Lower Leg
Case 7.1 Blount Disease (Tibia Vara)
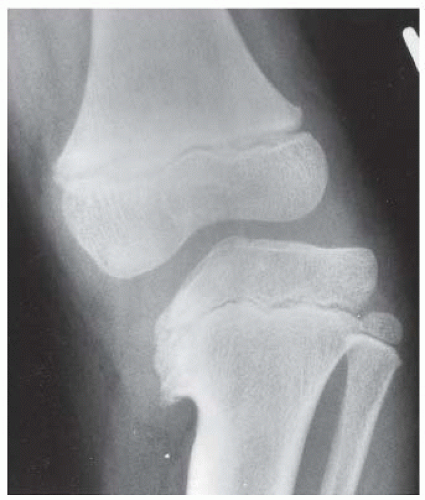
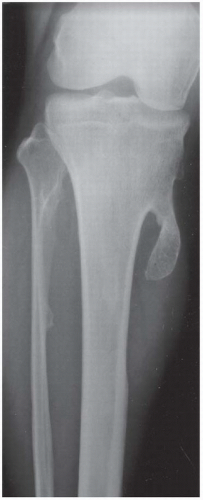
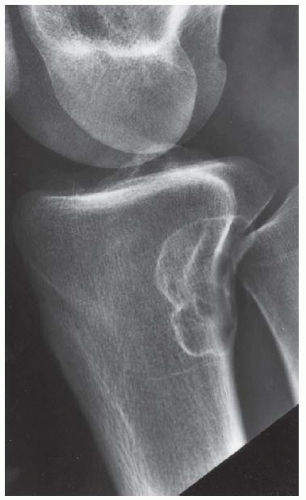
CLINICAL HISTORY Progressive bowing of lower extremities. A-B, radiographs at age 3; C, radiograph at age 7.
FINDINGS
A, B. Anteroposterior (AP) and lateral radiographs of the left knee at age 3 years demonstrate a varus deformity of the tibia with a prominent medial metaphyseal beak.
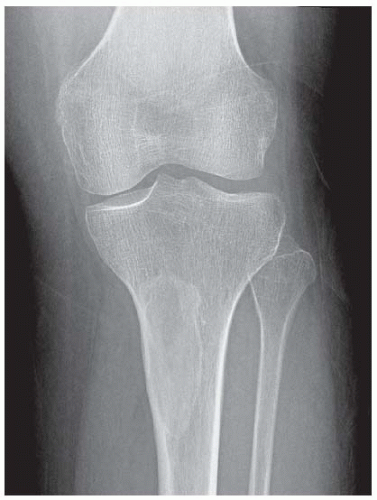
C. AP radiograph of the knee at age 7 years shows progression of the varus deformity, slanting of the medial tibial plateau, with persistent metaphyseal beak.
DIFFERENTIAL DIAGNOSIS Blount disease, posttraumatic deformity, rickets, physiologic bowing.
DIAGNOSIS Blount disease (tibia vara).
DISCUSSION The diagnosis in this case is made by recognizing the abnormally small, beaked appearance of the medial portion of the tibial metaphysis, with genu varus. These findings, in conjunction with a normal appearance of the lateral portion of the tibial metaphysis and normal femoral metaphysis, lead to the correct diagnosis.
Blount disease of the tibia is an entity subsumed within the larger group of disorders known as osteochondroses, recognized individually by the specific site of involvement within the skeleton. Other examples of osteochondroses include such entities as Legg-Calvé-Perthes disease of the capital femoral epiphysis and Kienböck disease of the lunate. Blount disease specifically affects the medial portion of the proximal tibial metaphysis. The etiology of the abnormal development of the medial portion of the metaphysis is unknown. Abnormal development of the medial metaphysis results in the characteristic metaphyseal beak and genu varus deformity. Magnetic resonance imaging (MRI) is helpful to evaluate the growth plate in patients who are already affected and in patients who are at risk, such as toddlers with delayed resolution of physiologic tibial bowing [1,2].
Case 7.2 Neurofibromatosis (Type I)
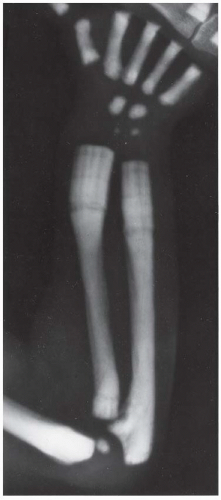
CLINICAL HISTORY (A) A 3-year-old boy with progressive tibial bowing deformity. (B) Companion case.
FINDINGS
AP radiograph of the lower leg. There is anterolateral bowing of the tibia, with increased sclerosis of the medullary cavity. A nonunion of the fibula is noted distal to the angular deformity.
AP radiograph of the lower leg shows anterolateral bowing of the shafts of the tibia and fibula.
DIFFERENTIAL DIAGNOSIS Neurofibromatosis (NF), osteogenesis imperfecta, fibrous dysplasia, posttraumatic deformity.
DIAGNOSIS Neurofibromatosis (Type 1).
DISCUSSION NF is an autosomal dominant disorder affecting neural crest cells. Cases may be classified according to the genetic defect as Type 1 (NF-1), Type 2 (NF-2), or schwannomatosis. Among other manifestations, NF-1 is associated with cutaneous and peripheral neurofibromas, skeletal deformities, and cafe au lait spots. Scoliosis and kyphosis are the most common skeletal abnormalities. Tibial bowing may occur in approximately 3% of NF-1 cases. The bowing is anterolateral, usually involves both tibia and fibula, and is associated with medullary sclerosis. These abnormal bones are prone to fractures and development of a pseudoarthrosis; orthopedic intervention may become frustrating as fractures and osteotomies fail to heal [3]. NF-1 is the most common form of NF; patients with NF-2 develop bilateral acoustic neuromas and do not have musculoskeletal manifestations.
Case 7.3 Osteogenesis Imperfecta
CLINICAL HISTORY A 4-year-old girl with multiple orthopedic problems.
FINDINGS
AP radiograph of the legs. The bones are osteoporotic. There are multiple healed femoral shaft fractures and severe posterior bowing deformities of the lower legs. The epiphyses at the knees are enlarged and have a popcorn appearance.
Frog lateral radiograph of both lower extremities shows osteoporosis, bowing deformities of the femurs, tibias, and fibulas, and multiple healed fractures.
DIFFERENTIAL DIAGNOSIS Osteogenesis imperfecta, fibrous dysplasia.
DIAGNOSIS Osteogenesis imperfecta.
DISCUSSION Osteogenesis imperfecta is a group of inborn connective tissue disorders characterized by radiographically decreased bone density. The underlying problem is one of abnormal collagen synthesis, in which a variety of different molecular defects in collagen produce a continuous spectrum of phenotypes. In the skeleton, the bone matrix is deficient, resulting in thin, osteoporotic, and fragile bones that are subject to repeated insufficiency fractures and consequent deformity. The condition is heritable, but cases are often sporadic. In general, there are autosomal recessive severe forms that present at birth and autosomal dominant forms that present later and have a mild course. The condition ranges from severe, congenital involvement with multiple fractures in utero and perinatal death to mild, late manifestations in adulthood. The severe forms account for 10% of cases, and the less severe forms account for 90% of cases. The incidence of osteogenesis imperfecta is 1 per 20,000 to 60,000 live births. Associated clinical features, with variable expression, include blue sclerae (90%); thin, translucent skin; hypermobile, lax peripheral joints; abnormal teeth (dentinogenesis imperfecta); and deafness (fragile otic bones). Bisphosphonate treatment has been helpful for patients with moderate to severe disease [4].
Case 7.4 Osteopetrosis, Precocious Form
CLINICAL HISTORY A young child with multiple orthopedic problems.
FINDINGS
AP radiograph of the lower extremities shows diffusely sclerotic bones without development of the medullary space. The metaphyses are undertubulated and club shaped.
Radiograph of an upper extremity of the same patient shows similar findings.
DIFFERENTIAL DIAGNOSIS Osteopetrosis, pyknodysostosis.
DIAGNOSIS Osteopetrosis, precocious form.
DISCUSSION All of the bones in this very young child show a generalized chalk-white density. The medullary cavity seems obliterated by the uniform density. The bone has a shape similar to a juggling club, with a narrow middle portion and a wider distal portion of uniform diameter. This shape is the result of longitudinal growth at the physis without bone resorption and remodeling in the cutback zone of the metaphysis, leaving the new bone the same diameter as the physis.
Osteopetrosis is a disorder due to abnormal function of the osteoclasts. There are autosomal recessive and dominant types. The autosomal dominant, or delayed form, is the most common. The precocious form (shown in this case) is inherited as an autosomal recessive trait and is usually lethal due to obliteration of the marrow. The osteoclasts fail to normally remodel bone. The unopposed osteoblastic activity leads to the generalized increase in bone density. The autosomal dominant form, of which there are two distinct genetic entities, was formerly known as marble bone disease or Albers-Schonberg disease [9].
Case 7.5 Congenital Adrenocortical Hyperplasia with Limb Lengthening
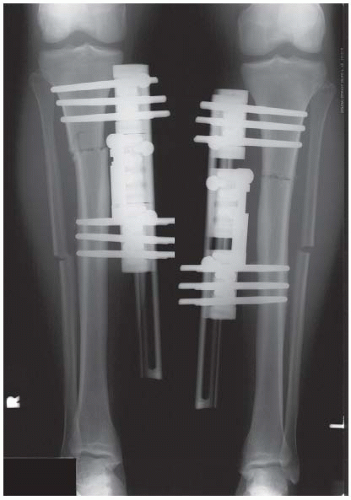
CLINICAL HISTORY An 18-year-old man with short stature. A, Postoperative radiograph; B, 5-month radiograph; C, 7-month radiograph.
FINDINGS
AP radiographs of the lower legs.
Pin-rod external fixators are present bilaterally, and osteotomies have just been performed through the proximal tibial and fibular shafts.
After 5 months of treatment, there has been a 6-cm gain in length.
After 7 months of treatment, the distracted fragments are bridged by remodeling bone.
DIFFERENTIAL DIAGNOSIS Limb lengthening for short stature (from any cause).
DIAGNOSIS Congenital adrenocortical hyperplasia with limb lengthening.
DISCUSSION Congenital adrenal hyperplasia is an autosomal recessive defect, involving the enzyme 21-hydroxylase, that results in failure to synthesize cortisol. There is a secondary overproduction of androgenic hormones that cause precocious puberty. The effect on the growing skeleton is rapid growth but premature closure of the epiphyses, so that a tall child becomes a short adult. The incidence of congenital adrenal hyperplasia is approximately 1 in 16,000, with a salt-wasting form from adrenal insufficiency and a simply virilizing form from excess androgens [5]. Conventional treatment is steroid replacement with exogenous corticosteroids. Surgical limb lengthening using the callus distraction (callotasis) has been applied to patients with developmentally short stature, such as those with achondroplasia [6,7,8]. In this technique, the cortex of the bone is partially cut, leaving the medullary contents intact. After 2 weeks, as soft callus forms, the two bone segments are slowly distracted by means of an external fixator, stretching out the callus as the gap between the fragments is increased 1 mm or so per day to lengthen the bone. Several centimeters of length can be gained, and the complication rate is relatively low. Once the desired length has been attained, healing and remodeling ultimately results in cortical bone formation. In this case, pin-rod external fixators have been used, and both tibias have been lengthened symmetrically.
Case 7.6 Physiologic Bowing
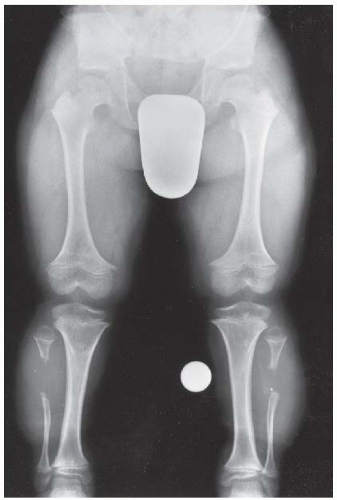
CLINICAL HISTORY Bowed legs in an infant.
FINDINGS AP radiograph of both lower extremities demonstrates a mild tibia vara without beaking of the proximal medial metaphyses or widening of the physes.
DIFFERENTIAL DIAGNOSIS Physiologic bowing, Blount disease, rickets.
DIAGNOSIS Physiologic bowing.
DISCUSSION The diagnosis in this case is made by recognizing that this is a young child with slight bowing of femurs and tibias centered at the knee, without any intrinsic abnormality. In particular, there is no medial tibial metaphyseal fragmentation. Mild enlargement of the medial tibial metaphyses can be present [10].
Physiologic bowing is thought to be related to the fetal position within the close confines of the uterus. It is selflimited. Parents usually bring these children in for evaluation between 1 and 2 years of age because of their bowed legs. Once the toddler begins to stand and walk, normal weight-bearing stresses correct the slight bowing.
Case 7.7 Achondroplasia
CLINICAL HISTORY A 4-year-old girl with short stature.
FINDINGS
Standing AP radiograph of the lower limbs. The long bones are short and thick with flared metaphyses.
Posteroanterior radiograph of the forearm and hand shows short but thick bones in the hand and forearm. The fingers have a stubby appearance.
AP radiograph of the upper arm shows a disproportionately short humerus. Note that with all the bones, there is a normal cortical and trabecular structure, and the bones have normal density.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Achondroplasia.
DISCUSSION Achondroplasia is a genetic disorder of abnormal enchondral ossification [11]. The long bones are abnormally short with metaphyseal flaring. Bone shortening is most prominent in the proximal aspect of the extremity (rhizomelic micromelia). The hand bones are short and broad, producing what is sometimes called a trident appearance. The acetabula are flat and the iliac bones are squared. Additional findings in achondroplasia (not shown) include a large cranium compared with the face, a small foramen magnum, a narrowed interpediculate distance in the lower lumbar spine, and concavity of the posterior vertebral bodies. The limb shortness in achondroplasia is being treated with increasing frequency by surgical limb lengthening (callotasis).
Case 7.8 Fibrous Dysplasia
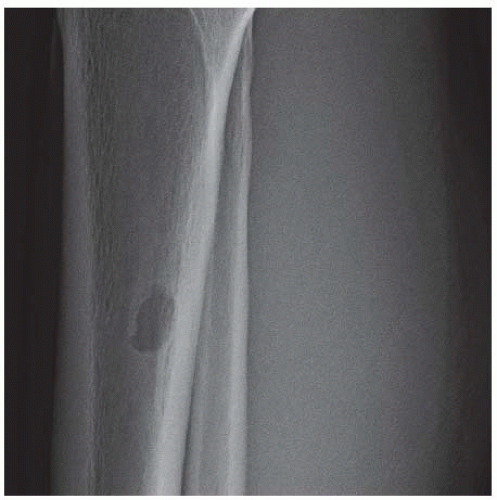
CLINICAL HISTORY A 42-year-old man with 1-month history of right anterior leg pain.
FINDINGS An AP radiograph (A), and coronal reconstructed computed tomography (CT) (B) of the proximal tibial diaphysis shows a focal lesion with ground-glass mineralization. The lesion has a faint sclerotic margin and is oriented along the long axis of the bone. (C) Coronal T1-weighted MRI shows an intramedullary lesion with low signal intensity. (D) Coronal T2-weighted, fat-suppressed MRI shows a heterogeneous intermediate and high-signal-intensity lesion with a low-signal-intensity margin. Increased radiotracer uptake is seen in the lesion on bone scan (E).
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Fibrous dysplasia.
DISCUSSION Fibrous dysplasia is a benign fibro-osseous lesion that is neither familial nor hereditary. Fibrous dysplasia appears to be a developmental abnormality involving the proliferation and maturation of fibroblasts, in which benign fibrous tissue, with abnormally arranged, dysplastic trabeculae of immature woven bone, replaces normal bone. The dysplastic trabeculae are no thicker than 0.1 mm, so they are not individually visible on clinical radiographs. If present in sufficient preponderance, however, they give the lesions a ground-glass density; if not, the lesions are radiolucent.
The lesions are medullary, but may replace both cancellous and cortical bone. The abnormal area may be sharply circumscribed and marginated by a thick layer of reactive bone, or it may blend gradually with the adjacent normal bone. The cortex may be either thickened or thinned, but frequently the outer size and shape of the affected bone is unchanged.
Bowing deformities result from biomechanically insufficient bone and from malunion of pathologic fractures. Lesions in the long bones are often discovered because of fracture or deformity. Therapy is restricted to orthopedic management of complications. The monostotic form is not associated with other abnormalities or disease. In this case, the patient underwent lesion curettage and bone grafting due to the risk of pathologic fracture.
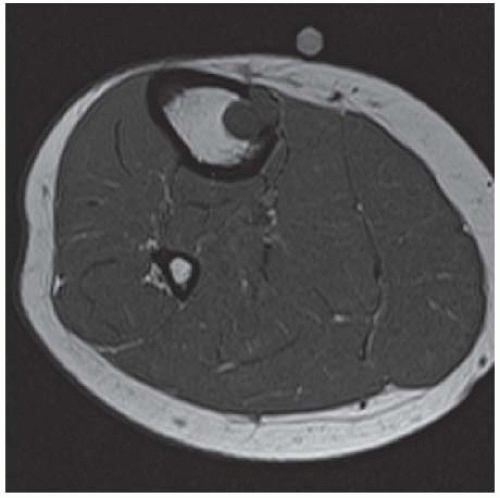
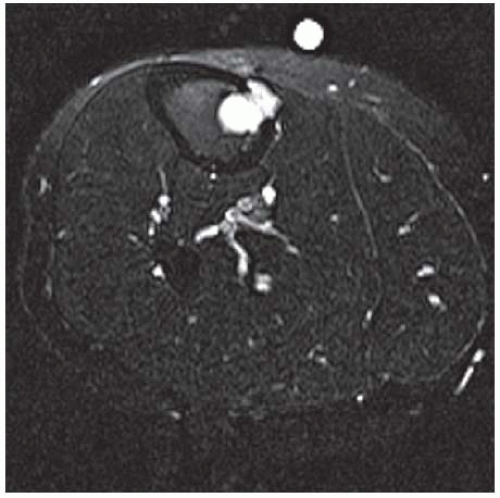
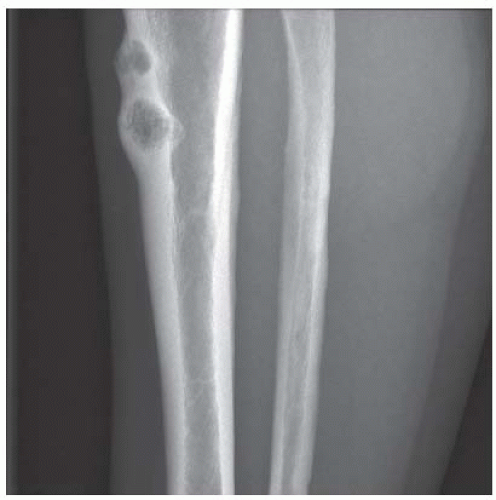
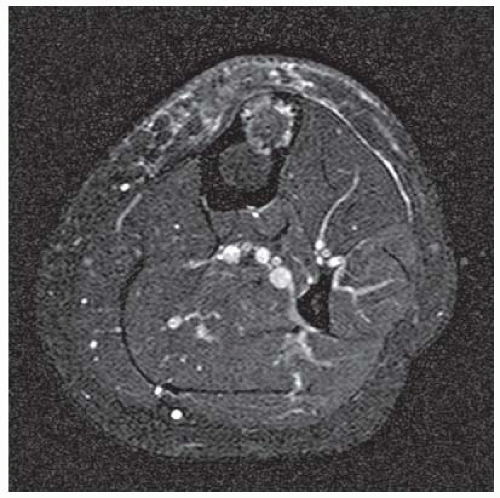
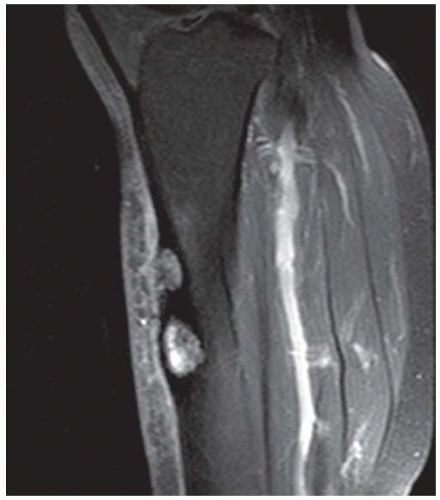
Case 7.9 Mazebraud syndrome
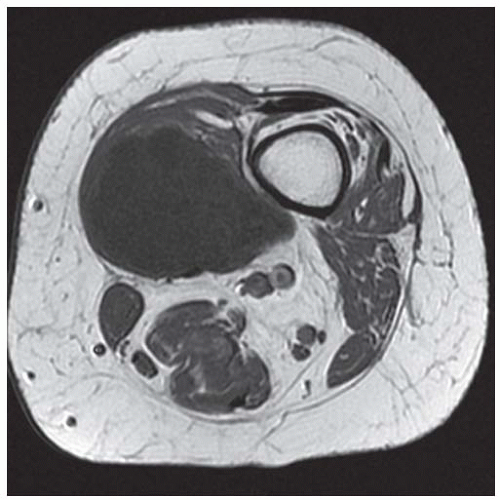
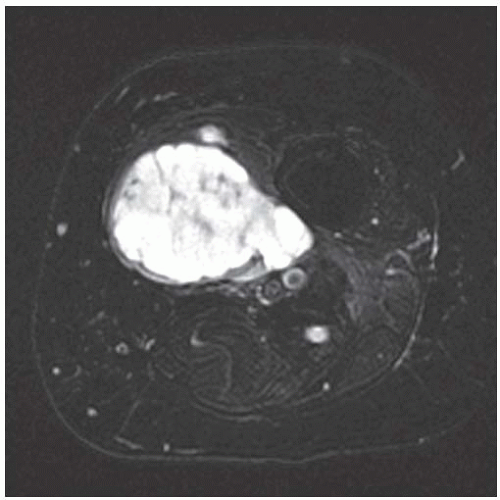
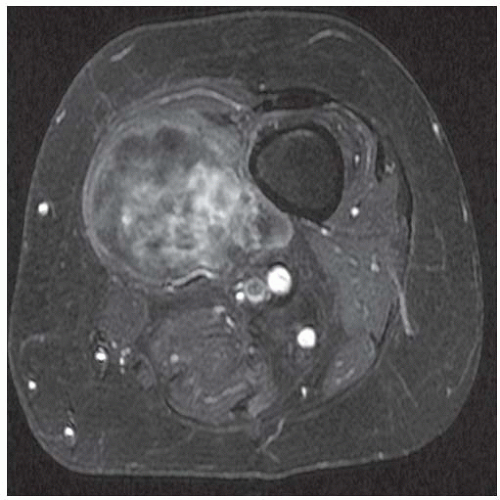
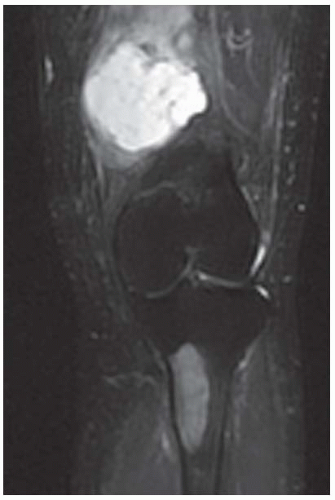
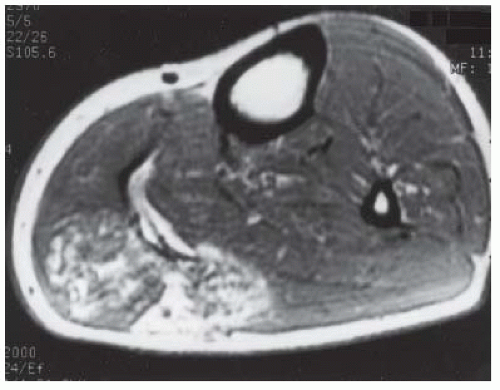
CLINICAL HISTORY A 75-year-old woman with thigh mass.
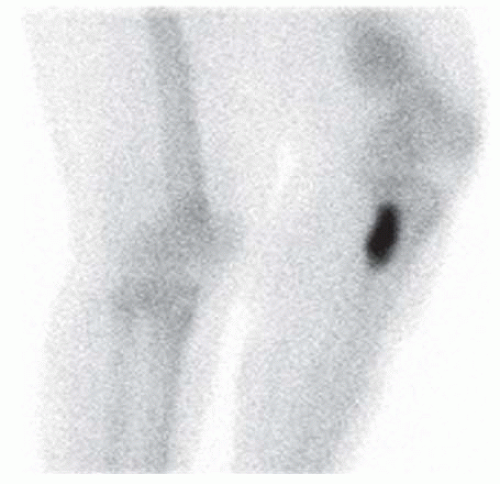
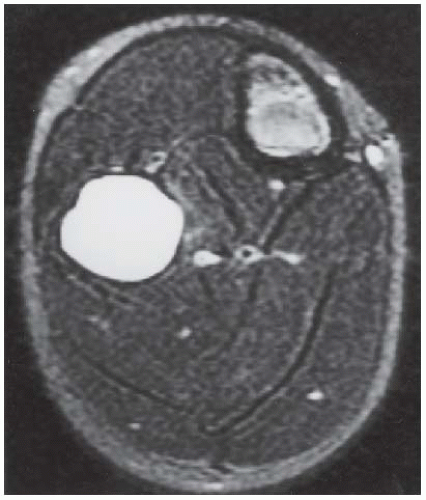
FINDINGS (A-C) Axial T1-weighted, T2-weighted, fatsuppressed, and postgadolinium T1-weighted, fat-suppressed MRI shows a lobulated mass in the distal vastus medialis. The mass shows high signal intensity on T2-weighted image and some internal contrast enhancement. Coronal inversion recovery MRI (D) shows the distal thigh mass and a welldefined intramedullary bony lesion in the proximal tibia that shows high signal intensity. Radiographs of the proximal tibia (E, F) demonstrate an ovoid lesion with ground-glass opacity and a thin sclerotic rim. (G) Bone scan (detailed view) shows increased uptake in the proximal tibia.
DIFFERENTIAL DIAGNOSIS Fibrous dysplasia with intramuscular myxoma, metastatic lesions involving bone and soft tissue.
DIAGNOSIS Mazabraud syndrome.
DISCUSSION Monostotic or polyostotic fibrous dysplasia associated with a single or multiple intramuscular myxomas is referred to as Mazabraud syndrome. Mazabraud syndrome is rare and does not appear to be hereditary. There is a high incidence of myxoma in close proximity to a focus of fibrous dysplasia. Of all the reported cases of Mazabraud syndrome, approximately 70% occurred in women, and 81% were polyostotic fibrous dysplasia [12]. The MR signal intensity of lesions in fibrous dysplasia is quite variable. On T2-weighted images, lesions are homogeneous to mildly heterogeneous, with about 60% of cases showing a signal intensity greater than that of fat. The remaining lesions will show either intermediate or low signal intensity on T2-weighted images. All lesions demonstrate decreased signal intensity on T1-weighted images. The diagnosis of fibrous dysplasia is readily confirmed on the corresponding radiograph [13]. Intramuscular myxoma shows low signal intensity relative to adjacent skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images. After administration of contrast material, heterogeneous enhancement is apparent with irregular rim enhancement. The degree of enhancement depends on the presence of solid myxoid and bridging fibrous septa at histologic examination. These features are unique and help differentiate myxoma from sarcoma [14].
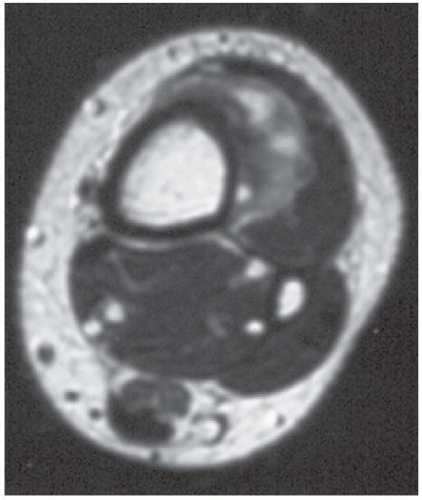
Case 7.10 Neurofibroma
CLINICAL HISTORY A 24-year-old woman with a painless soft tissue mass in the calf.
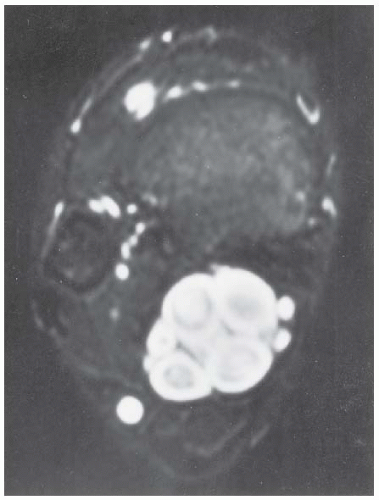
FINDINGS Axial T1-weighted (A) and T2-weighted (B) MRI shows a cluster of well-defined structures, demonstrating central relative hypointensity on T1 and T2 with rings of hyperintensity. Serial images establish the cylindrical nature of these structures.
DIFFERENTIAL DIAGNOSIS Neurofibroma or schwannoma.
DIAGNOSIS Neurofibroma.
DISCUSSION The ring-like morphology and central foci of hypointensity seen in this case are typical of peripheral nerve sheath tumors. In conjunction with the cylindrical nature of the lesion on long axis images, the diagnosis is likely to be neurofibroma. Most neurofibromas (90%) are solitary, slow-growing lesions found in young adults. The lesions may be superficial or deep and are usually painless. Because they are intimately associated with the underlying nerve, the patient may have dysesthesias. Because the lesion cannot be separated from the nerve, the nerve must be sacrificed at the time of surgical removal. MRI findings are often characteristic. The target appearance with a hyperintense rim and inner area of low signal intensity on T2 is typical of benign peripheral nerve tumors. It may be seen with either neurofibroma or schwannoma. Small foci of brighter signal intensity within the target area are said to represent thickened nerve bundles. This speckled appearance within a target lesion is characteristic of a peripheral nerve sheath tumor.
Case 7.11 Simple Bone Cyst
CLINICAL HISTORY A 16-year-old girl with leg swelling.
FINDINGS
A, B. Coronal T1-weighted MRI without and with gadolinium demonstrates T1 hypointensity and rim enhancement in a geographic, mildly expansile process of the proximal fibula diaphysis.
C. The T2 hyperintensity is homogeneous on the axial image. The lesion is central in transverse location.
DIFFERENTIAL DIAGNOSIS Simple bone cyst, aneurysmal bone cyst, fibrous dysplasia.
DIAGNOSIS Simple bone cyst.
DISCUSSION The diagnosis is made in conjunction with a plain radiograph (not shown). The expansile lesion in the metaphysis or diametaphysis is homogenous, with fluid signal characteristics and no aggressive features. There is no solid component and no septations within the lesion. The lesion has no mineralization within.
Case 7.12 Osteochondroma
CLINICAL HISTORY A 37-year-old woman with swelling, and a companion case.
FINDINGS
A. AP radiograph of the lower leg. There is an exostotic bony lesion arising from the medial tibial metaphysis. The cortex and marrow space of the lesion is contiguous with that of the underlying bone. Broadening of the proximal fibula represents another en plaque lesion.
B. Companion case. Lateral radiograph of the knee shows a pedunculated lesion arising from the posterior aspect of the proximal tibial cortex. The cortex and medullary space of the stalk are contiguous with the cortex and medullary space of the tibia.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Osteochondroma.
DISCUSSION The diagnosis in this case is made by recognizing that the lesion is composed of mature bone, with cortex and medullary space that is contiguous with the underlying bone. This osteochondroma has a coat-hook morphology, whereas the companion case has a more pedunculated cauliflower morphology. Osteochondromas (also called benign exostoses) are outgrowths of histologically normal bone that arise in the vicinity of a growth plate.
Case 7.13 Osteoblastoma
CLINICAL HISTORY A 5-year-old boy with anterior leg mass.
FINDINGS AP (A) and lateral (B) radiographs of the lower leg. There is an expansile lesion involving a long segment of the tibial diaphysis. The lesion has a hazy appearance and well-formed surrounding sclerosis. The lesion is somewhat asymmetric. There is no cortical penetration, periosteal reaction, or soft tissue mass.
DIFFERENTIAL DIAGNOSIS Fibrous dysplasia, osteoblastoma, adamantinoma, osteofibrous dysplasia.
DIAGNOSIS Osteoblastoma.
DISCUSSION A specific diagnosis is not possible in this case, but an expansile lesion with hazy mineralization in the tibial midshaft of a child brings up the differential of fibrous dysplasia and osteoblastoma. Other midshaft tibial lesions in children include adamantinoma and osteofibrous dysplasia (ossifying fibroma), both of which should have a more bubbly or multilocular appearance and are typically found in the cortex rather than the medullary space. Although osteoblastomas have a distinct predilection for the spine, of the approximately 30% that involve the long bones, the vast majority of these involve the lower extremities and are centered in the diaphysis. Most osteoblastomas are radiographically lucent, but mottled, stippled, or hazy ground-glass mineralization may be present. Osteoblastoma is unusual in children less than 5 years old, and there is a male predilection.
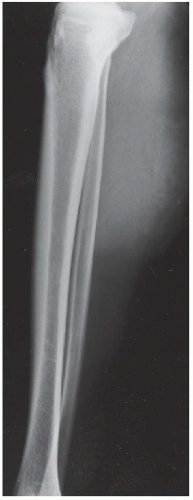
Case 7.14 Maisonneuve Fracture
CLINICAL HISTORY A 26-year-old intoxicated woman who fell down the stairs.
FINDINGS
Oblique radiograph of the ankle shows lateral dislocation of the talus and foot with disruption of the tibiofibular syndesmosis, and gross separation of the distal fibula from the tibia. A bone fragment representing the posterior malleolus is seen en face between the tibia and the fibula. The relationship of the talus to the lateral malleolus has been maintained. The displacement of the talus indicates that the deltoid ligament must be disrupted.
Oblique radiograph of the proximal leg shows a fracture of the proximal fibular shaft.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Maisonneuve fracture.
DISCUSSION A Maisonneuve fracture refers to an oblique fracture of the proximal fibular shaft that accompanies an injury at the ankle. The mechanism appears to be one of severe external rotation in which the talus and distal fibula are separated from the tibia, often accompanied by avulsion of the posterior malleolus by the strong posterior ankle ligaments, tear of the interosseous membrane, and either fracture of the medial malleolus or tear of the deltoid ligament [15]. In this case, the talus has dislocated laterally and become impacted against the lateral aspect of the tibia, but in the typical case, the talus relocates into the mortise on the rebound, reducing the posterior malleolar fragment. The Maisonneuve fracture may also be found in less severe external rotation injuries in which the lateral side of the ankle mortise is disrupted anteriorly but the posterior structures and the interosseous membrane remain intact [16].
Case 7.15 Nonossifying Fibroma (Fibrous Cortical Defect)
CLINICAL HISTORY An 18-year-old woman with knee pain.
FINDINGS AP (A) and lateral (B) radiographs of the knee show a well-defined, multiloculated, lucent lesion with sclerotic borders in the metadiaphysis. It is cortically based and eccentric, with extension into the medullary space. There is minimal expansion of the cortical surface.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Nonossifying fibroma (fibrous cortical defect).
DISCUSSION Nonossifying fibromas are histologically identical to fibrous cortical defects. Both are nonneoplastic proliferations of fibrous tissue and histiocytes that are selflimited and have no potential for growth or spread. Common radiologic usage of these terms refers to small, shallow, cortical lesions as fibrous cortical defects, and larger, multiloculated lesions as nonossifying fibromas. These lesions regress spontaneously, filling in with bone from the periphery and disappearing. The lesions are present at some time in perhaps one-third of all children. Fibrous cortical defects are seen mostly in children between 4 to 8 years old. Located on the cortical surface of the metaphysis at the attachment of a tendon or ligament, mostly around the knee, they produce a 1- to 4-cm scalloped defect in the underlying bone. They are round or oval, lucent, and sharply marginated by a sclerotic rim. Some have a bubbly appearance. Pathologic fractures may occur, but fibrous cortical defects are usually clinically silent. The distal femur, distal tibia, proximal tibia, and fibula are the reported locations for 90% of these lesions.
The lesion in this case has very indolent characteristics. The best way to estimate the rate of growth of a focal bone lesion is to evaluate the interface between the lesion and the host bone. The presence of a well-defined, thin, sclerotic rim of bone completely surrounding a lesion is indicative of a lesion whose rate of growth is slow enough to allow reactive osteoblastic activity. This rim of bone distributes biomechanical stress around the lesion and is typically better developed in weight-bearing bones. Lesions located in the diaphysis often do not have sclerotic margins, regardless of the growth rate.
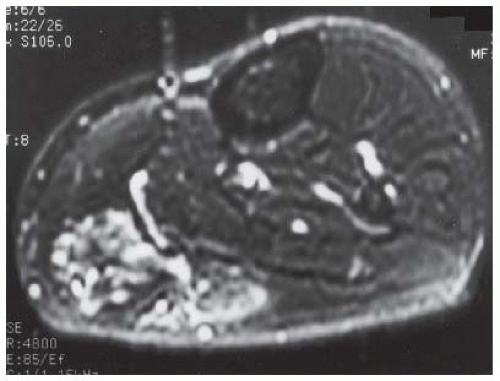
Case 7.16 Chondromyxoid Fibroma
CLINICAL HISTORY A 49-year-old woman with right tibial pain.
FINDINGS
A, B. AP (A) and lateral (B) radiographs of the knee demonstrate a geographic, eccentric lesion in the tibial diaphysis. There is a small area of cortical perforation medially.
C. Axial T1-weighted MRI shows lobulated low-signalintensity lesion extending through the medial cortex of the tibia into the soft tissue.
D. Axial T2-weighted, fat-suppressed MRI shows diffuse high signal intensity of the lesion.
E. Coronal T1-weighted, fat-suppressed MRI after intravenous gadolinium injection shows intense but peripheral contrast enhancement.
DIFFERENTIAL DIAGNOSIS Metastasis, chondromyxoid fibroma.
DIAGNOSIS Chondromyxoid fibroma.
DISCUSSION The diagnosis in this case is not easily made. Chondromyxoid fibroma is the rarest of all the cartilage tumors, and the imaging findings are nonspecific, so one should always expect to be wrong when proposing the diagnosis. The most common location for chondromyxoid fibroma is the proximal metaphysis of the tibia. The lesions are eccentric and often have a lobulated, well-defined margin. They have a sclerotic rim. Not infrequently, it also appears to erode through the cortex. A hemispherical defect appearing as a “bite” out of the bone has been described by some authors [17]. Cartilaginous matrix mineralization is not usually seen. Periosteal reaction is not a prominent feature. Internal characteristics of chondromyxoid fibroma on advanced imaging reflect the high water content of the lesion seen pathologically, with low attenuation on CT and low signal intensity on T1-weighted and very high signal intensity on T2-weighted MR images. Faint areas of calcification are unusual but are best appreciated by CT [18].
As the name indicates, histologically chondromyxoid fibroma is composed of a mixture of cartilaginous, myxoid, and fibrous elements. The lesion most commonly affects long bones, especially the tibia. In the Mayo Clinic series [19], chondromyxoid fibroma was the least common of the benign cartilage tumors, comprising only 3%, compared with 9% for chondroblastoma, 24% for chondroma (including enchondroma and periosteal chondroma), and 64% for osteochondroma.
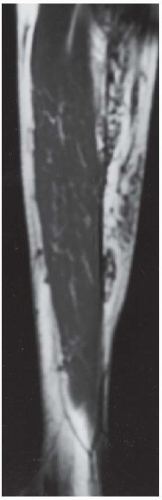
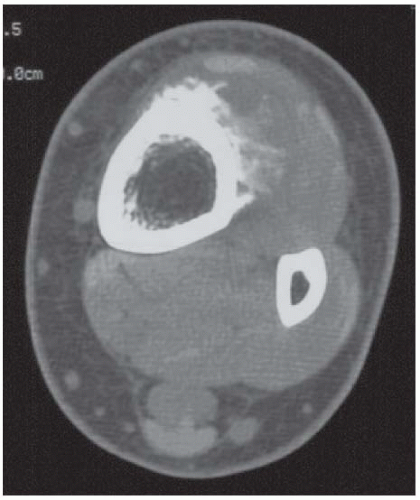
Case 7.17 Adamantinoma
CLINICAL HISTORY A 44-year-old woman who is an avid runner with left tibial pain with running.
FINDINGS Lateral and AP radiographs (A, B) and sagittal reconstructed CT (C) of left tibia show an anterior cortex lesion with two lucent regions and surrounding sclerosis.
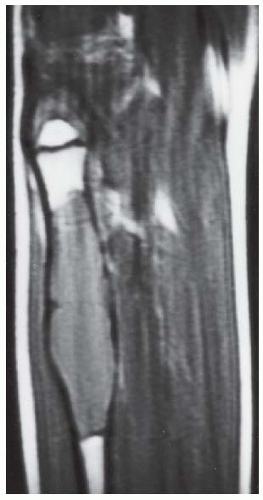
There is some coarse internal trabeculation without internal matrix mineralization on CT. Axial T1-weighted (D), short tau inversion recovery (STIR) (E), and sagittal postcontrast T1-weighted, fat-suppressed (F) MRI demonstrate low signal intensity on T1-weighted image and slightly heterogeneous iso-to-high signal intensity on STIR image. There is intense enhancement. The lesions are largely intracortical, but the inferior lesion does penetrate the medullary cavity, and the anterior cortex is also breached with subcutaneous edema. Intense radiotracer uptake is seen in the lesions on bone scan (G).
DIFFERENTIAL DIAGNOSIS Adamantinoma, ossifying fibroma, fibrous dysplasia.
DIAGNOSIS Adamantinoma.
DISCUSSION The radiologic diagnosis may be suggested by the particular location of the lesion in the anterior cortex of the tibia at the mid diaphysis. Adamantinomas are malignant tumors thought to be of angioblastic or epithelioid origin. There is a wide age spectrum, but it is most prevalent in the 2nd and 3rd decades and may have a slightly higher incidence in males. A striking feature of this neoplasm is its predilection for involvement of the midshaft of the tibia, which accounts for about 80% to 85% of all cases. Multifocal lesions may rarely develop in a single bone or in two or more bones [20,21]. The clinical course tends to be long, and most patients present with pain or swelling. The most common radiographic appearance is multiple, sharply circumscribed, lucent lesions of different sizes with surrounding sclerosis. Involvement of the bone is typically asymmetric, with the anterior tibial cortex virtually always the epicenter of the lesion. A relationship with ossifying fibroma has been postulated, because some regions of the tumors may have a histologic and radiologic resemblance. Whether ossifying fibroma represents a precursor to adamantinoma or whether it represents a reparative response is unknown; both possibilities have been suggested. The treatment of adamantinoma is surgical, but local recurrence, lymphatic metastases, and hematogenous metastases may occur.
Case 7.18 Hemangioma, Soft Tissue
CLINICAL HISTORY A 35-year-old man with intermittent swelling of the posterior calf.
FINDINGS
A. Lateral radiograph demonstrates soft tissue swelling with a few phleboliths. The region of abnormality shows mottled densities within fat and loss of the normal sharp demarcation between the subcutaneous fat and the superficial fascia.
B. Sagittal T1-weighted MRI demonstrates tubular structures with low signal intensity in a base of high signal intensity (fat).
C. Axial T2-weighted MRI shows tubular structures of high-intensity signal posteriorly.
D. Axial T1-weighted MRI after intravenous gadolinium injection shows enhancement of the lesion.
DIFFERENTIAL DIAGNOSIS Hemangioma, cellulitis.
DIAGNOSIS Hemangioma, soft tissue.
DISCUSSION Phleboliths within the soft tissue mass in the calf are suggestive of a vascular malformation. The MRI findings confirm the diagnosis. On T1-weighted MRI, hemangiomas characteristically have heterogenous signal intensity with some areas of fat-signal intensity. Low-intensity tubular structures of various sizes are usually evident. T2-weighted MRI shows fluid signal within the tubular structures, corresponding to sluggish blood flow. Hemangiomas may be classified histologically based on the predominant type of vascular channel [22]. The three main types are capillary, cavernous, and arteriovenous. The capillary type is most often found in the dermis or subcutaneous tissues, and typically does not undergo diagnostic imaging. The arteriovenous or venous types are rare. It is the cavernous type that often presents as a soft tissue mass requiring diagnostic imaging. Together, the classic radiographs and MRI findings are virtually diagnostic of cavernous hemangioma.
Case 7.19 Periosteal Osteosarcoma
CLINICAL HISTORY A 15-year-old cross-country runner with lower leg pain.
FINDINGS
A, B. Lateral and AP detail views of the lower tibia demonstrate a mass on the cortical surface of the distal tibia. There are lucent and sclerotic regions, with spicules of bone projecting away from the cortex into the soft tissues.
C. Axial CT with contrast enhancement shows the tumor mass extending from the cortical surface.
D. Axial T1-weighted MRI after gadolinium injection shows an enhancing mass apposed to an intact cortex, with low-signal regions within.
DIFFERENTIAL DIAGNOSIS Parosteal osteosarcoma, periosteal osteosarcoma, high-grade surface osteosarcoma, lymphoma, juxtacortical chondroma.
DIAGNOSIS Periosteal osteosarcoma.
DISCUSSION Osteosarcoma is an uncommon, malignant, bone-forming tumor with three commonly recognized but rare variants that arise on the cortical surface: parosteal osteosarcoma, periosteal osteosarcoma, and high-grade surface osteosarcoma [23]. Periosteal osteosarcomas comprise about 1.5% of all osteosarcomas. Usually found in the diaphysis of the femur or tibia, the peak age of discovery is about 20 years, and most patients present after a few weeks or months of pain, swelling, tenderness, or mass [24]. Periosteal osteosarcomas are moderately differentiated and chondroblastic, unlike the more common parosteal osteosarcomas, which are well differentiated and fibroblastic. The presence of any high-grade histologic features would cause the lesion to be classified as a high-grade surface osteosarcoma [25].
It is uncertain whether these surface osteosarcomas arise in the periosteum or in the outer layers of the cortex. On imaging, periosteal osteosarcomas appear as elongated, partially mineralized masses on the cortical surface of a long bone in the diaphyseal region, with thickened underlying cortex and solid periosteal reaction at the margins. Lucent regions within the tumor correspond to nonmineralized tumor cartilage, and brush-like spicules of bone extending from the underlying cortex into the tumor correspond mostly to trabeculae of reactive bone. Blotchy, punctate, and circular densities in the tumor represent mineralization of chondroid tumor matrix and reactive bone. The periphery of the lesion will have less mineralization. Periosteal osteosarcomas are much less dense radiographically than parosteal osteosarcomas, reflecting the difference in their histologic differentiation. Minimal involvement of the marrow space can be seen on CT or MRI [26]. Periosteal osteosarcomas are treated with wide excision. Their prognosis is better than that of high-grade intramedullary or high-grade surface osteosarcomas, but worse than parosteal osteosarcomas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree