FIGURE 2.1A

FIGURE 2.1B
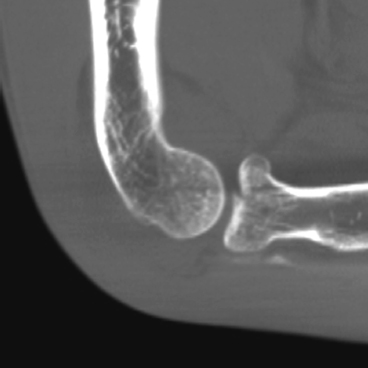
FIGURE 2.1C
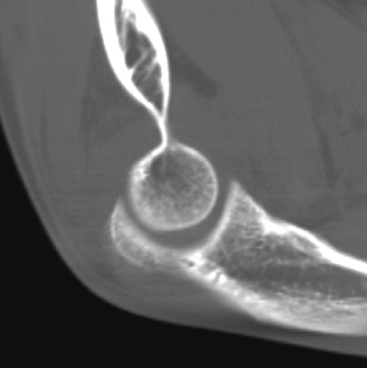
FIGURE 2.1D
FINDINGS
- Lateral radiograph shows elevated anterior and posterior fat pads, indicative of joint effusion. There is an intraarticular fracture of the radial head.
- Axial CT shows the fracture traversing the articular surface of the radial head.
- Sagittal CT reformation through the radiocapitellar joint shows slight depression of the radial head fragment.
- Sagittal CT reformation through the ulnar-trochlear joint shows the elevated anterior and posterior fat pads.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Radial head fracture.
DISCUSSION The fat pad sign at the elbow indicates an elbow effusion. Distention of the elbow capsule by fluid lifts up the anterior and posterior fat pads at the superior aspect of the elbow joint, displacing them from their normal positions and rendering them visible radiographically on the lateral view. The displaced anterior fat pad has been likened to a spinnaker sail, so the anterior fat pad is also called the “spinnaker sail sign.” A small portion of the anterior fat pad is normally visible as a thin, triangular radiolucency with a short base facing the elbow joint. The posterior fat pad is normally fully contained within the olecranon fossa and is not visible. In the setting of acute trauma, the fat pad sign is indicative of fracture, but an effusion from any cause may result in a fat pad sign. Radial head and neck fractures are sustained by younger adults during falls onto an outstretched hand, impacting the radial head against the capitellum. Two types of fractures result: the intra-articular radial head fracture, as in this case, and the radial neck fracture. Many radial head fractures may be treated by closed means or internal fixation, but comminuted displaced fractures have a high risk for osteonecrosis and resection with prosthetic implant may be performed [1].
CASE 2.2 CLINICAL HISTORY
An adult woman with deformity after a fall.

FIGURE 2.2A

FIGURE 2.2B
FINDINGS (A, B) AP and lateral radiographs of the elbow demonstrate lateral dislocation of the radius and displaced fractures of the middiaphysis of the ulna.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Monteggia fracture dislocation (Bado type III).
DISCUSSION A Monteggia fracture dislocation [2] is composed of a fracture of the ulna and a dislocation of the radial head. Various types are based on the site of the fracture and the associated direction of angulation and dislocation (Bado classification). The types are as follows: (I) proximal ulnar fracture with anterior angulation and anterior dislocation of the radial head (65%); (II) proximal ulnar fracture with posterior angulation and posterior dislocation of the radial head (18%); (IH) ulnar fracture just distal to coronoid process with lateral dislocation of the radial head (16%); and (IV) proximal ulnar fracture and fracture of the proximal radius distal to the bicipital tuberosity with anterior dislocation of the radial head (1%). This injury should be sought vigorously in adults with a demonstrated proximal ulnar shaft fracture. The radial head should intersect the capitellum on any view obtained. The radial nerve is damaged in 20% of cases, but most nerve injuries are transient.
CASE 2.3 CLINICAL HISTORY
A 2-year-old boy with upper limb deformity since birth.

FIGURE 2.3A

FIGURE 2.3B
FINDINGS (A, B) Lateral and oblique radiographs of the elbow. There is abnormal fusion of the proximal radius and ulna, with continuity of medullary space and cortical margins.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Radioulnar synostosis.
DISCUSSION Two types of radioulnar synostosis have been described [3]. This is a case of “true” or proximal synostosis, where there is smooth fusion along a 2- to 6-cm length of the proximal radius and ulna. The other type is typified by congenital dislocation of the radial head. Both types result from a failure of longitudinal segmentation of the proximal forearm, leading to bony or fibrous synostosis. Both types of synostosis may be bilateral in 60% of cases. Sporadic and familial forms are described, but sporadic forms are more common [4], Associated findings include clubfoot deformities, developmental dysplasia of the hip, thumb hypoplasia, Madelung’s deformity, and other segmentation anomalies (including carpal coalition and symphalangism). Associated syndromes include arthrogryposis, multiple hereditary exostoses, and Holt-Oram syndrome, to mention a few. Acquired synostosis can result from trauma, osteomyelitis, or Caffey disease. Before the osseous bridge is obvious, careful observation for the lateral radial bowing or ulnar tethering may help make an early diagnosis. Although some cases may be treated surgically, a longitudinal study of the natural history of congenital proximal radioulnar synostosis showed that most patients had few or no functional limitations, and were often employed in jobs that demanded extensive use of the forearm [5],
CASE 2.4 CLINICAL HISTORY
A 11-year-old boy in a mountain bike accident.
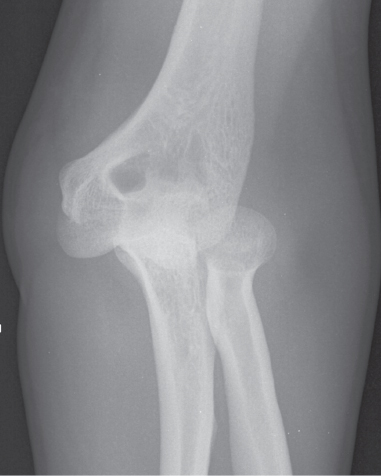
FIGURE 2.4A

FIGURE 2.4B
FINDINGS (A, B) AP and lateral radiographs of the elbow. Posterior dislocation of the elbow is present, without fractures.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Posterior elbow dislocation.
DISCUSSION The elbow is the most common site of dislocation in a skeletally immature patient and the third most common site of dislocation in an adult (after shoulder and interphalangeal dislocations). Acute dislocations of the elbow result from falls or sports-related mishaps, with the forces transmitted to a hyperextended elbow. Typically, the ulna dislocates posteriorly relative to the humerus, taking the radius with it. There are frequently no associated fractures, although the coronoid process and radial head in an adult and medial epicondyle in a child should be scrutinized. In children, both the medial epicondyle and the median nerve can become entrapped, preventing a closed reduction. Although posterior elbow dislocations are the most common, dislocation in other directions may occur. There is a rare variant known as a divergent dislocation, in which the radius and ulna separate in different directions. Recurrent dislocations imply instability, usually attributed to rapture of the medial collateral ligaments, avulsion of the brachialis attachment, damage to the anterior capsule, or some combination. Complications associated with elbow dislocations include compromise of the brachial artery, damage to the median or ulnar nerves, and heterotopic ossification (most commonly in the brachialis muscle, anterior to the elbow).
CASE 2.5 CLINICAL HISTORY
A 2-year-old child who refuses to move arm after a trip to the shopping mall.

FIGURE 2.5A
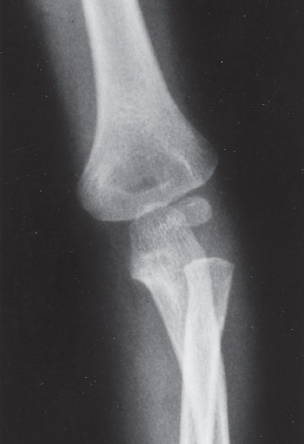
FIGURE 2.5B
FINDINGS
- A, B. AP and oblique radiographs of the left elbow demonstrate subtle subluxation of the radius with respect to the capitellum. A line drawn through the short segment of the radial shaft that is proximal to the radial tuberosity should intersect the center of the capitellum on all radiographic projections, but in this case it does not.
DIFFERENTIAL DIAGNOSIS Subluxation of the radial head, dislocation of the radial head, normal.
DIAGNOSIS Radial head subluxation.
DISCUSSION Subluxation of the radial head (nursemaid’s elbow, pulled elbow) is usually a temporary condition with spontaneous reduction. The usual history is a sudden pull on a forearm held in the pronated position, as might occur when a small child, who is being led by the hand by an adult, stumbles and falls. The adult will pull suddenly on the hand and forearm to prevent the child from striking the ground. The radial head slips under the lax annular ligament. Some authors state that the radiographs are normal, whereas other authors note that there may be subtle signs that indicate subluxation. If the radial head does not intersect the capitellum on all views, it is subluxated or dislocated [6]. The method of reduction involves a combination of flexion and supination (usually against an unhappy, resisting child). A palpable click is felt when the radial head relocates into its normal position. Offering a lollipop to the child and noting the ease of motion at the elbow joint can test the success of the maneuver. Occasionally, the annular ligament can become entrapped and prevent reduction [7]. The orthopedist will cast the child who fails to reduce or has a recurrent subluxation. Isolated radial head dislocation is a rare occurrence, limited to children. One is obligated to search for an associated fracture. Hereditary causes of radial head dislocation exist in, for example, the nail-patella syndrome, but are even more unusual than isolated dislocations. Injuries similar to pulled elbow have been described in adults [8,9].
CASE 2.6 CLINICAL HISTORY
A 5-year-old boy with elbow swelling. Radiographs at presentation and 4 months later.
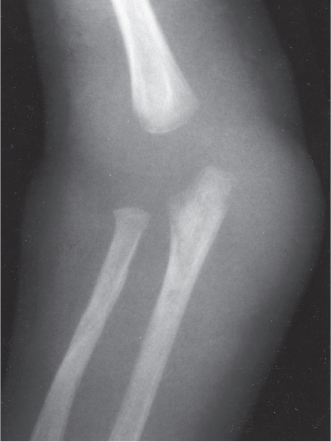
FIGURE 2.6A

FIGURE 2.6B
FINDINGS
- Oblique elbow radiograph at presentation reveals soft tissue swelling about the olecranon. Faint periosteal reaction is noted about the proximal olecranon metadiaphysis, and there is juxta-articular osteoporosis at the elbow joint.
- Oblique radiograph taken 4 months later demonstrates a marked increase in the periosteal reaction about the distal humerus and proximal ulna. Juxta-articular osteoporosis is still present and is most marked in the proximal olecranon.
DIFFERENTIAL DIAGNOSIS Septic joint, juvenile chronic arthritis, trauma, Lyme arthritis.
DIAGNOSIS Septic elbow joint.
DISCUSSION The recovery of an organism from the joint is the only reliable method for distinguishing a septic elbow joint from an aseptic joint. Examples of conditions associated with aseptic monoarticular inflammatory arthritis include rheumatic fever, hepatitis, and reactive arthritis. These immunologic entities commonly occur 2 to 3 weeks after the initial symptoms. Similarly, sterile synovitis can occur secondary to an inflammatory process in the adjacent bone or bursa. Potential sources of infection include the blood, adjacent bones or soft tissues, and direct penetration (accidental or iatrogenic). The classic radiologic sequence of events is as follows: joint effusion and soft tissue swelling (edema and hypertrophy of synovium, with leaky membranes), osteoporosis (hyperemia), joint space loss (chondral loss from inflamed pannus), marginal and central erosions (osseous destruction from inflamed pannus), sclerotic host bone formation (periostitis in this case), and late bony ankylosis (either fibrous or true osseous ankylosis). Bacterial septic arthritis is usually due to Staphylococcus aureus or a streptococcus species. In children, Haemophilus influenzae is an important causative organism. Polyarticular involvement is usually secondary to encapsulated organisms such as pneumococcus or H. influenzae.
When septic arthritis is secondary to tuberculosis or fungi, the radiographic findings differ in that there is little or no reparative bone, and the process is more indolent in nature. The hips and knees are more commonly involved than the wrist and elbow. Complications include synovial cyst formation, soft tissue and tendon injury (especially rotator cuff rupture in the shoulder) or abscesses, osteomyelitis, ankylosis, overgrowth of epiphyses from regional hyperemia (if physes are still open), and osteoarthritis.
CASE 2.7 CLINICAL HISTORY
A 70-year-old man with painful swelling over the elbow for several days.
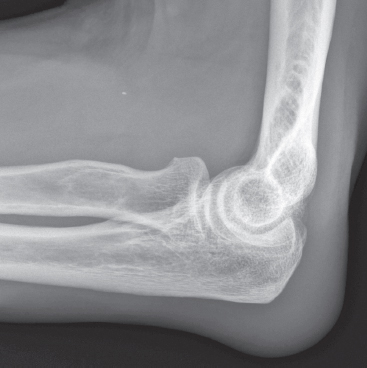
FIGURE 2.7A
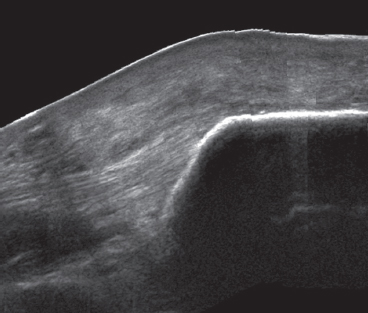
FIGURE 2.7B
FINDINGS
- Lateral radiograph of the elbow shows focal soft tissue swelling over the olecranon process. There is no soft tissue calcification and there are no changes in the underlying bone.
- Longitudinal sonogram with the transducer over the region of swelling shows a collection with heterogeneous echotexture and small central anechoic region. There are no calcifications. Color Doppler (not shown) revealed internal flow.
DIFFERENTIAL DIAGNOSIS Olecranon bursitis, septic or nonseptic; rheumatoid arthritis.
DIAGNOSIS Septic olecranon bursitis.
DISCUSSION Olecranon bursitis is a common lesion [10]. Beyond location, the imaging appearance is nonspecific, and aspiration with culture and gram stain may be required for definitive diagnosis. However, patients with septic bursitis may have systemic features of infection and tend to present earlier and with more severe symptoms than patients with non-septic bursitis. If calcification is present, tophaceous gout is a strong consideration. Patients with rheumatoid arthritis are also predisposed to developing olecranon bursitis. Swelling of the olecranon bursa may also follow falls onto the elbow, and if accompanied by an open injury, infection may follow.
CASE 2.8 CLINICAL HISTORY
A 29-year-old burn victim with stiff elbow joint.

FIGURE 2.8A

FIGURE 2.8B
FINDINGS (A, B) AP and lateral elbow radiographs show extensive soft tissue ossification at the elbow, enveloping the elbow joint. Flexion and extension at the elbow joint are severely limited. The overlying surgical staples indicate sites of skin grafting.
DIFFERENTIAL DIAGNOSIS Posttraumatic changes, thermal injury, collagen vascular disease.
DIAGNOSIS Heterotopic ossification after burns.
DISCUSSION Thermal burns cause coagulative tissue necrosis. The depth of the injury is related to the severity and duration of the applied heat. Initially, one can see soft tissue loss and soft tissue edema. Osteoporosis (30% of cases) may be localized or diffuse, and is explained on the basis of hyperemia, reflex sympathetic response, or alteration in local metabolism. Periostitis may also occur in the weeks that follow, and is thought to be secondary to a local periosteal irritation. Periarticular osseous excrescences, osteophytes, or soft tissue calcification or ossification (23% of cases) are common after extensive burns, and may be seen 2 to 3 months after injury [11,12]. They typically occur in adults along the preexisting connective tissue framework, most commonly around the elbow. The range of motion of involved joints will be limited mechanically. The exact pathogenesis of these ossifications is unknown and does not seem to correlate with the severity of the burn. The hyperemic response seen with burns can elicit bone growth. Contractures are most common about the elbow and within the hand. Articular abnormalities can be local or remote and result from hyperemia, compression, infection, or thermal injury. Differential considerations of ankylosis from heterotopic ossification include posttraumatic [13], neurogenic, and other etiologies [14].
CASE 2.9 CLINICAL HISTORY
A 6-year-old girl who fell

FIGURE 2.9
FINDINGS Lateral elbow radiograph. Anterior and posterior fat pad signs are prominent. There is slight posterior angulation of the distal humerus. A line drawn along the anterior cortex of the humerus (anterior humeral line) should intersect the capitellum in its posterior third, but in this case, the line intersects the capitellum in its anterior third. An actual fracture line is not visible on this radiograph.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Supracondylar fracture.
DISCUSSION The fat pad sign is the clue to the presence of a fracture about the elbow. More than 90% of children or adolescents with a posterior fat pad sign will have a demonstrable fracture, and absence of the fat pad sign in these age groups virtually excludes an intra-articular fracture, unless the injury is so severe that there is disruption of the elbow joint capsule. The supracondylar fracture constitutes 60% of fractures around the elbow in children. Radial head and neck fractures, common in adults, are generally not seen in children. Supracondylar fractures occur with hyperextension of the elbow, usually from a fall. The fracture extends transversely across the distal humerus through the coronoid and olecranon fossae, above the level of the condyles. The distal fragment is angulated posteriorly, so that the anterior humeral line passes anterior to the capitellum. A posterior fat pad sign is almost always present. The fracture is usually complete, but green-stick fractures, torus fractures, or plastic bowing are possible. The typical treatment is closed reduction with casting.
CASE 2.10 CLINICAL HISTORY
An 8-year-old little league pitcher with right elbow pain. Radiographs of right and left elbows.

FIGURE 2.10A

FIGURE 2.10B
FINDINGS
- AP radiograph of the right elbow (symptomatic). There is an irregular horizontal lucent defect through the ossification center of the capitellum.
- Radiograph of the left elbow (asymptomatic) is normal.
DIFFERENTIAL DIAGNOSIS Osteochondrosis of the capitellum, osteochondntis dissecans, acute trauma.
DIAGNOSIS Osteochondrosis of the capitellum.
DISCUSSION Osteochondrosis of the capitellum, or Panner disease, is better known as “little leaguer’s elbow.” The condition is an osteochondrosis of the humeral capitellum that is seen principally in boys between the ages of 5 and 10 years. An osteochondrosis is a general term that has come to refer to the condition resulting from ischemia of a growing epiphysis. The capitellum is the rounded protuberance at the distal humerus that articulates with the proximal radius and is covered with articular cartilage. The blood supply enters from its posterior aspect and is vulnerable to traumatic disruption by indirect repetitive valgus stress or direct compression, sometimes leading to vascular compromise. Although most lesions revascularize and heal without consequence, deformity, bony resorption, or frank fragmentation of the capitellum may occur. Pain and stiffness may limit full extension of the elbow, and a commonly associated clinical finding is joint swelling from effusion and/or synovial hypertrophy. Radiographic findings at the capitellum include the crescentic fissure through the ossification center (as noted in this case), increased density, decreased size, resorption, or frank fragmentation. Hyperemia may lead to premature maturation of the radial head. Unilateral involvement is noted in the throwing arm of little league baseball players, and the condition has also been noted in gymnasts. The main differential consideration is osteochondntis dissecans, a traumatic osteochondral injury seen in an older age group, after the capitellum has essentially stopped growing [15]. Computed tomography (CT) or magnetic resonance imaging (MRI) may be helpful when there is a question of fragmentation.
CASE 2.11 CLINICAL HISTORY
A 7-year-old boy with trauma.
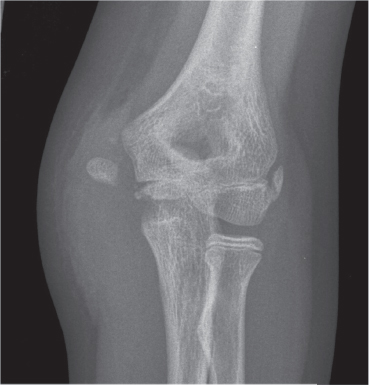
FIGURE 2.11A

FIGURE 2.11B
FINDINGS
- AP elbow radiograph shows that the medial epicondyle has been avulsed from the distal humerus, with the fracture plane passing through the apophyseal plate. Soft tissue swelling is present at the site.
- Lateral elbow radiograph does not show a fat pad sign.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Medial epicondyle avulsion fracture (Salter type I).
DISCUSSION The medial epicondylar ossification center appears around the age of 5 years. It is the site of origin of the common tendon of the flexor pronator muscle group, and can be avulsed by muscular contraction. This often results in a fracture fragment that is displaced distally or anteriorly. Medial epicondylar injuries are usually seen in the 5-to-15-year age group; after the medial epicondyle fuses in late adolescence, this injury no longer occurs. Medial epicondylar injuries are far more common than lateral epicondyle injuries. An important association to recognize with medial epicondylar injury is damage to the ulnar nerve as it passes the elbow. Injury of the ulnar nerve may result in motor weakness of the flexor carpi ulnaris, flexor digitorum profundus muscle of the fourth and fifth fingers, and intrinsic hand muscles of the fourth and fifth digits, as well as sensory deficits of the fourth and fifth fingers.
CASE 2.12 CLINICAL HISTORY
A 9-year-old boy with trauma.

FIGURE 2.12A
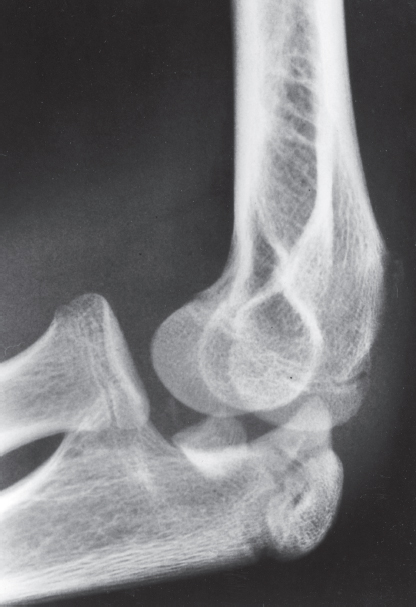
FIGURE 2.12B
FINDINGS (A, B) AP and lateral elbow radiographs. The medial epicondyle has been avulsed from the distal humerus during posterior dislocation of the elbow. The fracture plane passes through the apophyseal plate, and the fragment has interposed itself between the trochlea and ulna, preventing reduction of the dislocation.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Posterior elbow dislocation with entrapped medial epicondyle.
DISCUSSION Dislocation of the elbow may separate the medial epicondyle from the distal humerus by stress applied through the medial ulnar collateral ligament (UCL). The medial epicondylar fragment may then become entrapped in the elbow joint as it opens with valgus stress, requiring surgical reduction. For review, the order of ossification of the epiphyses and apophyses of the elbow can be remembered by the mnemonic CRITOE: Capitellum (less than 1 year), Radial head (5 years), Internal humeral epicondyle (7 years), Trochlea (10 years), Olecranon (10 years), and External humeral epicondyle (12 years). The age at which these centers begin to ossify is variable, but the order in which they close is generally not.
CASE 2.13 CLINICAL HISTORY
A 57-year-old woman with pain at the lateral aspect of the elbow.
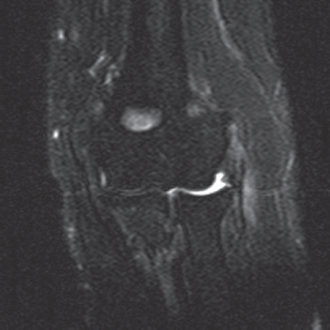
FIGURE 2.13A
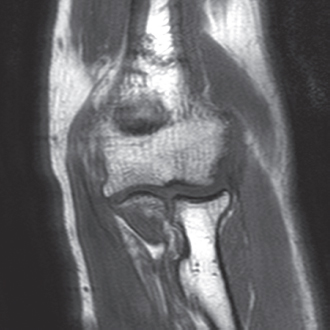
FIGURE 2.13B
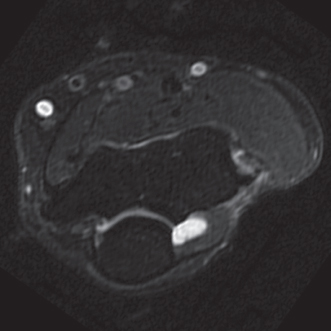
FIGURE 2.13C
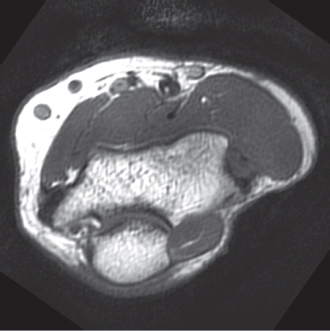
FIGURE 2.13D
FINDINGS Coronal (A) and axial (C) T2-weighted fat-suppressed and coronal (B) and axial (D) Tl-weighted MRI of the elbow show increased signal and thickening within the normally very low signal intensity common extensor tendon.
DIFFERENTIAL DIAGNOSIS Common extensor tendon full-thickness tear, lateral epicondylitis.
DIAGNOSIS Lateral epicondylitis.
DISCUSSION Lateral epicondylitis presents as lateral elbow pain that has an insidious onset, beginning gradually after vigorous activity and progressing to pain with activity. Radiographs are frequently normal, although some patients may have evidence of a spur at the lateral epicondyle or calcification of the common extensor tendon. MRI is useful in assessing the degree of tendon damage and associated ligament abnormality. Increased Tl-weighted and T2-weighted signal is seen within the tendon with epicondylitis. The tendon is usually thickened, and edema can be present in the adjacent soft tissues. Using both the axial and coronal planes is helpful in assessing these lateral tendons. Additionally, MRI is useful in evaluating additional structures that may explain the lack of response to therapy (e.g., ligamentous injury) [16]. Ultrasonography may also be used to assess for epicondylitis, although it has been found to be less specific than MRI [17].
CASE 2.14 CLINICAL HISTORY
A 21-year-old college baseball player with medial elbow pain.
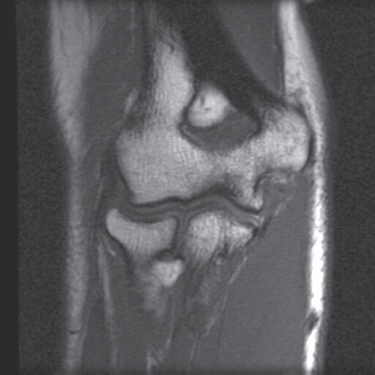
FIGURE 2.14A
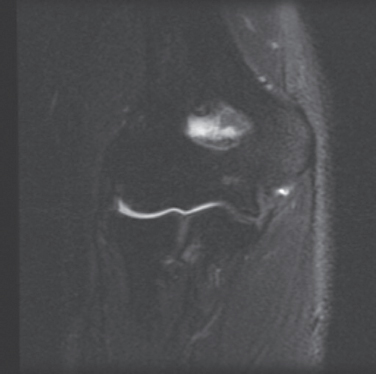
FIGURE 2.14B
FINDINGS
- Coronal Tl-weighted MRI shows globular signal isointense to muscle at the expected humeral origin of the UCL. The distal portion of the ligament may be seen as a dark, linear structure attaching to the ulna. The overlying common flexor tendon origin is intact at the medial epicondyle.
- Coronal T2-weighted fat-suppressed MRI shows high signal where the UCL is torn at its proximal origin.
DIFFERENTIAL DIAGNOSIS UCL tear, medial epicondylitis.
DIAGNOSIS UCL tear.
DISCUSSION The ulnar collateral ligament (UCL, also called medial collateral ligament) originates from the inferior aspect of the medial epicondyle, deep to the common flexor tendon origin, and does not have an attachment to the adjacent medial condyle. The UCL has an important anterior band that inserts at the sublime tubercle at the medial aspect of the coronoid process and a clinically less important posterior band that inserts along the supinator crest at the lateral aspect of the ulna. Tears of the UCL typically result from repetitive valgus stress, as may occur with pitching a baseball overhand, and may involve the proximal origin, the mid-substance, or the distal insertion. Avulsion fractures of the sublime tubercle may occur through the same mechanism. A tear of the UCL is a much more common injury than medial epicondylitis.
CASE 2.15 CLINICAL HISTORY
A 33-year-old man with posterior elbow injury.
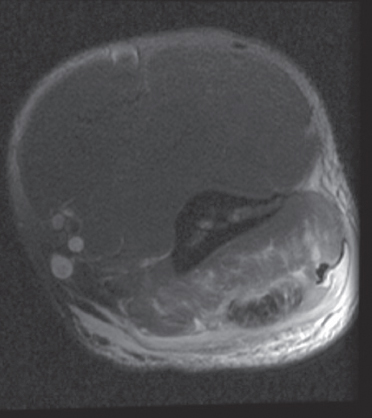
FIGURE 2.15A
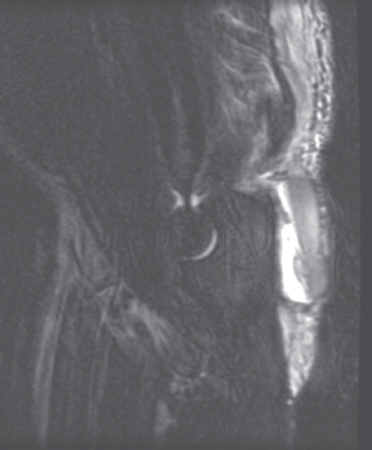
FIGURE 2.15B
FINDINGS
- Axial proton-density fat-suppressed MRI shows high signal in the triceps compartment, corresponding to edema and hemorrhage in and around the posterior aspect of the muscle. The triceps tendon is thickened and has high signal within it.
- Sagittal T2-weighted fat-suppressed MRI shows retraction of the triceps tendon, and surrounding edema and hemorrhage. The muscular portion of the triceps insertion has some high signal, but is not detached. Hemorrhage also involves olecranon bursa, with a hematocrit effect.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Triceps tendon tear with olecranon bursa hemorrhage.
DISCUSSION Triceps tendon ruptures are uncommon injuries caused by decelerating counterforce during active extension of the elbow. These injuries are seen mostly in participants of sports that require upper body strength training. Although tears at the musculotendinous junction may occur, in most cases there is a catastrophic failure at the distal insertion. Distal triceps tears are frequently associated with avulsion fractures at the olecranon. On MRI, the detachment of the tendon can be seen directly, with proximal retraction that is best demonstrated on sagittal images. Surrounding hemorrhage and edema will be seen in acute injuries, but clinical diagnosis in the acute phase may be challenging, and many patients will not be imaged until the injuries are subacute or chronic. Treatment in most cases will be surgical repair.
CASE 2.16 CLINICAL HISTORY
A 45-year-old woman with elbow pain following a fall.

FIGURE 2.16A
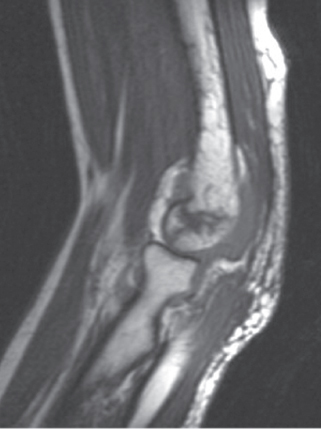
FIGURE 2.16B
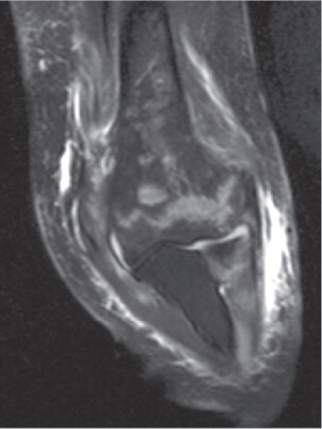
FIGURE 2.16C
FINDINGS
- Lateral radiograph of the elbow shows anterior and posterior fat pad signs. No fracture was visualized on the AP and oblique views.
- Sagittal T1-weighted MRI shows a complex intra-articular fracture involving the capitellum. An effusion lifting up the posterior fat pad can be seen.
- Coronal T2-weighted fat-saturated MRI shows a jagged fracture line traversing the distal humerus, from epicondyle to epicondyle.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Occult distal humerus fracture.
DISCUSSION The value of the fat pad sign in identifying patients with elbow fractures has been proven time and again, but it is not perfect. In a recent study, 20 adult elbow trauma cases, with positive fat pad signs but no identified fractures, underwent MRI scans within 0 to 12 days [18]. The authors found that 75% of their patients had identifiable fractures, mostly involving the radial head, but they also noted that actual management was not changed by the additional information in any of the cases. The issues raised by studies like this have been discussed in an editorial by Rogers [19]. If the cost and convenience of MRI in the acute setting were the same as that of radiography, it would clearly be the diagnostic modality of choice, and although management might not change, the diagnostic certainty would have some value to patients and their families, physicians and other providers, insurance companies and other payors, and so forth. Thus, Rogers argues that cost and convenience are the true barriers to the better diagnosis of musculoskeletal trauma.
CASE 2.17 CLINICAL HISTORY
A 75-year-old man with injury sustained while pulling cactus out of his yard.
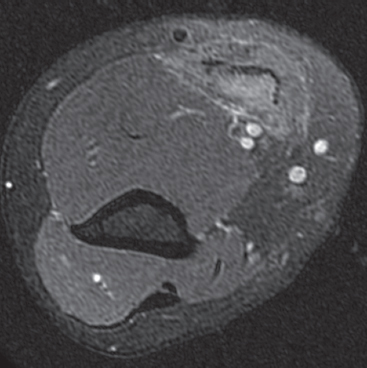
FIGURE 2.17A
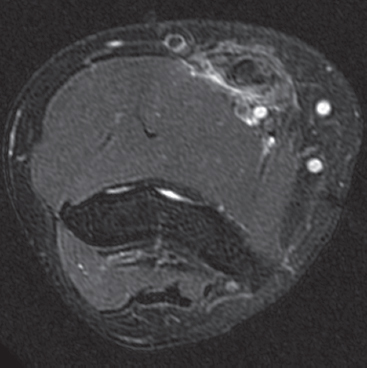
FIGURE 2.17B
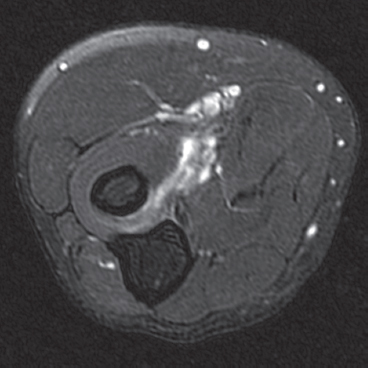
FIGURE 2.17C
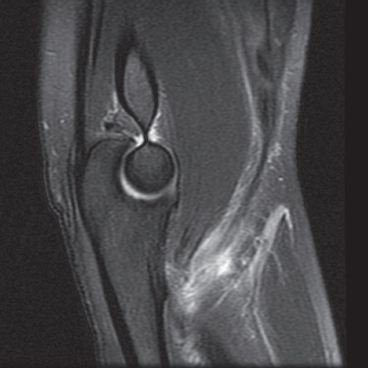
FIGURE 2.17D
FINDINGS
- Axial STIR MRI at the level of the distal humeral shaft shows swelling of the biceps muscle with high signal in the muscle and tendon.
- Axial STIR MRI at the level of the humeral condyles shows a retracted biceps tendon with thickening and high signal.
- Axial STIR MRI at the level of the bicipetal tuberosity of the radius shows absence of the biceps tendon with high signal tracking along its expected course.
- Sagittal proton density MRI with fat-suppression shows the retracted biceps tendon and muscle belly.
DIFFERENTIAL DIAGNOSIS High-grade partial-thickness or full-thickness tear of the biceps tendon.
DIAGNOSIS Complete biceps tendon rupture.
DISCUSSION Biceps tendon tears occur during flexion against strong resistance. These are most commonly seen in the dominant arm of middle-aged males who smoke tobacco [20]. The complete tear typically occurs at its insertion at the bicipital tuberosity of the proximal radius. In complete tears, proximal retraction of the tendon by muscle action results in a mass or bulbous swelling of the proximal arm; swelling at the distal arm may be minimal because of the tense antecubital fascia. Degenerative thickening of the biceps tendon may be present. MRI of complete biceps tendon ruptures will always show the absence of the tendon distally and nearly always shows a fluid-filled tendon sheath. Less common findings include an antecubital fossa mass, muscle edema, and atrophy [21]. Partial tears show high signal intensity within the tendon, fluid in the biceps tendon sheath, and thinning or thickening of the distal tendon, but the tendon will remain in continuity with its insertion. Biceps tendon ruptures are treated surgically, but some loss of function, particularly with activities requiring repetitive supination, is common [22].
CASE 2.18 CLINICAL HISTORY
A 45-year-old woman with progressive difficulty in rotating her shoulder after an injury. She had previously undergone surgical repair of her rotator cuff.
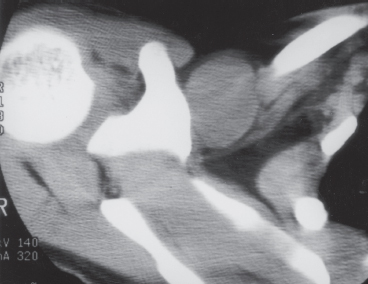
FIGURE 2.18A
FIGURE 2.18B
FIGURE 2.18C
FIGURE 2.18D
FINDINGS
- A. Axial CT scan (soft tissue windows) shows a globular 3-cm mass, isodense to muscle, in the infraclavicular region, medial to the coracoid process. The lesion is not calcified.
- B. Axial T2-weighted MRI demonstrates the rounded lesion located medial to the coracoid process and inferior to the clavicle. The lesion has high signal intensity.
- C, D. Coronal T1-weighted MRI before and after intravenous injection of gadolinium shows avid enhancement in the lesion. The abnormal appearance of the epiphysis is related to prior surgery.
DIFFERENTIAL DIAGNOSIS Ganglion cyst, fibromatosis, postsurgical scarring, soft tissue sarcoma.
DIAGNOSIS Fibromatosis (extra-abdominal desmoid tumor).
DISCUSSION Fibromatosis is a neoplastic process that arises in fascial and musculoaponeurotic coverings, sometimes at a site of previous trauma or surgery [23]. Described initially in the abdominal wall, it is commonly divided into superficial and deep forms [24]. Deep forms include extra-abdominal, abdominal, and intra-abdominal, which refer to their location relative to the abdominal wall. The extra-abdominal form of deep fibromatosis is of concern in this case. The age of peak incidence is between 25 and 35 years, and there is no clear sex predominance. The tumors are usually solitary, but as many as 15% of patients have synchronous multicentric lesions in the same extremity. Commonly involved sites include the shoulder area, upper arm, thigh, neck, pelvis, forearm, and popliteal fossa, in decreasing order of prevalence. Fibromatosis is nonencapsulated and has an infiltrative growth pattern that may be locally invasive. Lesions may grow to large size and become adherent to adjacent structures such as bone or neurovascular bundles. Fibromatosis is composed of well-differentiated fibroblasts embedded in an abundant collagenous matrix. Because of variable degrees of cellularity, matrix water content, and infiltration, attenuation on CT scans and signal intensity on MRI may be variable [25]. Enhancement may be heterogeneous. Associated osseous findings can include periostitis and pressure erosion. Treatment is surgical resection, but local recurrence is frequent unless wide margins can be obtained.
CASE 2.19 CLINICAL HISTORY
An 11-year-old boy with lumpy arm.

FIGURE 2.19A

FIGURE 2.19B
FIGURE 2.19C
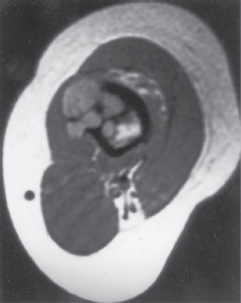
FIGURE 2.19D
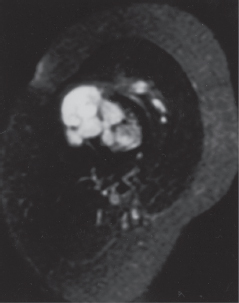
FIGURE 2.19E
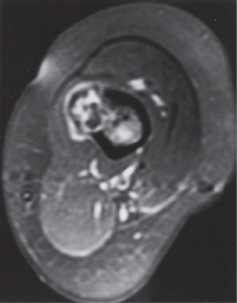
FIGURE 2.19F
FINDINGS
- A, B. AP and lateral radiographs demonstrate a cortically based lesion at the humeral diaphysis. The lesion involves the posterolateral cortex and is characterized by lobulated lucency surrounded by thickened cortex.
- C. Axial CT image shows the marked cortical thickening associated with the sessile, cortically based lesion. A lower-density soft tissue component surrounds the thickened cortex.
- D, E. Axial T1-weighted and axial T2-weighted MRI shows T1 hypointensity and T2 hyperintensity within the lobules of the lesion. The bulk of the lesion is on the cortical surface, but a portion of it projects into the medullary space.
- F. Axial T1-weighted MRI obtained after gadolinium injection shows enhancement of portions of the lesion.
DIFFERENTIAL DIAGNOSIS Juxtacortical (periosteal) chondroma, chondrosarcoma, osteochondroma, surface osteosarcoma, posttraumatic deformity, aneurysmal bone cyst.
DIAGNOSIS Juxtacortical chondroma.
DISCUSSION Juxtacortical (periosteal) chondroma is a benign, cortically based cartilage lesion that is similar to an enchondroma except for its location on the surface of bone [26]. The lesions consist of mature cartilage, and they are covered with periosteum. On pathologic examination, juxta-cortical chondroma can be more cellular than enchondroma and contain double-nucleated chondrocytes, which can lead to a diagnosis of a low-grade chondrosarcoma if the findings are not correlated with the benign radiologic appearance [27]. Most lesions are found in adolescents or young adults, with a male predominance [28]. The most common sites are the proximal humerus and femur, with two-thirds of lesions involving the metaphysis and the remainder involving the diaphysis. The presenting symptom is usually pain and/or swelling, but many juxtacortical chondromas are discovered incidentally on radiographs obtained for other reasons. The radiographic appearance of a calcified soft tissue mass eroding the associated cortex is classic. Solid periosteal bone formation at the margins of the lesion may produce buttresses and form a cup-like appearance. Calcification of matrix is seen in only one-half of cases and, therefore, need not be present for the diagnosis. Markedly elongated lesions with irregular cortical thickening are not atypical. Reactive medullary sclerosis and periostitis can be identified, and do not necessarily imply malignant degeneration or pathologic fracture; these features are probably a response to the peripheral vascularity. MRI is useful to show the lobulated morphology and T2 hyperintensity that is characteristic of chondroid lesions. Size greater than 4 cm, medullary involvement, cortical destruction, and an associated soft tissue mass are features suggestive of chondrosarcoma. Treatment is surgical, and lesions should not recur.
CASE 2.20 CLINICAL HISTORY
A 74-year-old man with shoulder pain.
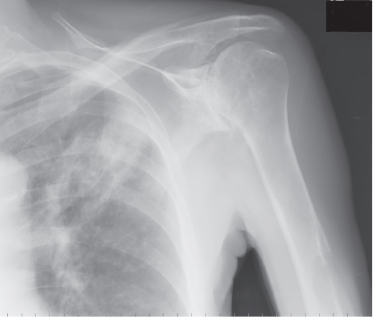
FIGURE 2.20A

FIGURE 2.20B

FIGURE 2.20C
FINDINGS
- A, B. AP (A) and axillary (B) radiographs of the left shoulder show a large mass in the left lung apex, and a lytic lesion in the midhumeral shaft. The humeral lesion is centered in the cortex and has provoked little, if any, reactive bone formation. Incidental degenerative changes at the glenohumeral joint are advanced.
- C. Radionuclide bone scan demonstrates abnormal radio-tracer uptake within the midshaft of the left humerus, right iliac crest, and right acetabulum, which is suspicious for bone metastasis. Increased uptake within the shoulder joints is related to osteoarthritis.
DIFFERENTIAL DIAGNOSIS Metastases, myeloma, lymphoma.
DIAGNOSIS Lung cancer metastasis, with pathologic fracture.
DISCUSSION Pathologic fractures through bones involved by metastases are common. The most common sites of pathologic fracture are the vertebral bodies, ribs, proximal femur, and proximal humerus. Metastases of lytic, blastic, and mixed radiographic appearance all cause weakening of the bone.
In the long bones, destructive lesions with full-thickness cortical penetration lead to pathologic fractures. Gaps in the cortex weaken the bone by causing uneven and aberrant distribution of the stresses of loading, impeding the normal biomechanical dispersion of force. Weakening is gradual as cortical bone is infiltrated, eroded, and destroyed. Blastic lesions also destroy cortex, and the reactive and the stromal bone that gives blastic lesions their radiodensity is structurally unsound. The bone may fracture under the stresses of normal activity. Cortical weakening makes bone most vulnerable to tensile forces; therefore, in the long bones, pathologic fractures are usually transverse. The onset of pain at a site of metastatic involvement may indicate the presence of microfractures in a weakened cortex. Median survival after discovery of a pathologic fracture through an osseous metastasis is only about 18 months (combined for all primary sites).
CASE 2.21 CLINICAL HISTORY
A 10-year-old girl with left arm pain.

FIGURE 2.21A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree