facial bruising. Parent noted a snap during diaper change, followed by inconsolability. A, Initial frog-lateral view of the hips demonstrates an oblique fracture of the left proximal femoral diaphysis. A SS, including the AP view of the right femur (B) was otherwise normal. Because of strong concerns of abuse, a bone scan was performed. C, Posterior view of the 99mTc MDP bone scan shows a photopenic region (large arrow) conforming to the known left fracture femoral site. Additionally there is increased uptake in the distal right femoral shaft (small arrows). D, Lateral view of the right femur four days later demonstrates SPNBF along the anterior cortex (arrows), correlating with the finding on bone scan.
Lastly, femoral shaft fractures may be accompanied by CMLs, particularly distally, in which cases a low-specificity injury may take on more ominous implications. Initial femoral radiographs in children with acute femoral fractures tend to be limited technically, and failure to identify a CML accompanying a shaft injury can have major implications in subsequent diagnostic assessments and clinical management (Fig. 3.25).
Figure 3.25 Extremity injury. AP view of the femur of a five-month-old infant with a history of a short fall and of not moving the right leg. There is an acute oblique fracture through the middle one-third of the diaphysis. The fracture has occurred through an area of thick, mature, subperiosteal, and endosteal new bone (large arrows). A CML is present distally (small arrow). Widespread skeletal injuries and a SDH were subsequently identified in this infant and his asymptomatic twin brother.
The distal femur
The distal femur is a common site of injury with abuse, particularly in infancy. Studies that focus on patients with significant orthopedic problems tend to underestimate the number of these fractures, whereas studies including large numbers of infants undergoing thorough SS evaluation yield high percentages of distal femoral injuries (18, 24, 30, 31, 41, 50, 51).
Nonspecific metaphyseal fractures
Nonspecific fractures of the metadiaphysis and metaphysis should be differentiated from CMLs and SH physeal injuries (Fig. 3.26). (See Figs. 2.5, 2.11.) Arkader et al. suggested a strong association of complete fracture of the distal femoral metaphysis with abuse in nonambulatory children (80). Of 29 fractures with this pattern, 20 occurred in children 1 year old or younger (before walking age). The average age for the 14 boys and 6 girls was 6 months, 10 days (range: 5 days to 1 year). Ten cases (50%) were confirmed to be a result of child abuse, and another 5 cases (25%) were highly suspicious for abuse. Fifteen of the 20 children (75%) with complete distal femoral metaphyseal fractures were potentially victims of child abuse. On the other hand, Haney et al. have provided evidence that posteriorly angulated and impacted distal femoral metaphyseal fractures can occur in infants and toddlers from a short fall onto a flexed knee, but they emphasize that a systematic assessment is appropriate to exclude abuse (81).
These nonspecific distal femoral metaphyseal fractures can be significantly displaced or angulated (see Fig. 2.11) or may produce no gross deformity (see Fig. 2.5). The spectrum of these simple fractures blends with that of SH injuries and CMLs and careful inspection of what appears to be a nonspecific transverse metaphyseal fracture may in fact reveal a tiny metaphyseal fragment (Fig. 3.26).
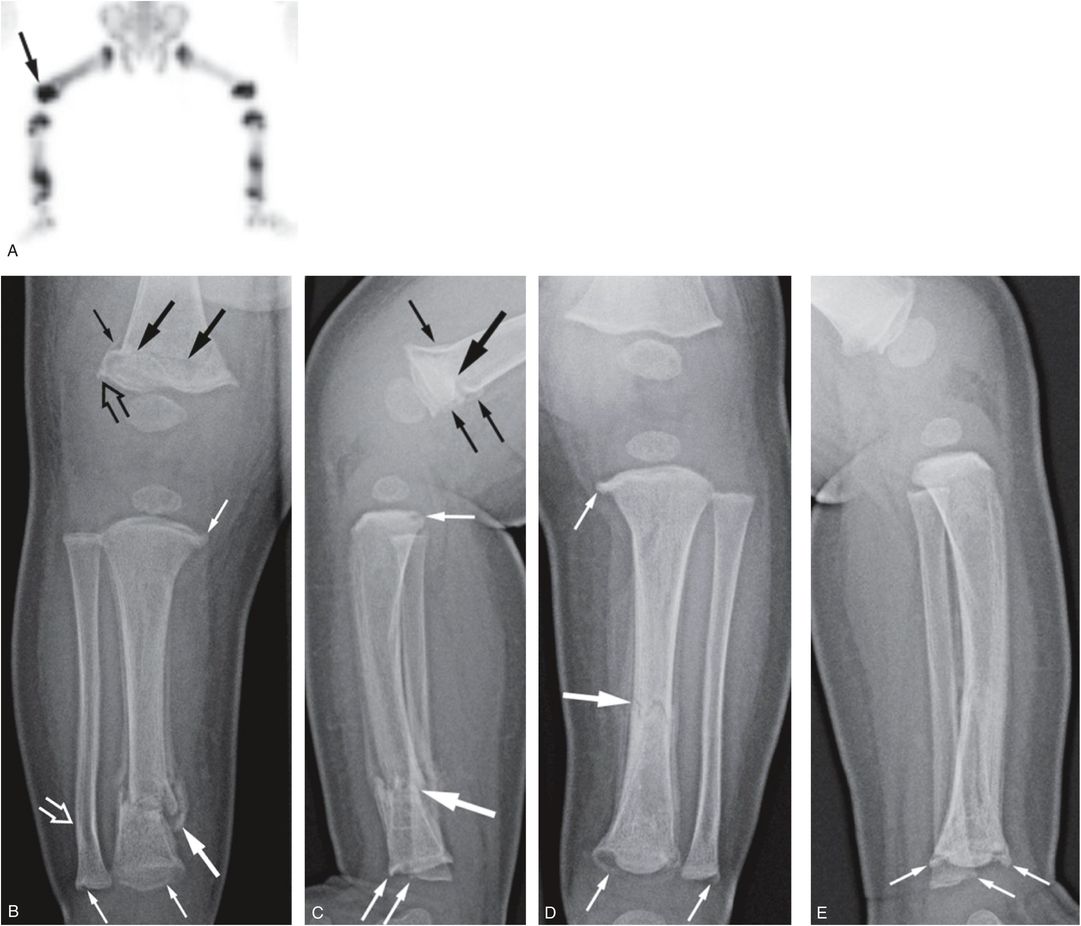
Figure 3.26 Nonspecific metaphyseal fractures. A three-month-old infant with fussiness and right leg swelling noted by pediatrician. A, Anterior MIP 18F-NaF PET image of the legs shows increased activity within the right distal femoral shaft (arrow) and metaphyseal–epiphyseal complex, as well as other foci of abnormal uptake in the lower legs. AP (B) and lateral (C) views of the right knee and lower leg demonstrate a roughly transverse anteriorly angulated fracture of the distal femoral metaphysis (large black arrows). There is early SPNBF (small black arrows). There is an associated subtle distal femoral metaphyseal irregularity suggesting a CML (open black arrow). In the lower leg, there are multiple CMLs involving the tibia and fibula (small white arrows) and a healing oblique distal tibial metadiaphyseal fracture (large white arrow). There is subtle lateral bowing deformity of the distal fibula (open white arrow). AP (D) and lateral (E) views of the left lower leg show a healing transverse midshaft tibial fracture (large arrow) and multiple CMLs of the tibia and fibula (small arrows). (See same patient in Fig. 4.47.)
The CML
The distal femur is one of the most common sites for the CML. Caffey emphasized the distal femoral location in his oration to the British Institute of Radiology in London in 1956, and a subsequent publication showed numerous examples of distal femoral metaphyseal injuries (56). Loder and Bookout found that 5 of 19 metaphyseal lesions involved the distal femur (74). Worlock and colleagues found that 5 of 17 metaphyseal lesions involved the distal femur (31). Kleinman and colleagues found that 15 of 64 CMLs (23%) in abused infant fatalities involved the distal femur (50, 82). The injuries were bilateral in four infants and unilateral in seven (five right, two left). They were commonly associated with ipsilateral CMLs of the proximal tibias. Barber et al. found that 52% (64/124) of the CMLs noted in 50 infants involved the distal femur (51).
Relevant normal anatomy
The normal flaring of long bone metaphyses is conspicuous in the distal femur (Fig. 3.27). The bony cortex is often indistinct distally as it approaches the subperiosteal bone collar (SPBC). This pattern is most evident medially, where the cortex may actually be discontinuous. The metaphyseal margin consists primarily of lateral trabeculae of the primary spongiosa that have been exposed by osteoclastic activity (see Chapter 1) (83). This pattern is less evident laterally, where a long SPBC is often visible on the frontal radiograph. In contrast to the medial SPBC, which tends to terminate near the chondro-osseous junction (COJ), the lateral collar often extends further distally along the physis, resulting in a spurlike metaphyseal extension (Fig. 3.27) (see Chapter 12) (82, 84).
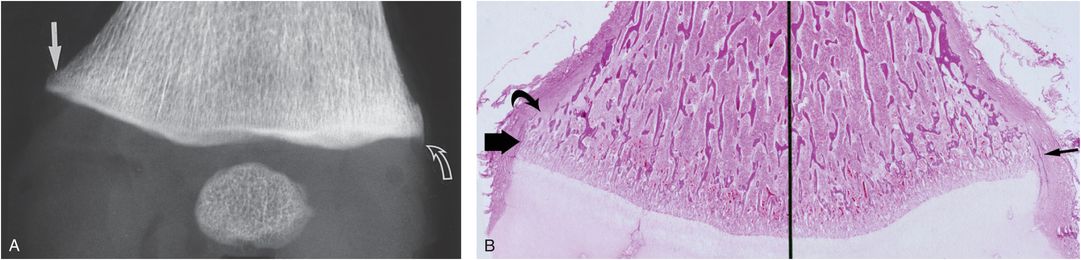
Figure 3.27 Normal left distal femur of a two-month-old infant. A, Normal flaring of the distal femoral metaphysis is most evident medially, where a step-off configuration is present (solid arrow). Laterally, the SPBC extends beyond the COJ, producing a spur pattern (curved arrow). B, Corresponding photomicrograph shows the medial SPBC (thick arrow). The adjacent metaphyseal margin is formed by the trabeculae of the primary spongiosa, which have been exposed by osteoclastic resorption (curved arrow). Laterally, the SPBC (thin arrow) extends beyond the metaphysis along the physeal margin, explaining the spur pattern seen radiographically. (From Kleinman PK, Marks SC Jr. A regional approach to the classic metaphyseal lesion in abused infants: the distal femur. AJR. 1998;170:43–7.)
Radiologic–histologic correlates
In most instances the distal femoral CML is relatively localized to the medial and posterior metaphyseal margins. With more extensive injury, the fracture plane extends anteriorly and laterally. Thus, when good quality images are obtained, the CML is usually evident medially, with lateral involvement in the case of more extensive injuries. Occasionally only a lateral component will be evident.
The acute CML is a subtle lesion radiographically. If there is no displacement of the fracture fragment, the lesion may be invisible or manifested only as a transverse subphyseal radiolucency. The lucency lies just above the zone of provisional calcification (ZPC), a mineralized region which includes the metaphyseal primary spongiosa and the calcified matrix surrounding the terminal chondrocytes in the lower hypertrophic zone of the physis (see Chapters 1, 2). As the fracture line extends peripherally and approaches the cortex, it undercuts the SPBC. Subphyseal radiolucency, without distinct cortical disruption, is a nonspecific radiographic finding difficult to differentiate from other causes of metaphyseal radiolucency (see Chapters 7, 12).
If mild displacement of the fragment is present, and/or if the projection yields superimposition of the margin of the fracture fragment over the adjacent metaphysis, a dense band defining the fracture line will be visible. This results in the corner fracture pattern (Fig. 3.28A). If the bone is projected with craniocaudad angulation, the larger peripheral fragment may be viewed as a crescentic radiodensity corresponding to the bucket handle pattern (Fig. 3.28B). Histologically, a plane of injury is seen across the trabecular transition zone at the junction of the primary and secondary spongiosa (Fig. 3.28C). (See Chapters 1 and 2.) At the periphery of the bone, the fracture line veers proximally to undercut the SPBC. The resultant larger peripheral fragment accounts for the corner fracture and bucket handle patterns visible radiographically.
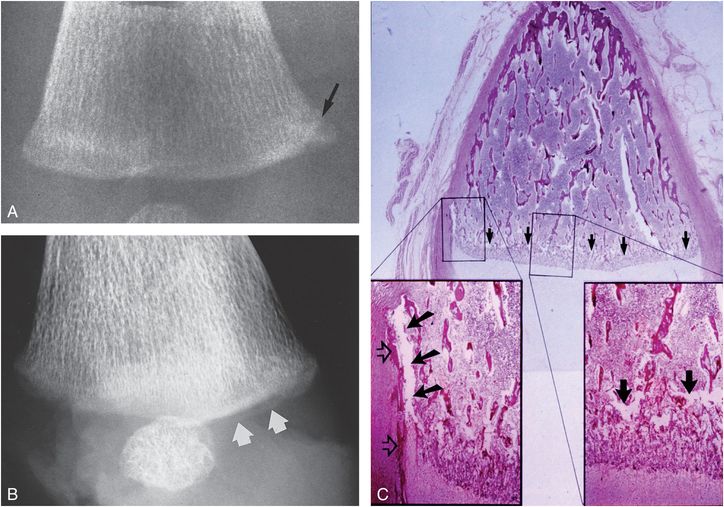
Figure 3.28 Distal femoral CML, acute. A, AP radiograph of the distal right femur in a one-month-old abused infant demonstrates a corner fracture pattern medially. A dense oblique band of radiodensity is present at the interface between the fragment and the adjacent metaphysis (arrow). B, Oblique specimen radiograph with caudal angulation shows a bucket handle pattern posteromedially (arrows). C, A corresponding oblique photomicrograph through the medial femoral condyle demonstrates an irregular plane of disruption along the primary spongiosa (arrows). The bottom right insert shows the plane of trabecular microfractures (arrows). There is no evidence of repair or hemorrhage. The bottom left insert demonstrates peripheral extension of the fracture line (solid arrows), which undercuts the SPBC (open arrows). (From Kleinman PK, Marks SC Jr. A regional approach to the classic metaphyseal lesion in abused infants: the distal femur. AJR. 1998;170:43–7.)
The healing distal femoral CML demonstrates radiologic and histologic features similar to those of injuries at other anatomic sites. Transmetaphyseal extension of the fracture can result in a band of metaphyseal radiolucency (Fig. 3.29A), a finding indistinguishable from that noted with acute injury.
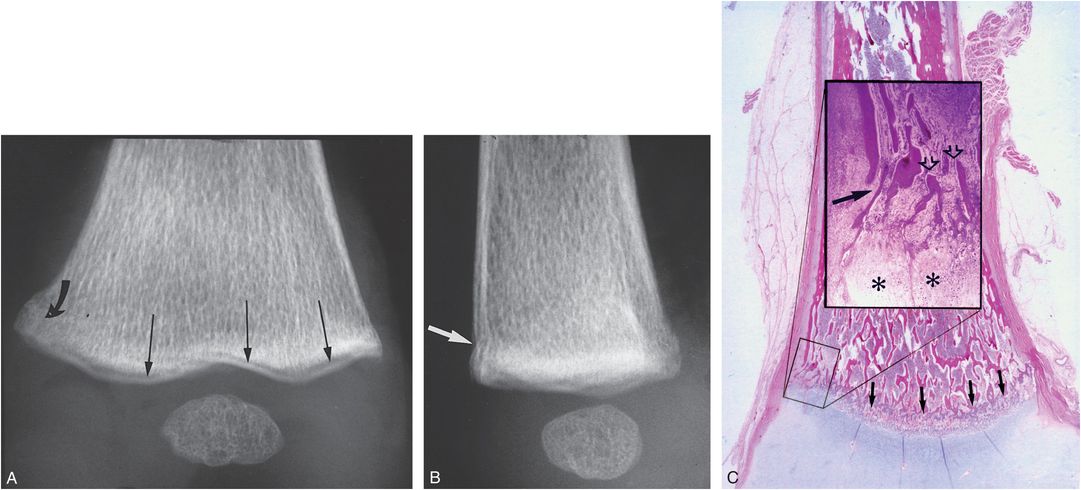
Figure 3.29 Distal femoral CML, healing. A, AP specimen radiograph of the distal left femur in a one-month-old abused boy demonstrates a zone of subphyseal radiolucency (long arrows). Medially, the fracture veers proximally (curved arrow), resulting in a faint corner fracture configuration. B, Lateral specimen radiograph shows disruption of the anterior metaphyseal cortex (arrow). C, Corresponding sagittal photomicrograph shows the plane of fracture extending across the metaphysis (arrows). The insert demonstrates inward displacement of the SPBC (solid arrow) corresponding to the radiographic finding in B. Amputated metaphyseal trabeculae are visible (open arrows). Osteoclastic bone resorption and granulation tissue are present, and an increase in the thickness of the hypertrophic chondrocyte zone is visible (asterisks). (From Kleinman PK, Marks SC Jr. A regional approach to the classic metaphyseal lesion in abused infants: the distal femur. AJR. 1998;170:43–7.)
Careful inspection of the margin of the metaphysis may show extension of this lucency to the periphery of the bone, with disruption of the metaphyseal cortex (Fig. 3.29B). Histologically, the fracture is evident as a series of trabecular fractures extending across the metaphysis (Fig. 3.29C). In the periphery, the fracture undercuts the SPBC at the site of cortical disruption. The typical features of osseous repair are evident, including fibrosis, osteoclastic bone resorption, and new bone apposition. Accumulations of hypertrophic chondrocytes at the site of injury indicate extension of physeal cartilage into the metaphysis. This is a reliable histologic indicator of healing (85, 86). Another radiographic pattern of the healing CML is a relatively discrete medial metaphyseal fragment corresponding to the corner fracture pattern (Figs. 3.29A, 3.30A).
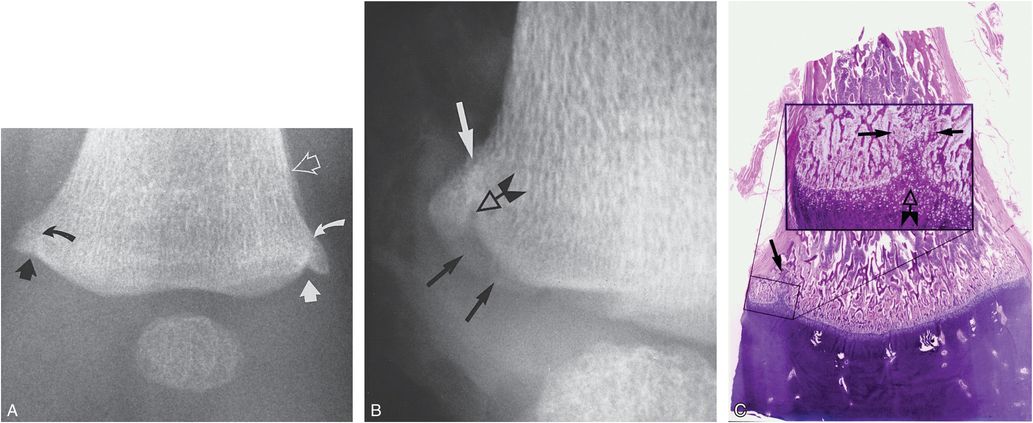
Figure 3.30 Distal femoral CML, advanced healing. A, AP radiograph of the distal left femur from SS of a four-month-old abused infant shows sclerotic fracture lines medially (black curved arrow) and laterally (white curved arrow), producing corner fracture configurations. Extension of radiolucency from the physis into the metaphysis is noted medially (straight solid black arrow) and laterally (solid straight white arrow). SPNBF is noted laterally (open arrow). B, Specimen radiograph of the medial metaphyseal margin demonstrates a bucket handle fracture pattern (solid black arrows). Extension of physeal radiolucency into the metaphysis is noted (open arrow). Proximal to this point there is faint sclerosis, reflecting healing (white arrow). C, Corresponding photomicrograph shows trabecular disruption medially at the fracture site (arrow). The insert demonstrates focal extension of hypertrophic chondrocytes into the metaphysis (open arrow). Trabecular reconstitution along the fracture line is noted between the solid arrows. These findings are consistent with advanced healing. (From Kleinman PK, Marks SC Jr. A regional approach to the classic metaphyseal lesion in abused infants: the distal femur. AJR. 1998;170:43–7.)
The conspicuity of this fracture relates to the reparative changes near the COJ. As the fracture line courses from the medial cortex toward the physis, a prominent vertical radiolucent extension from the physis is evident. Histologically, this corresponds to the thickening of the zone of hypertrophic chondrocytes along the plane of osseous disruption (Fig. 3.30C).
The dependence of the corner fracture and bucket handle pattern upon technique is well seen in Fig. 3.30. Corner fracture patterns are visible medially and laterally with marginal sclerosis. When the metaphyseal margin is tipped and projected at an obliquity, the corner fracture pattern transforms to a bucket handle CML (Fig. 3.30B). The focal extension of physeal lucency and SPNBF are reliable indicators of healing (Fig. 3.30A,B). Histologically, a focal extension of hypertrophic chondrocytes corresponds to the extension of physeal lucency into the metaphysis radiographically (Fig. 3.30C). Lesions with advanced healing and those that have sustained repetitive injury may manifest fragmentation and sclerosis of the metaphyseal margin (56).
The dependence of the imaging characteristics on the radiographic projection is illustrated in Fig. 3.31. When the large peripheral component of the fracture fragment is projected tangentially, a roughly triangular fragment is visible. When the fragment is projected at an obliquity due to flexion at the knee and/or angulation of the x-ray beam, this larger fragment is projected as a curvilinear radiodensity. Depending on the extent of metaphyseal disruption, the osseous fragment may be restricted to a medial location, may be visible both medially and laterally, or with severe injury may extend continuously from the medial to the lateral surface. With these extensive transmetaphyseal injuries, the pathologic and imaging patterns of distal femoral CMLs may overlap with those of SH injuries (Fig. 3.32) (87). The displaced fragment may strip the posterior periosteum with subsequent SPNBF. Although the principal injury is along the margin of the primary spongiosa, the fracture may meander into the physis. Because of the extent of the injury, striking evidence of healing and remodeling will be apparent pathologically.
Figure 3.31 Diagram of the corner fracture and bucket handle patterns of the CML in the distal femur. Top images, extensive injury; bottom images, localized injury. Fractures (arrows) extend adjacent to the COJ and then veer proximally to undercut the larger peripheral segment that encompasses the SPBC. When the physis is viewed tangentially, the CML appears as a corner fracture pattern (left images). When a view is obtained with beam angulation, a bucket handle pattern results (right images). (From Kleinman PK, Marks SC Jr. A regional approach to the classic metaphyseal lesion in abused infants: the distal femur. AJR. 1998;170:43–7.)
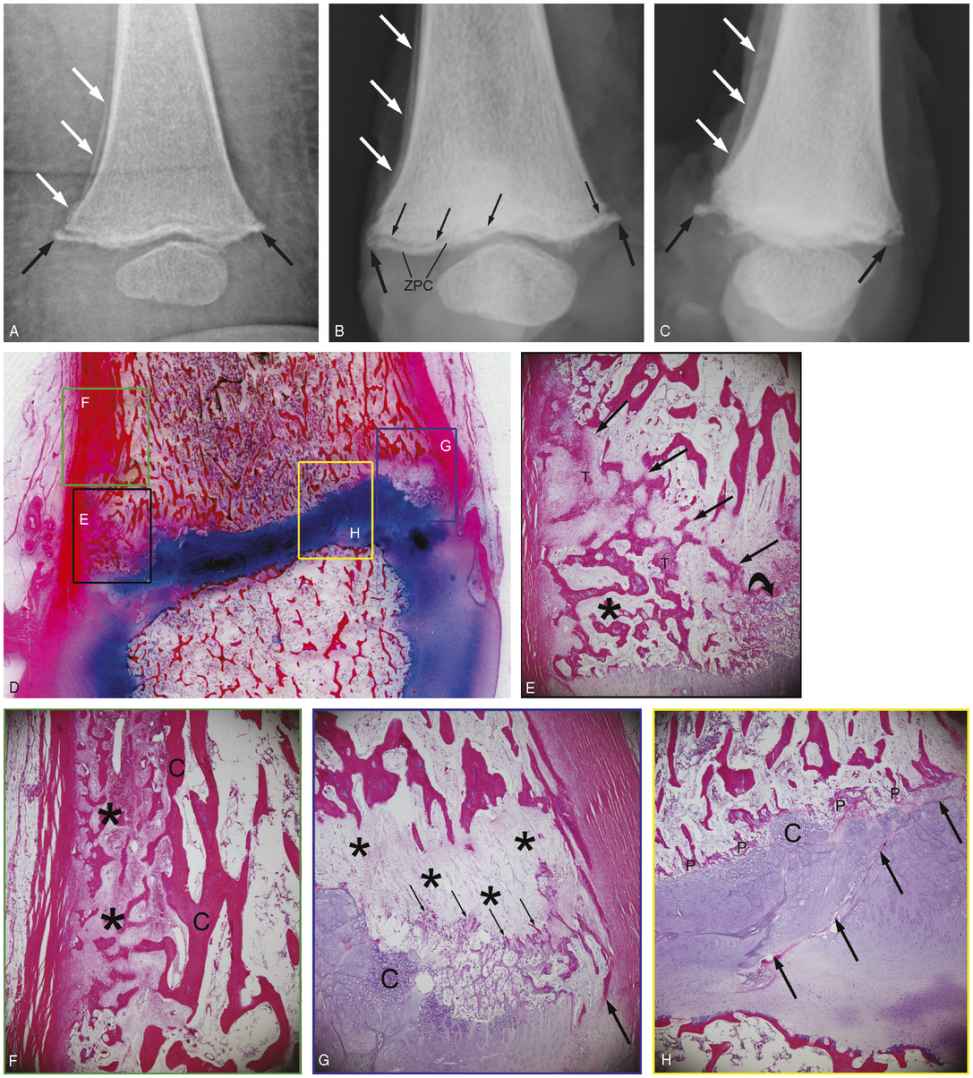
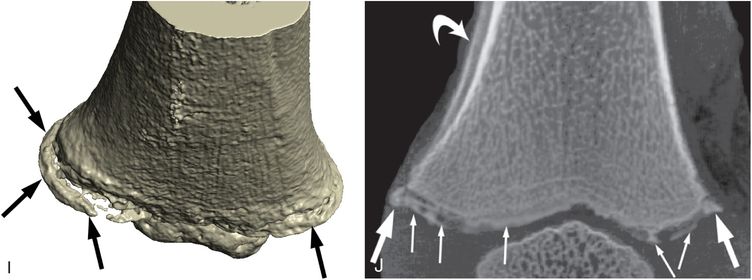
Figure 3.32 Extensive displaced distal femoral CML, with physeal involvement, healing. Nine-month-old fatally abused infant. A, AP radiograph of the distal left femur from the SS shows a CML with medial and lateral components (black arrows). The medial fragment is displaced and there is SPNBF (white arrows). AP (B) and lateral (C) specimen radiographs show the metaphyseal fragments (thick black arrows) with central extension of the subphyseal fracture radiolucency (thin arrows), which separates the ZPC. The posterior fragment is displaced and there is SPNBF (white arrows). D, Very low power sagittal histologic section. E–H, Low power photomicrographs of the boxed regions in D. E, Posteriorly the plane of injury (straight arrows) extends from the periphery obliquely through the spongiosa isolating a peripheral osseous fragment (*) corresponding to the radiographs. There is evidence of repair with early intramembranous bone formation of new trabeculae (T). Note the focal extension of hypertrophic cartilage into the primary spongiosa (curved arrow). F, More proximally there is thick SPNBF (*) extending to the cortex (C). G, Anteriorly, there is a conspicuous region of loose connective tissue devoid of trabeculae that have been resorbed (*). Early reconstitution of primary spongiosa is evident (thin arrows). There is focal thickening and disorganization of the hypertrophic cartilage (C). Thick arrow = SPBC. H, Centrally, a fracture component extends obliquely across the physis (arrows). There is early reconstitution of primary spongiosa (P) and focal cartilage extension (C). I, 3D-CT surface rendering shows the peripheral component of the fracture (arrows). J, Coronal MIP image shows extension of the fracture to the interior. The large peripheral fragment (thick arrows) is continuous with the more central components (thin arrows) composed of the ZPC. Curved arrow = SPNBF. Two weeks earlier the infant had been hospitalized for a sublingual hematoma.
More commonly, the zone of trabecular disruption and repair tends to be limited to the periphery of the bone, sparing the central portions of the primary spongiosa (Fig. 3.33). This pattern of injury appears to be greater in the distal femur than at other sites. The higher propensity for failure of trabeculae in the periphery suggests a torsional mechanism that applies greater displacement strains to the superficial regions versus the interior of the medullary cavity. Technical factors, as well as the age and morphologic peculiarities of the osseous injury, result in a wide spectrum of radiologic patterns of the distal femoral CML (Fig. 3.34).
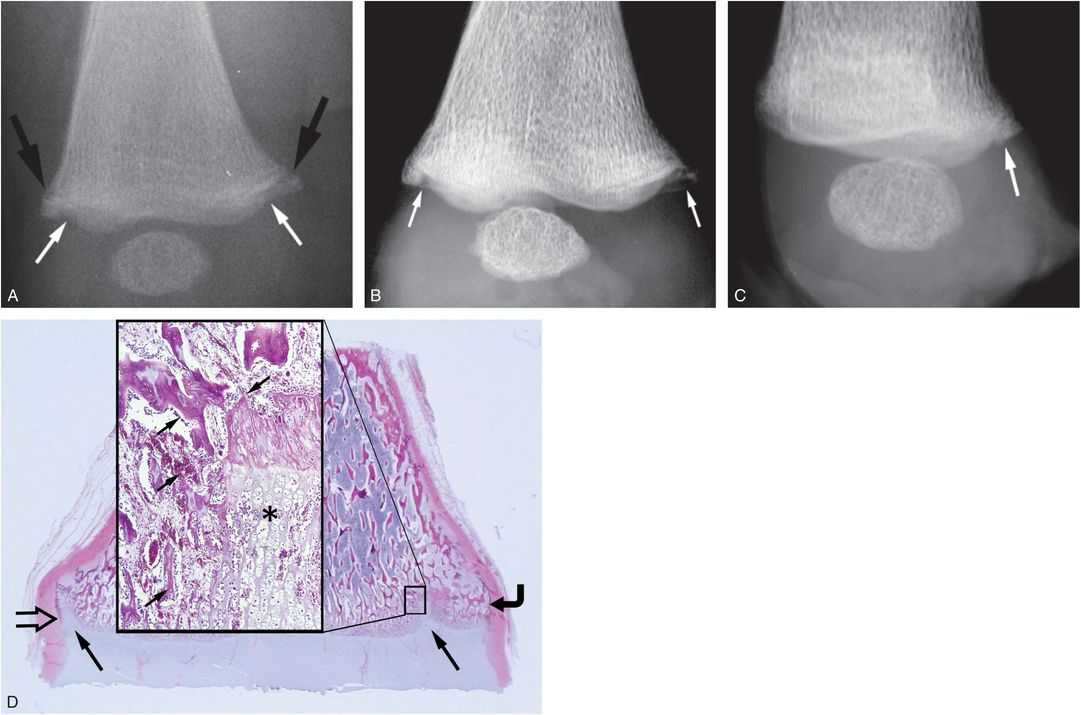
Figure 3.33 Zone of trabecular disruption and repair limited to the periphery. A seven-month-old fatally abused infant. A, Postmortem AP radiograph of the right distal femur demonstrates a corner fracture pattern of the margins of the distal femur (large black arrows). There is extension of physeal lucency into the metaphysis and marginal sclerosis (small arrows). B, AP specimen radiograph of the distal right femur displays the character of the CML fragments and extension of physeal lucency to advantage (arrows). C, The lateral view suggests an injury limited to the posterior metaphyseal margin (arrow). D, Corresponding coronal low power photomicrograph shows extension of physeal cartilage into the metaphysis (large arrows). The central metaphysis is spared. Note that the size and shape of the corner fracture fragment varies, with the generous medial fragment (curved arrow) that involves a substantial width of the primary spongiosa and a smaller lateral fragment which consists mainly of the SPBC (open arrow). The insert in D shows extensions of cartilage columns into the metaphysis (*) and bony repair (arrows). There were additional skeletal injuries including CMLs of the ipsilateral proximal and distal tibia. (Also see Fig. 3.46.) (From Kleinman PK. Problems in the diagnosis of metaphyseal fractures. Pediatr Radiol. 2008;38(Suppl. 3):S388–94.)
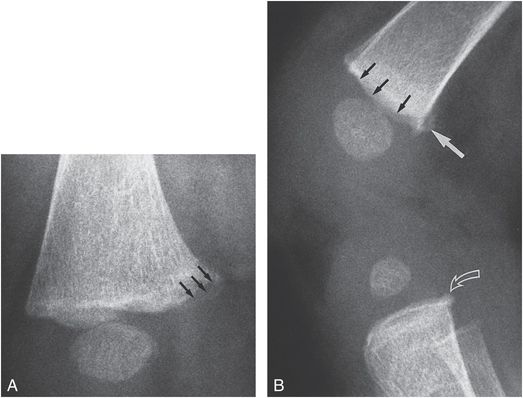
Figure 3.34 Distal femoral CML in a 4-month-old former 28-week premature infant with a history of a 1½-ft fall from a bed. A, Oblique view of the distal right femur shows a bucket handle pattern medially. Note the sclerotic margins of the fracture line (arrows) indicating advanced healing. No SPNBF is present. B, Lateral view demonstrates irregularity of the metaphyseal margin (solid small arrows) and a corner fracture pattern posteriorly (solid large arrow). A CML is present in the proximal tibia (open arrow). A subsequent history was obtained from the caretaker that the infant was forcefully “snatched” by the legs during a diaper change on a bed.
Despite the frequency of the lesion, SPNBF is an uncommon occurrence (Figs. 3.30, 3.32). As noted, the acute CML may be inconspicuous or absent initially, and a follow-up SS in several weeks can be valuable to document injury. When the lesion is visible initially, dating may be difficult and the follow-up study can provide valuable information in this regard (Figs. 3.35, 3.36). Actual growth of the fracture fragment occurs with continued enchondral ossification at the COJ (Fig. 3.37). A corner fracture pattern evident initially can evolve to a bucket handle appearance as the fragment grows, and the full extent of the fracture line becomes more conspicuous (Fig. 3.37).
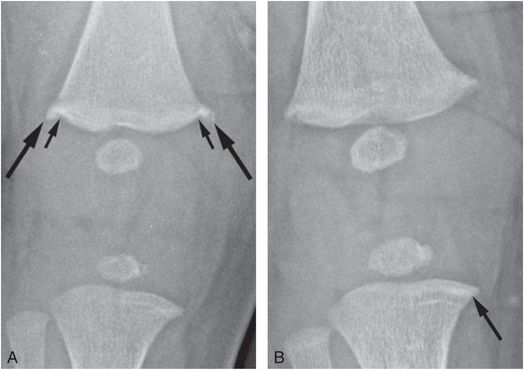
Figure 3.35 Healing CML in twin infant. A 14-week-old infant evaluated because of unexplained skull fracture and metatarsal fractures in twin sibling. Shoulder bruising was evident on physical examination. A, AP view of the right knee reveals distal femoral CMLs with corner fracture patterns (large arrows). Extension of physeal lucency into the metaphysis is noted (small arrows) with the suggestion of marginal sclerosis. B, A radiograph two weeks later shows nearly complete resolution, confirming that the injury was healing on the initial radiograph. There is also a transverse sclerotic band in the medial metaphysis of the proximal tibia (arrow), suggesting an additional healing CML.
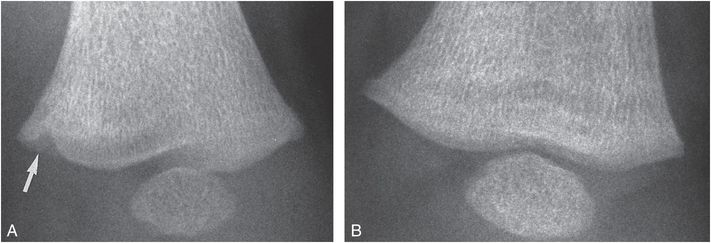
Figure 3.36 Distal femoral CML, complete healing. A, AP view of the distal left femur in a five-month-old abused infant shows a healing CML manifest as an area of extension of physeal radiolucency into the medial metaphyseal margin (arrow). B, A follow-up study three weeks later shows complete resolution of findings.
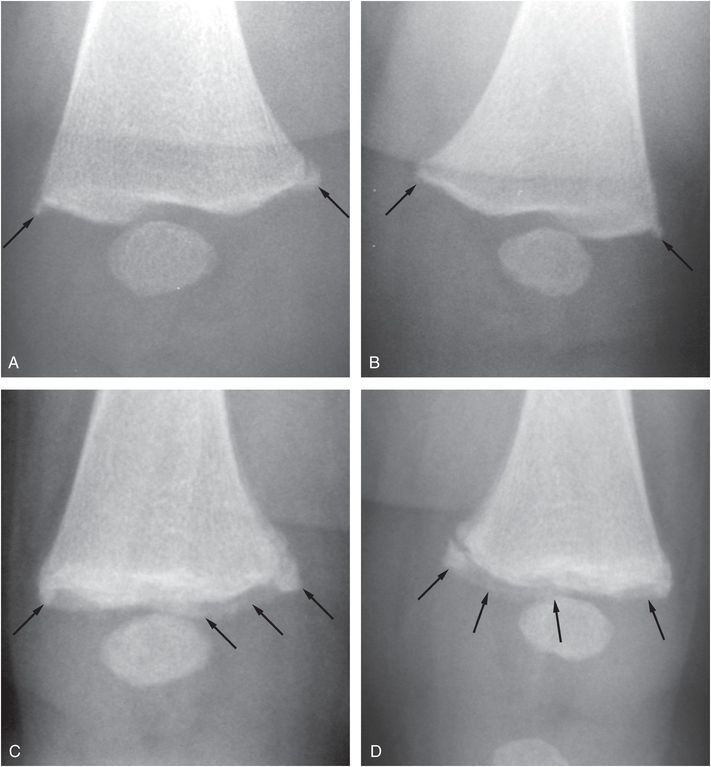
Figure 3.37 “Growing” distal femoral CML fragments. A three-month-old infant with multiple rib fractures noted on an abdominal radiograph done for diarrhea. (Same patient shown in Figs. 3.76, 3.104.) A, B, AP views of the right and left distal femurs show bilateral CMLs (arrows). C, D, Corresponding follow-up images two weeks later show enlargement of the fracture fragments (arrows) due to further apposition of enchondral bone distal to the fracture sites. The appearances progress from corner fractures to bucket handle patterns with age.
As with CMLs elsewhere, radiography, with tight collimation, liberal use of oblique projections, and follow-up imaging, remains the mainstay for detection and characterization. As noted with respect to lesions of the proximal femur, when optimized, scintigraphy with 18F-NaF PET also shows promise of greater detection than 99mTc-based bone scans for distal femoral CMLs (Fig. 3.38).
Figure 3.38 Scintigraphy with 18F-NaF PET. A one-month-old infant with bronchiolitis, apnea, and an unsuspected skull fracture. (Same patient as in Fig. 3.51.) MIP 18F-NaF PET image of the distal femurs with contrast optimized to visualize the region of the growth plate shows increased uptake (arrow) in the medial metaphysis of the left femur, correlating with the finding radiographically in Fig. 3.51B.
Markowitz and associates explored the use of sonography to assess the normal anatomy and features of the distal femoral CML (88). They nicely demonstrated the SPBC, most visible medially, and suggested that asymmetry in the appearance of this structure as compared with the opposite side may indicate metaphyseal injury. Sonography has an established role in the evaluation of distal femoral epiphyseal separations (see below).
Physeal injuries and epiphyseal separations
In contrast to the CML, distal femoral epiphyseal separation is usually a major injury resulting from severe force applied to the knee (Fig. 3.39). If the child is seen after the acute event, the injury may be readily evident. When the fracture is neglected, the lesion may be noted on a SS performed on other grounds for suspected abuse.
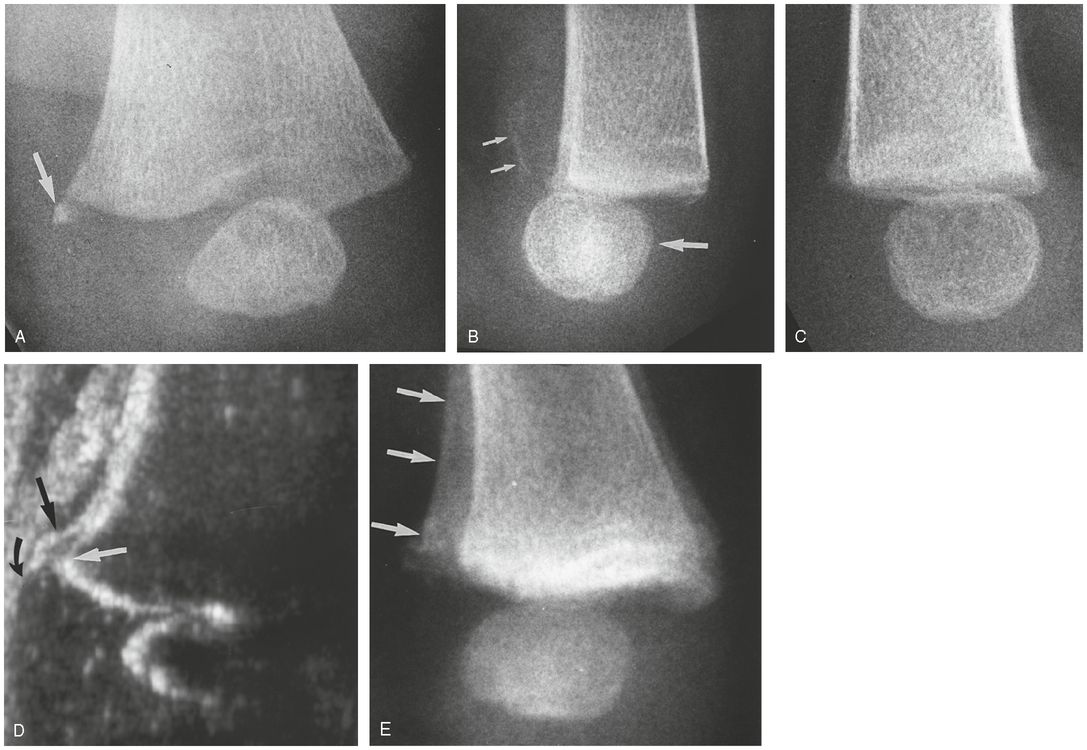
Figure 3.39 Distal femoral epiphyseal separation. A, Oblique view of the distal left femur in a three-month-old abused infant demonstrates a small osseous metaphyseal fragment medially (arrow). The pattern suggests a common CML. B, Lateral view demonstrates posterior displacement of the epiphysis with respect to the metaphysis (large arrow). Note the faint SPNBF (small arrows). C, Lateral view of the normal right side for comparison. D, Sonogram performed in a coronal oblique projection from the posteromedial aspect of the knee demonstrates posteromedial displacement of the hypoechoic distal femoral epiphysis (curved arrow) from the echogenic metaphyseal margin (white arrow). Note the echogenic SPNBF (straight black arrow). Compare with image B. E, Follow-up LPO radiograph one month later demonstrates dense SPNBF (arrows) and epiphyseal displacement corresponding to the sonographic image.
The appearance on initial images may be normal if there is no epiphyseal displacement and no associated metaphyseal fracture. With displacement, the finding may be subtle (Fig. 3.39A) and the true extent of the injury will be evident only on the lateral projection (Fig. 3.39B). Subtle displacement is best appreciated if a comparison view of the opposite femur is obtained (Fig. 3.39C). As the epiphysis is displaced, it strips the adjacent periosteum, and thus, with early healing, faint SPNBF will be noted along the margin of the metaphysis adjacent to the displaced epiphysis (Fig. 3.39B). Sonography is a relatively simple and inexpensive means of documenting this injury (Figs. 3.39D, 3.40). If there is no displacement of the epiphyseal ossification center, a SH type II injury will be indistinguishable from the more common CML pattern. Sonography can demonstrate periosteal stripping and elevation above a SH injury prior to the radiographic evidence of healing. This will herald the development of extensive SPNBF, a feature usually lacking with CMLs. MRI nicely shows the subperiosteal fluid and predicts the development of SPNBF on follow-up radiographs (see Fig. 3.14). The severity of the injury may also be apparent on bone scan, as a zone of decreased tracer uptake within the metaphysis, perhaps reflecting medullary hemorrhage and decreased marrow perfusion (Fig. 3.41).
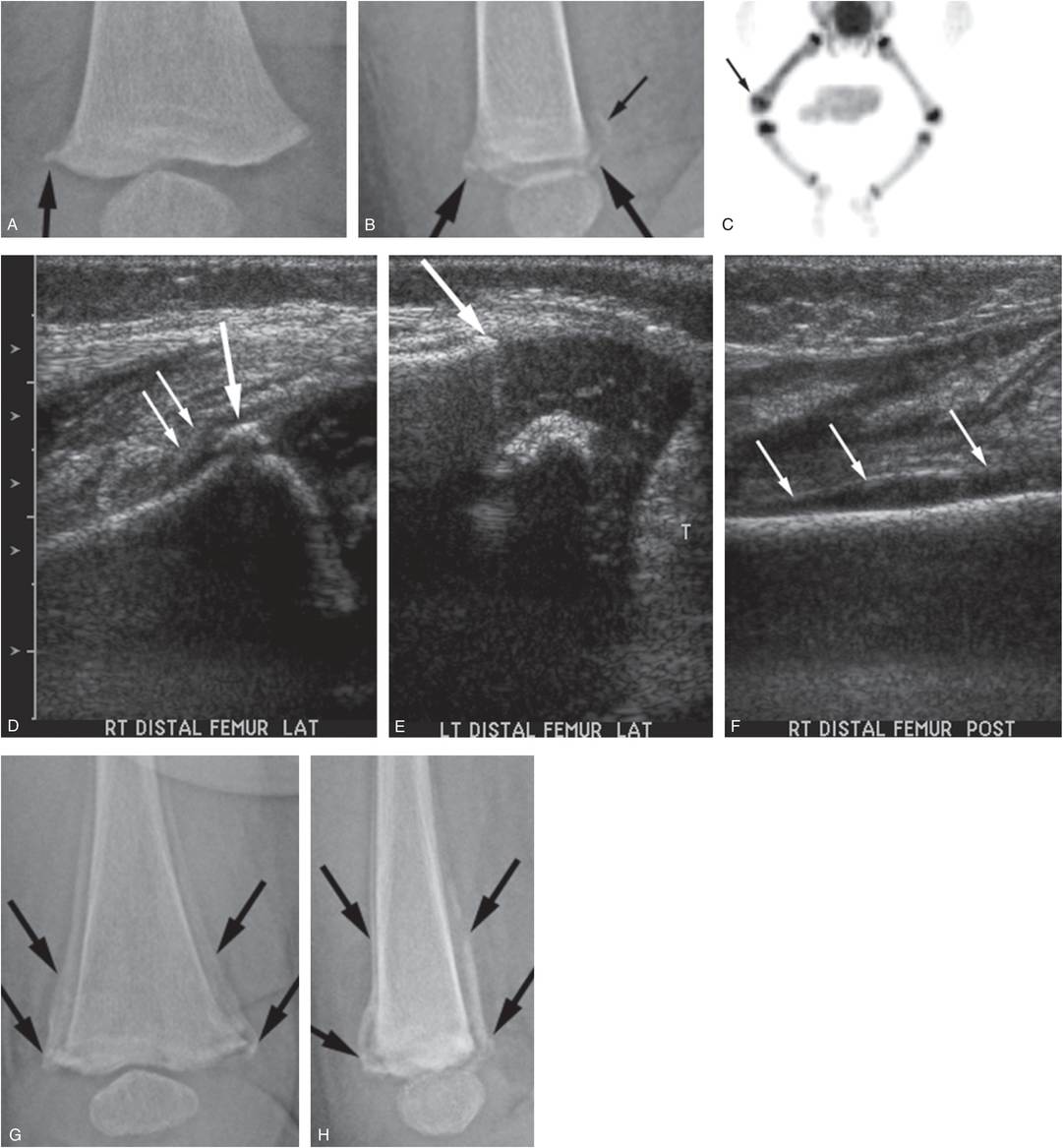
Figure 3.40 Distal femoral epiphyseal separation. A two-month-old infant not moving right leg. AP (A) and lateral (B) views of the distal right femur demonstrate a fracture (large arrows) involving the juxtaphyseal metaphysis. There is faint SPNBF evident posteriorly (small arrow) suggesting displacement and periosteal stripping. C, Anterior MIP 18F-NaF PET image of the lower extremities shows focal increased uptake in the right distal femoral metaphyseal–epiphyseal region, and more generalized increased activity in the mid and distal shaft. D, Sonogram of the right distal femur acquired from a lateral approach with a comparison view of the left (E) shows a juxtaphyseal metaphyseal fracture fragment incorporating the SPBC (large arrow), associated with periosteal stripping (small arrows). Note the intact collar (arrow) and periosteum on the left. F, Posterior image shows periosteal elevation extending proximally (arrows), correlating with the finding in B. The extent of abnormal uptake on the bone scan and the periosteal stripping evident sonographically point to an epiphyseal separation, rather than a simple CML. AP (G) and lateral (H) views of the distal right femur two weeks later show extensive SPNBF (arrows) pointing to a SH type II physeal injury/epiphyseal separation.
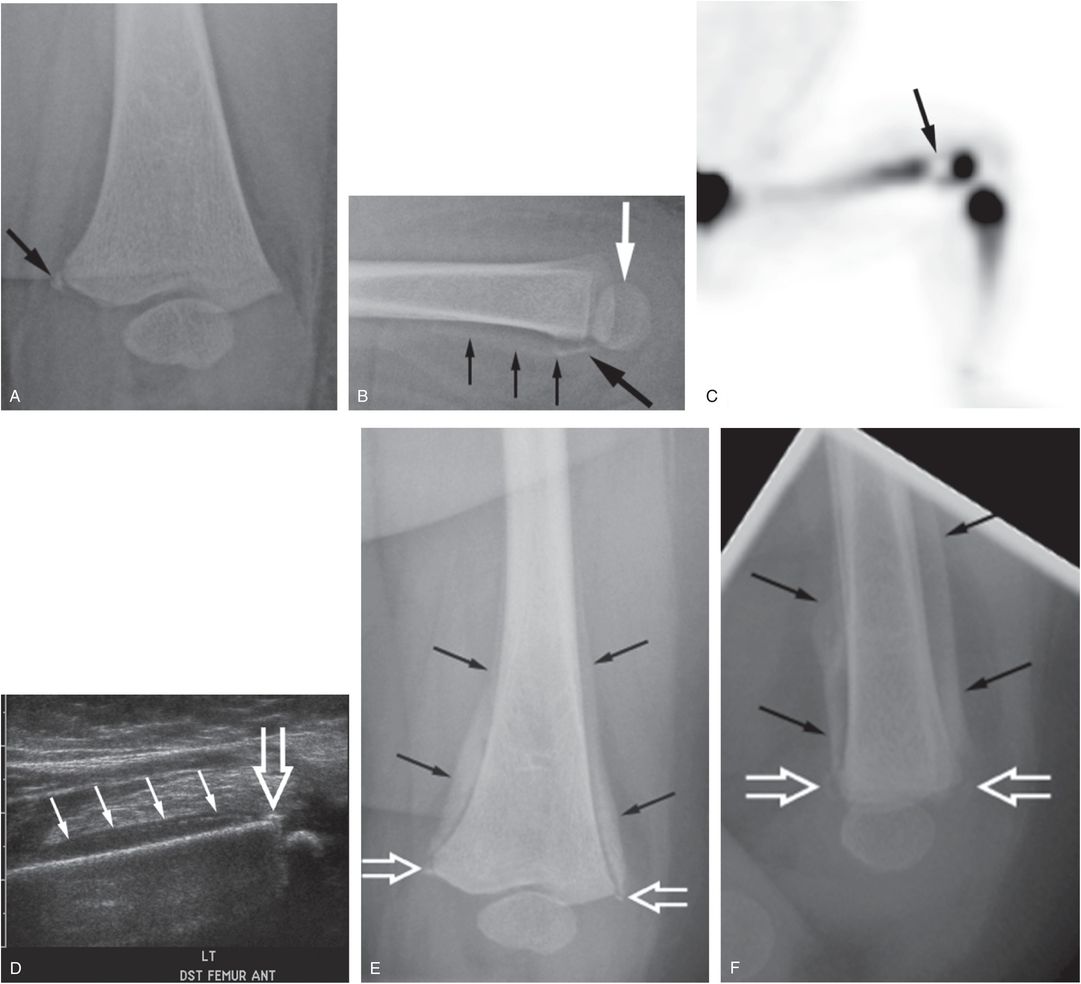
Figure 3.41 Distal femoral epiphyseal separation. A six-month-old infant with multiple bruises and decreased movement of the left leg following a reported fall in the bathtub. (See same patient in Fig. 4.51.) Oblique (A) and lateral (B) views of the left knee demonstrate a fracture fragment arising from the posteromedial aspect of the distal femoral metaphysis (large black arrows). There is slight posterior displacement of the distal femoral epiphysis (white arrow) and the suggestion of early SPNBF (small arrows) along the posterior metaphysis. C, Anterior MIP 18F-NaF PET image of the left lower extremity shows a sharply marginated photopenic region in the distal femoral metaphysis (arrow). D, Sagittal sonogram obtained via an anterior approach shows anterior periosteal elevation (solid arrows) and a metaphyseal fragment encompassing the SPBC (open arrow). The scintigraphic and sonographic features, in conjunction with the posterior displacement of the distal femoral epiphysis point to a SH type II injury. SS also showed rib and ulnar shaft fractures. AP (E) and lateral (F) views of the left femur 10 days later show extensive SPNBF surrounding the distal diaphysis and metaphysis (black arrows), extending to the metaphyseal fracture fragment (open arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree