Clinical Presentation
The patient is a 70-year-old woman with a 1-year history of left hip and groin pain. There was no antecedent trauma. She underwent injection therapy, particularly epidurals, for which she stated she would have anywhere from 6 weeks to up to 4 months relief. She states that her pain is most significant when walking. The pain becomes intense after walking approximately 50 feet or standing longer than 15 minutes. The pain is present but decreases when sitting, particularly in the reclined position with the left leg elevated. She is rarely pain free, only when lying supine and remaining motionless. Her pain is described as both aching and sharp with activities.
Imaging Presentation
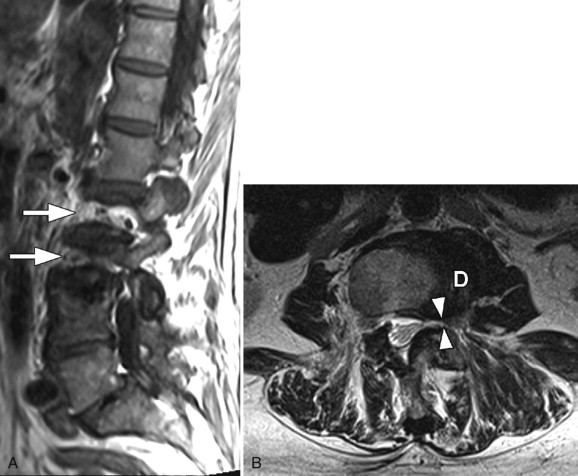
Sagittal T1-weighted midline image does not demonstrate the L2 and L3 vertebral bodies because they are not in the midsagittal plane secondary to scoliosis. The axial T2-weighted image reveals moderate narrowing of the left neural foramen ( Fig. 66-1 ) .
Imaging Presentation
Sagittal T1-weighted midline image does not demonstrate the L2 and L3 vertebral bodies because they are not in the midsagittal plane secondary to scoliosis. The axial T2-weighted image reveals moderate narrowing of the left neural foramen ( Fig. 66-1 ) .
Discussion
Scoliosis, historically, has been defined as an abnormal coronal curvature of the spine of 10 degrees or more. However, through a better understanding of biomechanics, spinal anatomy, and imaging techniques, it has been discovered that scoliosis is not merely coronal imbalance. Scoliosis is a three-dimensional rotational deformity that affects the coronal balance, sagittal balance, and axial rotation of the spine.
There are many different types of scoliosis. They can be classified by curve location, age at onset, and curve type. Typically, they are classified by their etiology—congenital, idiopathic—and their part in other diseases and syndromes—traumatic or degenerative. Each type has its own natural history, methods of treatment, and prognosis.
Curve location is defined by its apex. The apex of a curve is the most lateral vertebral body on frontal radiographs. A scoliosis is considered cervical if its apex is between C2-C6, cervicothoracic if between C7-T1, thoracic if between T2-T11, thoracolumbar if between T12-L1, lumbar if between L2-L4, or lumbosacral if at L5 or below.
Scoliosis can be defined by age at presentation. Type 1 (infantile) is from 0 to 3 years of age, type 2 (juvenile) is from 4 to 10 years of age, type 3 (adolescent) is from 11 to 17 years of age, and type 4 (adult) is 18 years of age or older.
Curve types are defined as either primary, those that first develop, or secondary, those that develop as a “means to balance the head and trunk over the pelvis, not only in the frontal but also in the sagittal plane.”
Congenital scoliosis is the most frequent congenital spinal deformity. The curvature is not present at birth. The vertebral anomalies are present at birth, but the spinal deformity does not reveal itself until later childhood after the spine grows. Congenital scoliosis is commonly associated with cardiac and/or urologic abnormalities. Congenital scoliosis progresses in 75% of cases.
Idiopathic scoliosis is the most common type of scoliosis in skeletally immature patients. Idiopathic scoliosis can be classified as infantile, juvenile, or adolescent forms. The infantile and juvenile forms of idiopathic scoliosis are less prevalent than the adolescent form. The prevalence of adolescent scoliosis is 2% to 3%. Males are more affected than females in the infantile form. This reverses in the juvenile form, where there is a female preponderance, although this depends on curve magnitude. For curves closer to 10 degrees, there is no significant gender difference with juvenile scoliosis. With curves greater than 30 degrees, the ratio of female : male is 10:1. There appears to be a genetic predisposition to the development of scoliosis. Monozygotic twin studies show an increased prevalence of scoliosis as opposed to dizygotic twins, and is also greater in family members with scoliosis as compared with the general population. Idiopathic scoliosis appears to be due to a failure of adequate control of spinal growth with differential growth between left and right sides of the spine and/or differential growth between the anterior and posterior aspects of the spine. The infantile form of idiopathic scoliosis rarely progresses. The juvenile form progresses in 70% of cases with the potential for cardiac and pulmonary compromise secondary to trunk deformity. Only 2% of adolescents have scoliosis (curve of 10 degrees), but only 5% of these have a progression of their curve beyond 30 degrees.
Scoliosis is associated with other diseases and syndromes. Cerebral palsy and muscular dystrophy are associated with scoliosis. Scoliosis is seen in nearly 10% of patients with trisomy 21 . Scoliosis is also associated with Chiari malformations, syrinx, spinal tumors, and generalized diseases and syndromes such as Marfan syndrome, neurofibromatosis , and rheumatoid disease .
Traumatic scoliosis is a compensatory mechanism to fractures and/or dislocations or to soft tissue injuries such as burns.
Adult scoliosis can be divided into type 1 adult scoliosis, which is degenerative; type 2 idiopathic adolescent scoliosis, which progresses into adulthood; and type 3 secondary adult scoliosis, which may be due to a leg length discrepancy, hip pathology, or may be secondary to a metabolic bone disease such as osteoporosis combined with asymmetric arthritic disease. Adult idiopathic scoliosis generally does not progress if curves are less than 30 degrees. Curves that are between 30 and 50 degrees at skeletal maturity tend to progress an average of 10 to 15 degrees over their lifetime. Curves between 50 and 75 degrees progress at an average of 1 degree per year. Degenerative scoliosis usually develops after the age of 50 and is typically associated with disc degeneration, facet arthritis, thickening/hypertrophy of the ligamentum flava, loss of lumbar lordosis, and lateral listhesis. Degenerative scoliosis can lead to neurogenic claudication, radicular pain, and back pain.
Imaging Features
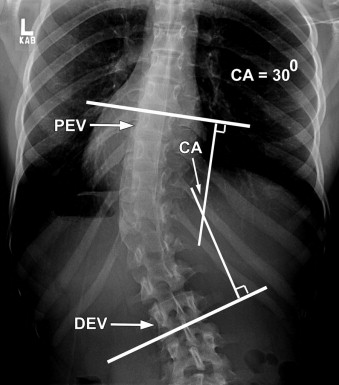
Computed tomography (CT) and magnetic resonance imaging (MRI) can be used to demonstrate the effects of scoliosis in relation to the spinal canal, spinal cord, and neural foramen. CT can be used to evaluate more subtle bone abnormalities such as hemivertebrae and butterfly vertebrae and is particularly useful in computer-assisted placement of pedicle screws because there is a much greater difficulty and thus a greater morbidity with “blind” screw placement secondary to the three-dimensional abnormalities of scoliosis. By far, the most useful imaging technique in the evaluation of scoliosis is plain film radiographs. Many advocate upright and supine frontal and lateral long-cassette (36-inch) radiographs that include the occiput to the femoral heads ( Fig. 66-2 ) . The greatest magnitude of a patient’s spinal deformity is best seen on the weight-bearing upright images. By convention, scoliosis radiographs are evaluated as if the physician were looking at the patient from the back (the left side of the radiograph is the left side of the patient), and the lateral view is with the physician looking at the patient’s right side (patient looking to the right). Four measurements are typically calculated from the plain radiographs; the Cobb angle, the apical vertebral translation, the coronal balance, and the sagittal balance.
- 1
The Cobb angle measures the angular magnitude of a spinal deformity and is calculated by using the end vertebrae (the vertebrae that are maximally tilted at each end of the curve). Lines are drawn parallel to the superior endplate of the cranial end vertebrae and parallel to the inferior endplate of the caudal end vertebrae; 90-degree perpendicular lines are then drawn for each of these lines so that they intersect. The angle created by these two intersecting lines is the Cobb angle ( Fig. 66-3 ) . A Cobb angle measurement is obtained for each curve present. It is very important to make sure that positioning of the patient is consistent, because measurements have been shown to differ by more than 20% secondary to positioning variances.